![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
87 Cards in this Set
- Front
- Back
|
How can you treat Shigella Intoxication?
|
GASTOINTESTINAL
Fluids, electrolyte replacement, Antibiotics (careful -- some promote shiga toxin release) SYSTEMIC Antibiotics, Antibody Therapy |
|
|
What major disease does Shigella cause?
|
Bacillary Dystentary (most common in developing countries)
|
|
|
Which disease does Mead et al. claim to have a significant number of cases, when in reality, current data shows the genus to have far less of an effect?
|
Yersinia
|
|
|
What are characteristics of Shigella?
|
Gm -, nonsporeforming facultative anaerobe
Mesophile (7-46C) Catalase + Lactose - No gas production from sugar fermentation Related to Escherichia Stress resistant to acid, salt and freezing |
|
|
What is the major difference between Escherichia and Shigella
|
E is lactose +
S is lactose - |
|
|
What are two most common species of Shigella in outbreaks?
|
Shigella flexneri, Shigella sonnei
|
|
|
What are the virulence factors of Shigella?
|
Shiga toxin (stx)
Enterotoxins (ShET1 & ShET2) Plasmid coated invasive proteins Invades cells of large intestine |
|
|
What is the major natural reservoir for Shigella
|
Humans
|
|
|
What is the defining symptom for shigella intoxication?
|
Diarrhea with blood, mucous, and or pus (DYSENTARY)
|
|
|
What are complications of Shigella intoxication?
|
HUS (Children)
Severe Dehydration Intestinal Perforation Septicemia Seizures |
|
|
How can Shigella be controlled in a plant environment?
|
No contact with human feces
Heating, Sanitizing GMPs - personal hygeine |
|
|
Which is considered an emerging pathogen? Shigella or Yersinia?
|
Yersinia: first case was 1950s
Not very common to have outbreaks |
|
|
What are characterisics of Yersinia?
|
Gm-, Psychrotroph, Infective dose is ~1000 cells
|
|
|
What is the most common species of Yersinia in foodbourne outbreaks?
|
Yersinia enterocolitica
|
|
|
How is Yersina enterocolitica commonly misdiagnosed?
|
misdiagnosed as appendicitis (bacteria causes severe abdominal pain). Syndrome is called pseudoapendicitis
|
|
|
What are the difference between Yersina and Shigella in terms of incubation time and disease duration?
|
Shigella: IT: 1-3d DD: 5-6d
Yersinia: IT: 24-30h DD: 3d-3w |
|
|
Who is suceptible to Yersinia and what are complications
|
Children under 5, Causes autoimmune conditions such as reactive arthritis and thyroid diseases
|
|
|
In what foods and animals can Yersinia be found?
|
Found in livestock and wild animals (Biovar 4 in pigs, 1B in rats).
Human Foods: Pork, beef, lamb, poultry, raw milk |
|
|
What are the virulence factors of Yersinia? What is one special characterisitc about Yersinia virulence?
|
Invasin protein, AIL (Attachment and Invasion Locus), Heat-stable enterotoxins, lipopolysaccharide.
Yersinia virulence is enhanced when it grows below 30C. |
|
|
What is the most virulent Vibrio strain?
|
Vibrio vulnificus (most deadly foodbourne pathogen)
|
|
|
Name the main strains of Vibrio relevant to foodbourne disease and whether they cause an intoxication or infection or toxicoinfection.
|
Vibrio parahemolyticus - infection
V. vulnificus - Infection V. cholera - toxicoinfection V. mimicus - toxicoinfection |
|
|
What are characteristics of the Vibrio genus?
|
Gm - facultative anaerobe, curved rods, Catalase positive, mesophilic (grows from 5-42C), halophilic (requires NaCl to grow, can survive in 3-5% solutions), Sensitive to pH below 5, most lactose negative (except V. parahemolyticus)
|
|
|
Describe characterisitcs of Vibrio parahemolyticus infection
|
Gastroenteritis (Diarrhea, nausea, vomiting, chills, fever, abdominal cramps)
Self limiting Human studies confirmed an infectious dose of 10^5 CFU Incubation time = 3-76h |
|
|
Describe characteristics of V. vulificus infection
|
V.v affects organs, it is systemic. Symptoms include Primary septicemia, Fever, Chills, Hypotension, Prostration (Phy or mental exhaustion)
Enteric (GI) symptoms are rare Incubation time is 7-40h Vulnificus is responsible for 90% of Vibrio related deaths in the US |
|
|
Who is suceptible to vulnificus?
|
Men >50 yrs old that have liver or blood disorders that cause high iron in the blood.
Organism needs iron to grow, and is sex specific because estrogen protects against the toxin for women |
|
|
What are the defining characterisitcs between the Vibrio FBD species?
|
V.vulnificus lacks gastrointestinal symptoms
V. cholera is a toxicoinfection while vulnificus and parahemolyticus are infections |
|
|
What are characterisitics of V. cholera and what are the complications? What type of illness does it cause: toxicoinfection, infection, or intoxication?
|
toxicoinfection.
CHaracteristics: Infectious dose is 10^5 CFU Incubation time is 12h-5d Violent watery diarrhea with mucus (rice water) Dehydration Complications: Cholera gravis -- tachycardia and hypotension |
|
|
Which V. cholera strain is most prevalent?
|
O1. Other strains are O139(bengal) and El Tor
|
|
|
What are the virulence factors of V. parahemolyticus?
|
Heat stable hemolysin - Kanagawa positive strains K+
(hemolysin = K+ designation) |
|
|
What are virulence factors of V. vulnificus?
|
K Capsule is involved in Fe uptake (needs Fe to grow)
Lipopolysaccharide (cell wall) causes endotoxic shock |
|
|
What are virulence factors of V. cholera?
|
Cholera enterotoxin (CT). This molecule is a protein with A-B subunits.
|
|
|
What is the Cholera enterotoxins mechanism in the body? What does it end up causing?
|
1. Binds to a GM1 receptor
2. Internalizes in the endosome 3. Stimulates adenylate cyclase 4. Increases cAMP and leads to increased Cl- secretion and lack of NaCl adsorption 5. MASSIVE LOSS OF FLUIDS |
|
|
What is the main source of Vibrio genus bacteria?
|
Coastal and Estuarine Coastal Water
Population increases with water temperature Bacteria is especially concentrated in filter feeders i.e. mussels |
|
|
What are the top three foods in terms of Vibrio prevalence?
|
Raw Oysters, Imported Shrimp, and Finfish and Shellfish
|
|
|
Name several control methods to kill Vibrio bacteria
|
High pressure processing (does not ruin oyster meat), avoid eating raw oysters, Irradiation, Treatment and sanitation of water (Cholera)
|
|
|
What is the present controversy concerning the zero tolerance policy of Listeria monocytogenes?
|
-A representative test is not performed
-Listeria is present in many foods, eliminating it completely is very difficult -Some suggest that education is way to solve problem -Listeria monocytogenes infections have not substantially decreased, meaning the program is not exactly a success |
|
|
What types of foods are most likely to have Listeria m?
|
Beef and pork meat, Poultry, Smoked Fish
|
|
|
What are organism characterisitcs of Listeria?
|
Gm+, nonsporeforming, facultative anerobe, rod, fermentative (glucose --> lactate, acetate, and acetoin), psychrotroph 1-44C, does well without competition in food, halotolerant (can grow in concentrations up to 12%), can survive well in environment
|
|
|
What serotypes are responsible for 95% of Listeria monocytogenes cases?
|
1/2a, 1/2b, 4b (causes 30-50% of all cases)
|
|
|
What are disease characteristics of Listeria monocytogenes infection?
|
Gastroenteritis may be absent (mild symptoms)
Diarrhea, Slight Fever, Abdominal Cramps Systemic Infections (CNS) Septicemia, Meningitis (Inflammation of CNS-reason for lethality), Menigoencephalitis |
|
|
Describe the mechanism of Listeria monocytogenes infection
|
1. Bacteria enters into cell via Internalin (inlA, inlB)
2. Lysis of Vacuole and Intracellular Division (hly, plcA) 3. Actin Filament Nucleation and Tail formation/movement (actA) 4. Escape from Cell 6. Escape from double membrane , spread from cell to cell (plcB, mpl) |
|
|
Describe the Virulence Factors of Listeria monocytogenes
|
Positive Transcription Factor (prfA) - global regulator
Internalin (inlA) - internalization Phosphatidylnositol-specific phospholipase C (plcA) - hydrolyzes endosome membrane Listeriolysin O (hly) - lysis of endosome & beta-hemolysis Actin Polymerase (actA) - actin formation Phospholipase C (plcB) - cell to cell spread |
|
|
How is Listeria monocytogenes detected, and what are several principles?
|
It is tested based on its ability to hydrolyze esculin (produces characteristic black color on MOX and LEB media), hemolysis, rhamnose fermentation.
It is tolerant to: acriflavin, nalidixic acid, cycloheximide, LiCl, Colistin Sulfate, Moxalactam. AGARS USED: MOX, PALCAM, TSAYE, UVM1 Broth, TSA Blood Agar |
|
|
What are ways that are being used to control RTE Meats?
|
Producer: Mild thermal treatment in package, high pressure processing, sodium lactate, sodium diacetate
Consumer: Re-heating of product |
|
|
Describe the Bil Mar Listeria Outbreak. What did it highlight?
|
Part of Sara Lee, made Ball Park hot dogs, turkey franks and deli meats.
Outbreak in 1999, due to repair work on a refrigeration unit. The outbreak functioned to change the preception of risk with deli meat. |
|
|
Explain the role of proline and glycine betaine for Staphylococcus’ environmental survival
|
They are osmoprotectants. They high intracellular concentration lowers the water activity of the cells matching the external and protecting the cells.
|
|
|
2. If you were working at Chubby Chuck’s Chickery as a Quality Assurance microbiologist and you detected a total of 5 ng of SEB using a very sensitive ELISA test in a sample of 100 g of chicken salad produced a the day before. Would you recall the product? What would you do?
|
You probably would not want to recall the product since this concentration (0.05 ng/100 g) is significantly lower than the minimum LD50 reported (1 ng/g), but you would certainly would want to re-test and/or identify whether the product was contaminated and how you could prevent this from happening again.
|
|
|
What are the functions of potassium tellurite for Staphylococcus detection?
|
It is a differential (causes black colonies) and a selective (inhibits other microorganisms) agent.
|
|
|
Why are the Staphylococcus aureus enterotoxins so resistant to heat?
|
Because 1) they are very small protein, 2) are monomeric or single-unit, 3) have closed structure, and 4) have low number of α-helices
Two of these would have earned 2 points |
|
|
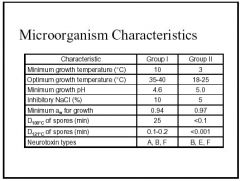
What are characteristics of Cloistridium botulinum
|
Anaerobic, Gm+, Endospore forming rod, Spores can remain dormant for up to 30yrs, Spores are very resistant to heat and UV light, Major types are:
proteolytic (digestion of proteins by cellular enzymes) GROUP I non-proteolytic, GROUP II Seven types (A --> G) based on toxin type (ABE are human) |
|
|
Name characteristics of Group I and Group II C. botulinum micro-organisms
|
Above
|
|
|
What are the four types of C. botulism sicknesses?
|
Foodbourne - intoxication
Infant botulism - toxicoinfection Wound botulism - toxicoinfection Inhaled botulism - biological weapon |
|
|
What are the classic symptoms of C. botulism?
What are the clinial features of the disease? What if infants are affected? What are their signs? |
Double Vision, Muscle Weakness, Drooping Eyelids, Slurred Speech, Difficulty Swallowing
Blurry vision, muscle paralysis, respiratory failure, urinary retention, orthostasis, nausea, diarrhea, and dry mouth Weak cry, poor feeding, constipation, poor muscle tone |
|
|
What are disease characteristics of Botulism
|
High mortality rate (<10%)
Incubation period: Foodbourne:6h-8d Wound: 4d-14d Inhalation: 24-36h |
|
|
How is botulism treated?
|
Supportive care including:
Mechanical Ventilation, Parenteral nutrition, Prevention of 2˚ Infections, Body Positioning Passive Immunization (antitoxin): Halts paralysis, IMMEDIATELY administer, Equine Antitoxin used for ABE strains Elimination: Induced Vomiting High enemas |
|
|
How is the C. botulism bacteria and toxin detected in a lab setting?
|
Collection of stool or blood
Mouse bioassay ELISA test |
|
|
How is C. botulinum controlled in foods?
|
Temperature (Refrigerated Storage(<10C), Thermal inactivation, Cooking)
pH (below 4.6 inhibits all growth) Aw (NaCl added to lower Aw. ~10% for GpI, 5% for GpII) Redox Potential (Pressurized CO2 is lethal to C. bot) Added Preservatives (Nitrite is main pres. added - reacts with Iron-Sulpher proteins/Liquid smoke added to fish also inhibits) Competing Microorganisms (using competitive organisms has significant effect - Lactobacillus) |
|
|
Describe the mechanisms of pathogenicity for C. botulinum
|
1. Toxin enters bloodstream via mucosal surface or wound
2. Binds to peripheral cholinergic nerve endings 3. Inhibits release of acetylcholine, preventing muscle contraction 4. Symmetrical descending paralysis occurs beginning with cranial nerves and progressing downward 5. Death can result from obstruction of respiratory tract or paralysis of resp. muscles. 6. 2˚ complications are prolonged ventilation support and intensive care |
|
|
What are the virulence factors of C. botulinum?
How does botox work? Where are the toxin genes found? |
Botox:
Water soluble large protein. Protein is cleaved by an enzyme close to N-terminus which converts it into an active toxin, leaving a heavy and light chain linked by a disulfide bond. Heavy - 100kDa Light - 50kDa F(X) of Protein: Blocks release of acetylcholine from synaptic vesicles at nerve terminals causing the flaccid paralysis. 10^-9 Ounce is Toxic Protein is cleaved by an enzyme close to N-terminus which converts it into an active toxin ABE & F: Chromosome C1 & D: Encoded in bacteriophages G: located in a plasmid |
|
|
What are the most common foods where Botulism has been found?
|
HOME canned goods (low acid foods)
Honey (infants) Crash injuries, injection drug use exposed to soil |
|
|
Why does C. perfingens have the largest number of cases per outbreak, on average?
|
Since it causes a mild disease, only the largest outbreaks are reported, which are usually in institutional settings because of the practice of preparing food in advance.
|
|
|
What are characteristics of Cloistridium perfringens?
|
Gm+, anaerobic endospore forming, encapsulated, non-motile rod
Mesophile Fastest growing pathogen with G=7min (45C) Grows at pH of 5.5-8 Spores are thermally resistant Heterofermentive - ferments rapidly causing production of LOTS of gas (CO2, H2S, H2) BIG FARTS Four types based on toxin production: ABCDE |
|
|
Why are C. perfingens toxicoinfections usually mild and self limiting?
|
1. Diarrhea flushes unbound C. perfingens toxin-bound cells out of the small intestine
2. Toxin affects villus cells of intestine, which are the oldest cells and are rapidly replaced in healthy individuals |
|
|
What are the disease characterisitcs of C. perfringens?
|
Toxicoinfection
EXPLOSIVE diarrhea and abdominal cramps Incubation time of 8-16h Self limiting within a day Infectious dose 10^6 CFU |
|
|
How does C. perfringens modify its environment to promote growth?
|
If the redox potential is low enough to intiate growth, then C. perfringens modifies the environment by producing ferredoxin, a reducing molecule.
|
|
|
What are virulence factors of C. perfringens?
|
The cpe gene encodes the enterotoxin CPE, produced by type A strains, it is chromosomally located in toxicoinfectious isolates found in food.
Other toxins are encoded in the plasmid. CPE is heat sensitive, the cpe gene is thought to be responsible for this |
|
|
Describe the pathogenesis of C. perfringens
|
1. cells germinate in food
2. vegetative cells grow in food 3. food is ingested 4. cells continue to grow in intestine 5. synthesis of CPE enterotoxin and sporulation start when reaching stationary phase 6. CPE accumulates as inclusion bodies (inside cells) 7. When mother cell lyses, CPE is released |
|
|
Where is C. perfringens found?
|
High concentrations in soil
Found in temperature abused meat and poultry containing dishes |
|
|
Which is more common: C. perfringens or B. cereus?
|
C. perfringens by a long shot (3rd most common FB disease)
B. cereus causes only ~27000 cases annually |
|
|
Describe characteristics of Bacillus
|
Gm+, spore forming aerobic rod, mesophilic (most)
|
|
|
There are two distinct types of B. cereus diseases, what are they and what are their disease characteristics?
|
EMETIC (VOMITING)
intoxication, vomiting and nausea, 10^5 CFU infectious dose, 0.5-5h incubation, most common in Japan & UK, toxin is cyclic peptide (1.2kDa) which is heat and pH resistant, illness lasts 6-24h DIARRHEIC toxicoinfection, toxin produced in small intestine, watery diarrhea, infectious dose 10^5 CFU, 8-16h incubation time, most common in US & EU, toxin is an enterotoxin (24kDa), illness lasts about 6-24h |
|
|
What are virulence factors of B. cereus?
|
Emetic toxin: (cereulide)-enzymatically synthesized peptide
Enterotoxin: three component hemolysin (Hbl) causes diarrhea, transcribed from one operon (hbl) |
|
|
What are virulence factors for B. anthracis?
|
Two plasmids cause illness together: pX01 and pX02
|
|
|
Why is B. anthracis ideal as a bioterrorism agent?
What makes C. botulinum toxin an even better bt agent? |
Because it is highly lethal and infectious, resistant to environmental factors, inexpensive and easy to produce, can be trasmitted via air, water or food.
Botox is an even better BT agent because it takes as little as 1g to kill 1 million people and is easily cultivated and aerosolized. The illness would cause symptoms that would overwhelm the health care system. |
|
|
What is spoilage?
|
A food is spoiled if is composed of filthy putrid or decomposed substances
|
|
|
Name two aciduric, thermophilic, aerobic and facultative anaerobic bacteria associated with spoilage
|
Aerobes:
Pseudomonas, Moraxella Facultative Anerobes: Lactobacillus, Brocontrix Thermoduric: Bacillus, Cloistridium Aciduric: Lactobacillus, Pediococcus |
|
|
What is the order of preference for bacteria involved in microbiall spoilage
|
carbos-->aminoacids--->proteins
|
|
|
What are byproducts of aerobic respiration, fermentation (Energy production)
|
Aerobic: Co2
Fermentation: Lactic acid, acetic acid, ethanol |
|
|
What are byproducts due to protein utilization aerobic decay and fermentation
|
Aerobic: Co2
Putrefaction/Fermentation: cadaverine, skatole, putrescine, histamine, keto acids |
|
|
What are the major differences in food characteristics of meat, processed meat, seafood, fruits and veggies, and beverages?
|
Raw Meat has no preservatives and high water content, highly perishable
Processed meat has preservatives, salts and additives that lower the aw and eliminate most bacteria. Typically they have low carbos (except mollusks) high protein and a high concentration of NonProtein Nitrogenous compounds, which function to increase degradation and spoilage. F & V have higher carbohydrate concentration and water and are acidic Beverages are the most acidic and also have high concentrations of carbohydrates |
|
|
What are the major associated spoilage organism for each food type in spoilage?
|
Fresh Meat: No dominant group. Pseudomonas (aerobe), Lactobacillus, Moraxella, Enterobacter, Cloistridium
RTE Meat: Gram + Rods: Lactobacillus, Weisella Seafood: Strict Aerobes: Pseudomonas, Moraxella, Acinetobacter F & V: No predominant group. Mostly molds and bacteria. Veggies: Penicillum, Aspergillus. Pseudomonas, Erwina, Cloistridium Fruits: Lactobacillus, Acetobacter. Penicillium, Aspergillus. Saccaromyces Bevs:No dominant, but mostly yeasts and molds, with a few bacteria. Soft Drink: Lactobacillus,. Saccharomyces, Candida Juice: Penicillium, Aspergillus. Lactobacillus fermentum. Same yeasts as SD. |
|
|
What are conditions for spoilage of each? How are they different?
|
ALL: Temps above freezing or 5C
FM: low oxygen delays spoilage RTEM: Long Storage, Open package/store SEAFOOD: low oxygen delays spoilage, exposure to outside environment promotes autolytic enzymes FV: Tissue wounds, senescence, high temperature, high oxygen |
|
|
What are spoilage types for each main group and what are detection methods?
|
FM: off odor, slime, myoglobin oxidation, souring, Fungal (white spots, whiskers)
RTEM: Greening (caused by H2O2 or H2s), Sliminess, Souring (TEST: Chemical: Measurement of greening, pH, LAB) SEAFOOD: Degradation of NPN by bacteria, Fishy odor, discoloration of gills & eyes, proteolysis (softening) FV: Softening, rotting, color changes Detection: ALL: Total Aerobic/Anaerobic count, pH Seafood: Chem measurement of NPN compounds, Sensory examination of eyes and gills FV: Sensory, refractive index, LAB RTEM: LAB |
|
|
What are differences in spoilage prevention in the main categories?
|
FM: Better slaughtering practices, carcass washing, modified atmosphere, freezing
RTEM: Treated spices, ingredients, AntiM ingredients, Packaging treatment SEAFOOD: Freezing FV: modified atmosphere, low temps |
|
|
What are the initial and byproducts of NPN degradation?
|
NPN converts various compounds of fish including histadine, taurine, TMAO to Histamine (scromboid poisoning), TMA, indole, NH3
|
|
|
How does myoglobin of FM degrade?
|
Exposure to oxygen causes oxidation of myoglobin resulting in a brown color of meat. CO will prevent the browning of meat.
|
|
|
What benefit does Nitrates have for spoilage. What compound ensures that the reaction goes the way it is supposed to? What negatives?
|
NO3 --> Notrosomyoglobin (NO+myoglobin) --> PINK COLOR
Positive is it keeps the color of the meat the same. Erythorbate favors this reaction and prevents reaction with amines. NEGATIVE: If reacts with amines, creates carcinogenic compounds |

