![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
50 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Describe the 2nd stage of lyme disease
|

Stage 2:
• NEURO findings, most commonly BELL'S PALSY (but bilateral) • Cardiac findings, commonly fluctuating AVB that may present as SYNCOPY and may require temporary pacing • Develops 4 wks after bite • Hematogenous dissemination of spirochetes |
|
|
|
Describe the clinical findings in tick paralysis.
Recovery? Cause? |
• ASCENDING flaccid paralysis
• LOSS of DTRs • Absence of bulbar findings • Complete recovery seen within 48 hrs of tick removal Caused by a NEUROTOXIN from the DERMACENTOR tick. This is NOT an infectious dz! |
|
|
|
Describe the epidemiology and clinical findings in Reiter's syndrome
|
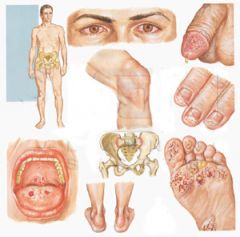
Epidemiology:
• Males 15 - 35 yo • HLA-B27 Clinical: • Appears 2-6 wks after CHLAMYDIAL or dysentery infx (SHIGELLA, Salmonella, Camp, Yersinia) Classic Triad of: • Arthritis (wt-bearing jts of lower extremities; 'LOVER'S HEEL') • Conjunctivitis • Urethritis Also seen: • Painful oral and penile ulcers (balanitis circinata) • SAUSAGE DIGITS • Keratoderma blennorrhagia (waxy plaques on palms and soles) |
|
|
|
Describe the epidemiology and clinical picture of ankylosing spondylitis.
Extra-articular manifestations? |

Epidemiology:
• MALE > Female • Age < 40 Clinical: • Sacroiliitis that develops into BAMBOO SPINE • MORNING STIFFNESS that improves with exercise • UVEITIS -- the most common extra-articular manifestation • Plantar fasciitis • Achilles tendinitis |
|
|
|
Describe the etiology and sx of toxic shock syndrome
|
Etiology:
• Staph TSS toxin-1, or • Strep pyogenes (GABHS) exotoxins A and B Sx: • Diffuse DESQUAMATING SUNBURN-like rash • High fever • HoTN • Leads to multisystem organ failure |
|
|
|
Describe the first stage of Lyme disease
|

Stage 1:
Erythema (chronicum) migrans rash: • Seen 1 wk to one month after tick bite at the site of the bite • 'Bullseye lesion'; Bright red border with central clearing • Quickly multiplies and spreads to thigh, groin and axilla Non-specific viral sxs |
|
|
|
Describe the sometimes fatal syndrome associated with allopurinol. Which patients are most at risk?
|
Syndrome of:
• Exfoliative rash • Fever • Hepatitis At-risk patients: • Preexisting renal insufficiency • Taking diuretics |
|
|
|
Discuss babesiosis:
• Cause • Mechanism • Sx • Labs • Tx |
Caused by a PROTOZOAN parasite from the IXODES tick ('Babe-y (I)') that infects ERYTHROCYTES.
Sx -- malaria-like: • HEMOLYTIC ANEMIA • Intermitent SWEATS • HA • Fever • Myalgia • SPLENOMEGALY May cause OVERWHELMING SEPSIS in asplenic pts Labs: • Pancytopenia • Elevated LFTs Tx: • CLINDA + QUINIDINE |
|
|
|
Discuss Colorado tick fever:
• Cause • Sx • Labs • Duration of sx |
A tick-borne illness caused by a self-limiting RNA VIRUS
Sx: • BIPHASIC FEVER pattern ('SADDLEBACK' fever curve). Each fever phase lasts 2-4 days. • Severe retro-orbital HA • Photophobia • Back pain Labs -- DECREASED WBC Duration -- entire course of illness usually lasts 2 weeks |
|
|
|
Discuss Relapsing Fever.
• Organism • Sx • Labs • Diagnostic test • Tx |
Cause ('R&B'):
• TICK-borne illness caused by Borrelia SPIROCHETE (different from the Lyme Borrelia) • Reservoir -- wild Rodents Sx: • Fever, chills • Myalgia, arthralgia Labs: • Decreased platelets • Elevated WBC • Elevated ESR Test -- Giemsa stain Tx: • Doxy,or • E-mycin |
|
|
|
How does the lupus anticoagulant and antiphospholipid antibody affect PTT and clotting?
|
These PROLONG PTT, but
are paradoxically associated with INCREASED CLOTTING --> • Recurrent CVAs • Recurrent PEs |
|
|
|
Severe disturbances of which electrolytes can cause severe, reversible MYOPATHY?
Rate of onset? Findings? |
HYPOkalemia (< 2)
HYPERkalemia (> 7) HYPERmagnesemia HYPERcalcemia HYPOphosphatemia ACUTE rate of onset Findings: • FLACCID paralysis • DTR usually PRESERVED |
|
|
|
State the American College of Rheumatology diagnostic criteria for SLE
|
Need 4 or more criteria during any interval period:
Dermatology: • Malar or discoid rash • Photosensitivity • Oral ulcers Arthritis, SYMMETRIC ('Hitch-hiker's thumb') Renal -- persistent PROTEINURIA CV: • PERICARDITIS • Pleuritis Neuro: • Seizures • Psychosis Immune/ Heme: • Hemolytic anemia • Leukopenia • Lymphopenia • Thrombocytopenia • ANA • Anti-DNA Ab • Anti-Smith Ab • Antiphospholipid Ab • Lupus anticoagulant |
SOAP BRAIN MD
S=serositis O=oral ulcers A=arthritis P=photosensitivity, pulmonary fibrosis B=blood cells R=renal, Raynauds A=ANA I=immunologic (anti-Sm, anti-dsDNA) N=neuropsych M=malar rash D=discoid rash |
|
|
State the causative organism for each of the following tick-borne diseases:
• Babesiosis • Colorado tick fever • Ehrlichiosis • Relapsing fever • Tick paralysis |
Babesiosis -- Protozoan PARASITE from the Ixodes tick ['Baby (y-->I)']
Colorado Tick Fever -- RNA virus Ehrlichiosis -- Gram-neg intracellular BACTERIA Relapsing Fever -- Borrelia SPIROCHETES from Ornithodoros ticks ('R&B') Tick paralysis -- NeuroTOXIN from the DERMACENTOR tick |
|
|
|
State the epidemiology of SLE.
What is the classic triad of symptoms at initial presentation? |
• Female > male (11:1)
• Childbearing years • BLACK > white Presentation triad: A woman of childbearing age with: • Fever • Joint pain • Malar or butterfly rash |
|
|
|
State the physical exam findings of the hand in RA
|

• MCP and PIP affected
• DIP is spared • Subluxation with ulnar deviation of MCPs • Swan neck deformity • Boutoniere's deformity |
|
|
|
What are the diagnostic criteria for Reflex Sypathetic Dystrophy (aka Complex Regional Pain Syndrome)?
|
• Allodynia
• Burning pain • Edema • Color changes • Hair growth changes • Sweating changes • Temperature changes • Demineralization on xray |
|
|
|
What are the GI complaints seen in SLE?
|
• ORAL ulcerations -- usually accompany dz flares
• ESOPHAGEAL dysmotility • CRAMPY abdominal pain |
|
|
|
What are the major and minor Jones criteria for rheumatic fever?
|
'SPEC FEAR'
Major: • Sub-Q nodules • Polyarthritis (symmetric) • Erythema marginatum • Carditis • Chorea Minor: • Fever • Elevated ESR, CSR • Arthralgia • PROLONGED PR + SUPPORTING EVIDENCE of prior group A strep: • Elevated/increasing strep Ab titer • Positive rapid strep or throat cx • Recent scarlet fever |
|
|
|
What are the relative contraindications to arthrocentesis?
|
• Bleeding diasthesis
• Coagulation therapy • Infection over site • BACTEREMIA |
|
|
|
What common medication often exacerbates SLE symptoms?
|
Oral contraceptives
SLE pts should use only LOW-ESTROGEN OCPs |
|
|
|
What conditions are associated w/ MIGRATORY arthritis?
|
• HSP
• GC • Sepsis • Mycoplasma pneumonia • Lyme Dz • Rheumatic fever • Bacterial endocarditis ('He Gently SMyLed Right Back') |
|
|
|
What drugs are used in the management of SLE?
|
Oral steroids
ANTIMALARIAL drugs control the cutaneous and musculoskeletal manifestations of SLE: • Hydroxychloroquine • Chloroquine Immunosuppressive agents for tx failure/ severe disease |
|
|
|
What is the cause of Ehrlichiosis?
|
A tick-borne infection caused by Gram-negative intracellular BACTERIA
|
|
|
|
What is the differential dx of ASYMMETRIC arthritis?
|
Asymmetric AND Symmetric:
• GC • Lyme • Reiter's Asymmetric only: • Henoch Schonlein Purpura |
|
|
|
What is the pathognomonic lab finding in a pt with Babesiosis?
Other lab findings? |
Pathognomonic:
• 'MALTESE CROSS' formation -- intra-erythrocytic PARASITES on GIEMSA-stained blood smear Labs: • PANCYTOPENIA • Elevated LFTs |
|
|
|
What is the recommended abx and duration of treatment for EARLY Lyme disease?
Pregnant/ Lactating/ Children? Severe disease? |
Early Dz:
• Doxy 100 bid, or • Amoxicillin 500 qid, or • Cefuroxime 500 bid. • Tx is for 20 - 30 days Pregnant/ Lactating/ Kids < 8 yo: • Amoxicillin Severe Dz: • PCN IV 20 million units, or • Rocephin 2 g qd |
|
|
|
What is the relative occurance of Neisseria gonorhoeae in mono- vs poly-articular arthritis?
|
Mono -- only 20% of cases
Poly -- much more common |
|
|
|
What is the role of abx prophylaxis of Lyme disease in patients with tick bites?
|
Prophylaxis is not recommended after tick bites, even in endemic areas, except perhaps:
• Pregnant patients • Prolonged tick attachment in small children |
|
|
|
What is the rule when evaluating ANY patient with monoarticular arthritis?
|
Monoarticular arthitis is SEPTIC arthritis until proven otherwise
|
|
|
|
What is the sensitivity of ESR and CRP in the diagnosis of osteomyelitis?
|
ESR -- 90%
CRP -- greater than 90% |
|
|
|
What is the treatment of Erythema Nodosum?
|

• High dose ASA or NSAIDS
• Supersaturated potassium iodide soln (rarely) 'Nodosum -- NSAIDS' |
|
|
|
What is the treatment of Rocky Mountain Spotted Fever?
Pregnant? When should treatment begin? |
Doxy
Pregnant -- Chloramphenicol Most classes of abx are effective Treatment should begin IMMEDIATELY upon suspecting RMSF; very HIGH FATALITY RATE in untreated cases |
|
|
|
What is the typical presentation of N gonorrhoeae septic arthritis?
What is its prevalence? |
N gonorrhoeae septic arthritis most commonly presents as POLYARTICULAR arthritis
Accounts for 20% of all monoarticular arthritis Accounts for 'a larger proportion' of polyarticular arthritis |
|
|
|
What is transient (toxic) synovitis?
• Epidemiology? • Presentation? • Joint fluid analysis? |
NON-SPECIFIC INFLAMMATION of the synovium of the hip, often FOLLOWING a VIRAL ILLNESS
Epidemiology: • 18 mos - 12 yo (usually 5-6 yo) • MALE > female • The MOST COMMON cause of hip pain in children Presentation: • Limp or inability to bear weight • Hip, knee or thigh pain Joint fluid: • 5000 - 15000 WBC • PMN < 25% Note: this condition a DIAGNOSIS OF EXCLUSION. Must first r/o septic joint. |
|
|
|
What medical conditions should readily come to mind in a patient presenting with a rash to the PALMS and SOLES?
|
• Kowasaki Dz
• Erythema multiforme • Rocky Mountain Spotted Fever • Neisseria gonorrhoeae • 2° syphilis • Bacterial endocarditis |
|
|
|
What non-immunosuppressive drugs are effective in treating the cutaneous and musculoskeletal manifestations of SLE?
Side effects? |
• Chloroquine
• Hydroxychloroquine Side effects: • Retinopathy -- irreversible • Corneal deposits -- reversible |
|
|
|
What percent of blood cultures and gram stains are positive in patients with septic arthritis?
|
50%
GS > Cx |
|
|
|
What sx is almost pathognomic for Brucellosis?
|
MALODOROUS PERSPIRATION
|
|
|
|
What test is the most sensitive, and what is the most specific, for diagnosing SLE?
|
Most sensitive -- ANA
Most specific -- anti-Smith Ab ('ANA Nicole Smith') |
|
|
|
What test(s) are used to dx Rocky Mountain Spotted Fever?
|
• Skin bx
• Immunofluorescent staining |
|
|
|
Which disease is associated with erythema marginatum, and which is associated with erythema (chronicum) migrans?
|
Erythema marginatum -- Rheumatic Fever (Major Jones criteria)
Erythema (chronicum) migrans -- Lyme Dz |
|
|
|
Which joints are most commonly affected in psoriatic arthritis?
Behcet's Dz? |
Psoriatic arthritis -- PIPs and DIPs
Behcet's -- Ankles and knees |
|
|
|
Which meds are associated with precipitation of SLE?
|
• Hydralazine
• Procainamide • Isoniazid NOTE: OCPs EXACERBATE established SLE |
|
|
|
Describe the symptomatology and RASH of Rocky Mountain Spotted Fever.
What does the CBC show? |

Rash:
• Initially MACULAR --> • Progresses to PETICHIAL • Begins on the WRISTS, ANKLES, palms and soles • Spreads CENTRALLY Other sx: • HIGH FEVER • Myalgias (especially CALF) • HA • Vomiting • Malaise CBC -- NORMAL |
|
|
|
What are the major complications of untreated Rocky Mountain Spotted Fever?
Mortality rate? |
• Shock
• DIC • CHF • ARDS Mortality rate -- 3-6% |
|
|
|
State in order the joints typically affected by septic arthritis
|
1) knee (40-50%)
2) hip (13%) 3) shoulder (10-15%) 4) fingers, wrist, elbow, ankle (3-8%) |
|
|
|
State the relationship between joint fluid viscosity and joint infection.
What lab test can evaluate viscosity? |
Viscosity decreases with infection
Drip test -- Normal jt fluid will form a string approx 5 - 10 cm long when dripped from a syringe. A decrease in this length indicates reduced viscosity and joint infection. |
|
|
|
While Staph aureus is the most common cause of septic arthritis overall, state the organism responsible for septic arthritis in the following groups of people:
• Infants < 6 mos • 6 - 24 months • IVDU |
< 6 months:
• E coli • GBS 6 - 24 months: • Kingella kingae • (H flu) IVDU: • Staph aureus • Pseudomonas |
|
|
|
Describe the 3rd stage of Lyme disease.
|
Stage 3:
• Polyarthritis, migratory • Seen in large joints, particularly the KNEES • Large effusions common • Pts have minimal joint pain • Seen in 50 - 60% of pts • Occurs w/in 6 months |
|

