![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
105 Cards in this Set
- Front
- Back
|
What five factors are important for a successful pure tone audiiometric result?
|
*the patient
*the environment *test equipment *the examiner *test procedure |
|
|
What is it important to consider about the patient one is planning to test?
|
One needs to have an assessment of the patient and their capabilities and some opinion as to what type patient we're dealing with and what their capabilities are.
|
|
|
What type of environment is preferable for audiometric evaluation?
|
A sound treated room, with patient in double walled room to attenuate as much external noise as possible.
|
|
|
What should be your main concern with the testing equipment?
|
The calibration of the equipment.
|
|
|
What is important to know about the examiner performing the audiometric testing?
|
The examiner needs to be properly trained and knows proper protocol, and how to consider the factors, such as patient and environment and etc.
|
|
|
Why is it important to follow a specific test procedure?
|
Procedures have been researched thoroughly, and continually refined over time to ensure correct results.
|
|
|
What is the testing equipment called used to assess hearing?
|
Audiometer
|
|
|
What do the two large dials on an audiometer control?
|
1. Intensity of stimulus
2. Frequency of stimulus |
|
|
Why must the signal be atteuated on the audiometer?
|
Tone is sent through at maximum intensity. Must be squelched or attentuated to appropriate level.
|
|
|
If stimulus is delivered via earphones, it is delivered via ____ ________.
|
Air Conduction
|
|
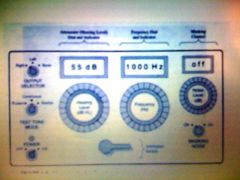
Using the professors picture, can you label the different parts.
|
Parts: attenuator, masking dial, where stimulus sent indicator, type of tone indicator, frequency dial, intensity dial
|
|
|
If stimulus sent via bone oscillator, it is sent via ____ __________.
|
Bone conduction
|
|
|
Why are there lower intensity limits for bone conduction than for air conduction?
|
It takes more power to drive the bone oscillator than wth air conduction outputs. The intense power can cause harmonic distortions causing the actual intensity to not match what you're trying to send (1500, vs. 1000 Hz for example). Also, tactile sensation so strong patient may think they hear, vs feel it.
|
|

Where should the center of earphones (with the grid) be placed
|
Directly over the ear canal
|
|
|
Earphones are called _____ _____ earphones and why is this important?
|
Supra aural. This means that they must go over the top of the ear and cover most of the auricle.
|
|
|
When earphones are color coded, what colors dilineate left from right pieces.
|
Red is right and blue is left.
|
|
|
Where can the bone oscillator be placed?
|
It can be placed on the left OR right side, OR forehead OR any other place on skull.
|
|
|
What are the Hz frequencies we test?
|
125, 250, 500, 1000, 2000, 4000 and 8000
|
|
|
When testing a patient, remember that their right side is on your _____ and their left side is on your _____.
|
left, right
|
|
|
Testing procedure protocol requires that you begin testing at what Hz?
|
1000 Hz
|
|
|
Why are 3000 Hz and 6000 Hz sometimes on an audiogram?
|
Sometimes an audiologist wants to know the threshold at these half octaves.
|
|
|
In testing the dB increments are in ____.
|
Tens (ex: 10 db, 20, db, 30 db and etc.)
|
|
|
What is the maximum intensity level we would ever test at?
|
110 dB
|
|
|
What symbol and colors would you use for marking the results for the right ear?
|
round and red (Note r and r for right)
|
|
|
What symbol and colors would you use for marking the results for the left ear?
|
Blue and X
|
|
|
Right ear bone conduction markings are:
|
< (it's open to your right)
|
|
|
Left ear bone conduction markings are:
|
> (it's open to your left)
|
|
|
Triangle icon means what?
|
Left ear masked when sound delivered to right. Note( r in triangle, to go with r in round and red for right ear markings!)
|
|
|
Box icon means what?
|
Right ear masked when sound delivered to left.
|
|
|
Define threshold
|
The level at which a stimulus,such as a pure tone, is barely perceptible. Usually clinical criteria demand that the level be just high enough for the subject to be aware of the sound at least 50 percent of the time it is presented.
|
|
|
What kind of instructions should be given a patient before beginning.
|
Tell them what to expect, and stay away from jargon. Tell them therre will be different tones at different loudness levels, NOT different frequencies at different intensity. Give them instructions on how to indicate when they hear the tone, and ask which ear is their better ear.
|
|
|
What information do most clinics follow that came from research published in 1959 by Carhart and Jerger?
|
Information regarding how to go about finding the threshold of a patient.
|
|
|
Carhart and Jergers technique is also known as the _________ ___________.
|
Ascending technique.
|
|
|
Describe the ascending technique of Carhart and Jerger.
|
Start at 1000, then test 2000, 4000, 8000. Retest 1000, then test 500, 250, 125.
|
|
|
Why do we retest at 1000 Hz in ascending technique?
|
1000 Hz is:
|
|
|
What is acceptable retest results at 1000 Hz.
|
It is acceptable to have results within 5 dB. If it's 10 dB or more, we need to figure out why.
|
|
|
How long should we present a tone to a patient?
|
One to two seconds.
|
|
|
At what decibel level should we present our first tone at 1000 Hz?
|
30 dB
|
|
|
Explain gross threshold search.
|
If there is no response at the 1st presentation at 30 dB, raise the tone to 50dB HL. If there is no response on up into the higher intensities, continue raising the tone in 10 dB steps until a response is obtained.
If there is a response at the 1st presentation at 30 dB, lower the tone in 10 dB steps until there is no response from the patient. |
|
|
Describe fine threshold search.
|
DOWN 10 dB - UP 5 dB
|
|
|
How do we find the pure tone average.
|
|
|
|
What frequency range is the speech frequency?
|
500 Hz to 2000 Hz
|
|
|
At what PTA range would you say there is no hearing loss?
|
-10 to 15 dB
|
|
|
At what PTA range would you say there is a slight hearing loss?
|
16 to 25 dB
|
|
|
At what PTA range would you say there is a mild hearing loss?
|
26 - 40 dB
|
|
|
At what PTA range would you say there is a moderate hearing loss?
|
41-55 dB
|
|
|
At what PTA range would you say there is a moderately severe hearing loss?
|
56-70 dB
|
|
|
At what PTA range would you say there is a severe hearing loss?
|
71-90 db
|
|
|
At what PTA range would you say there is a profound hearing loss?
|
91 dB +
|
|
|
Are testing procedures the same for BC as for AC? Why or why not?
|
They are essentially the same. The difference is that you've already have threshold via AC, which will inform where to start testing for BC conduction.
|
|
|
Why would you have a bone oscillator and a supra aural headphone on the patient at the same time?
|
You would have both, so that you could mask the ear you do not want to test.
|
|
|
Explain distortional bone conduction.
|
As we distort the bone and in a moment rarefy and compress it;that movement causes an up and down motion on the basilar membrane which is interpreted as sound in the same fashion as when they're stimulated by air conduction.
|
|
|
A ________ contribution to the total bone conduction experience is distortional bone conduction.
|
Main
|
|
|
A ________ contributor to the total bone conduction experience is osseous-tympanic.
|
Minor
|
|
|
Explain osseous-tympanic conduction.
|
The bone conduction causes vibration of the bones around the middle ear. This changes pressure in the ear canal creating air conduction (via bone conduction) that now comes in through tympanic membrane and increases perception of sound.
|
|
|
Explain inertia bone conduction.
|
As the ear is stimulated by bone conduction, the ossicular chain suspended in the middle ear lags behind the stimulation by bone conduction. Therefore, the lagging behind will cause the stapes to move and give compressions and rarefactions at the oval window.
|
|
|
Name the three contributors to bone conduction experience.
|
Distortional bone conduction, osseous-tympanic bone conduction, and inertia bone conduction.
|
|
|
What is the speech banana on an audiogram?
|
The area where the speech energy is found at converstional levels.
|
|
|
What would you expect if a person's hearing level drops below the speech banana?
|
They would be having problems with speech perception.
|
|
|
Which ear would you test first?
|
You would start with the patient's better ear. If they don't know, then the right ear is traditionally the one to start with.
|
|
|
What two frequencies would you most likely NOT see bone conduction testing on?
|
125 Hz and 8000 Hz
|
|
|
If there is an arrow pointing downward on the audiogram, what does it mean?
|
It means that we tested to the limit of our audiometer and were not able to get a response from the patient.
|
|
|
If you have a circle denoting test results showing a hearing loss, what other items should you be considering (two other circles with the three being a triangle)
|
Your other two circles should be anatomy and disorders. All three circles are interrelated.
|
|
|
Why would an audiogram of a person with normal air conduction hearing not be tested by bone conduction?
|
It would be foolish to test by bone conduction. If you get normal hearing, threre is normal bone conduction.as well.
|
|
|
What is an air bone gap?
|
A gap between air conduction and bone conduction.
|
|
|
ABG is ___ ______ _____.
|
Air bone gap
|
|
|
PTA is an acronym for what?
|
Pure tone average
|
|

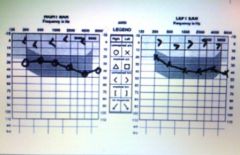
What type of hearing does this person have?
|
Normal hearing
|
|
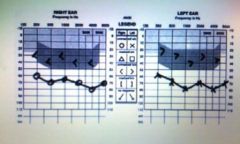
What type of hearing does this person have?
|
Bilateral conductive loss
|
|
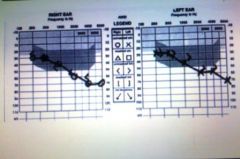
What type of hearing does this person have?
|
Bilateral mixed hearing loss
|
|
What type of hearing does this person have?
|
Bilateral sensorineural loss
|
|
What type of hearing does this person have?
|
Unilateral conductive loss
|
|
What type of hearing does this person have?
|
Unilateral sensorineural loss
|
|
Explain why the top portion is listed as a sensorial neural loss (vs. the bottom portion)
|
With the bone gap made up with via bone oscillation, you are seeing what the cochlea is truly able to hear. This makes the bottom portion reflective of what the bone conduction adds to the mix.
|
|
|
Explain the abbreviations TE and NTE
|
TE = the ear being tested
NTE = the ear that is the ear that is not being tested. |
|
|
Explain the concept of cross hearing.
|
This is when during audiometric testing the sound being presented to the poorer ear, travels and is heard by the better ear.
|
|
|
If when presenting the stimulus (sounds) via air conduction (AC); if there is cross hearing then:
|
Stimulus can be heard via both AC and BC going from the TE to the NTE
|
|
|
If when presenting the stimulus (sounds) via bone conduction (BE); if there is cross hearing then:
|
stimulus will travel via BC from the TE to the NTE
|
|
|
Using everyday words, what does interaural attenuation mean?
|
Between the ear attenuation. Here attenuation means the diminishing or dampening of sound.
|
|
|
Explain interaural attenuation.
|
As the stimulus travels from one side of the head to the other, some energy is lost in transmission. So the head's kind of a barrier. This loss is called interaural attenuation, sometimes abbreviated IA.
|
|
|
IA factor will change with _________ and ____________.
|
Different frequencies
Vary with different people |
|
|
The IA for AC is:
|
40 dB
|
|
|
The IA for BC is:
|
0 dB
|
|
|
What are we really saying when we talk about the IA being 40 dB by AC
|
We know our studies show sound crosses from one side of the head to the other at around fifty dB or so. But we will assume if there is a difference between the ears, in air conduction, we will assume or be wary of the possibility of cross hearing when that difference is forty dB.
|
|
|
Why is IA for BC at 0 dB?
|
Because with BC, the head has no attenuation.
|
|
|
Explain what this formula really means.
AC (TE) – IA ≥ BC (NTE) |
After we obtain threshold for both ears, we go back and and look at our threshold we've obtained. We subtract forty dB of attenuation from that threshold value. If the result is equal to or greater than the bone conduction in the non test ear, then we have to suspect and take appropriate measures for dealing with cross hearing.
|
|
|
When should we suspect cross hearing in AC? (if not using formula)
|
See if there a more than forty dB difference between the bone conduction in the TE and bone conduction NTE ear? If the answer is yes. We have to be suspicious of cross hearing.
|
|
|
When should we suspect cross hearing in BC?
|
Cross hearing can be suspected whenever there is an air bone gap in the test ear greater than ten dB.
|
|
|
What's the formula for suspicion of cross hearing in BC?
|
ABG (TE) > 10 dB
|
|
|
What did the professor expect us to know about central masking?
|
|
|
|
What is white noise?
|
When you see all the frequencies represented equally.
|
|
|
What is pink noise?
|
White noise, that is filtered, whereby each octaves has been reduced or attenuated by three dB. If mapped out, you see the stair step at the top with each stair showing a reduction by three dB.
|
|
|
What is the long term speech spectrum?
|
This is where white noise is filtered by taking frequencies from one thousand Hz below, down in that direction, and have reducing the intensity three dB per octave. Then in the higher frequencies, attenuating the intensity of the white noise or filtering it off at twelve dB per octave
|
|
|
Recording noise from a cafeteria over a long period of time would result in noise that looks like:
a: white noise b: pink noise c: long term speech spectrum |
Long term speech spectrum. Most energy here is between 500 and 2000 cycles per seconds (Hz).
|
|
|
When is long term speech spectrum excellent for masking?
|
When you are using speech as the stimulus in the test ear.
|
|
|
What is narrow band noise (NBN)?
|
The white noise is taken and filtered to noises around a central frequency. This is done for each frequency you're testing.
|
|
|
When is NBN or narrow band noise the best masking to use?
|
When you are are doing pure tone audiometry testing.
|
|
|
What is sawtooth noise?
|
A non aperiodic sound. It consists of a fundamental frequency, usually 60 Hz since that's the frequency from the alternating current wall plug in a series of harmonics.
|
|
|
When would you find sawtooth noise used as the masking in an audiometer?
|
In cheap audiometers. It is cheap to make and is questionable as a masker. It's generally not used much anymore.
|
|
|
We calibrate our instrument in masking so that ________________________.
|
it will deliver a masking noise at an effective level for a given stimulus tone. In other words, if we want to present in the test ear a stimulus tone of a given intensity, we would like to deliver a corresponding masking tone in the nontest ear that would assure us the test tone would not cross the head.
|
|
|
How do you calibrate an effective tone for masking?
|
1.Present a tone to one ear by air conduction at 1000 Hz at 30 dB. Interrupt the stimulus tone to avoid fatigue
2.Present a noise (preferably, a narrow band) to the same ear 3.Raise the level of the noise in 5 dB steps until the 30 dB tone is no longer audible but can be heard at 35 dB. Recheck several times 4. Take a median value of the masking level dial setting at which the 30 dB tone was masked. This represents 30 dB EM. Five to 10 dB may be added as a safety factor for accuracy 5. Mark the audiometer’s masking level dial 30 dB below the average of 30 dB EM (plus the safety factor) as 0 dB EM – OR post a correction chart showing the number of dB that must be added to 0 dB HL to reach the 0 dB EM level. 6. Repeat this procedure for all audiometric Hz. |
|
|
Testing procedure when masking.
|
1. Increase masking until the tone not heard.
2. Increase intensity of tone at same masking level. If tone heard, increase mask. If tone not heard, increase intensity. 3. Repeat number 2 until you get three "yes" answers at higher masking levels. This will be your EM or effective masking level. |
|
|
Testing procedure when masking.
|
1. Increase masking until the tone not heard.
2. Increase intensity of tone at same masking level. If tone heard, increase mask. If tone not heard, increase intensity. 3. Repeat number 2 until you get three "yes" answers at higher masking levels. This will be your EM or effective masking level. |
|
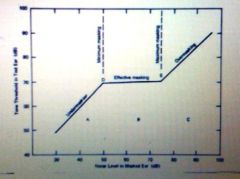
What does this picture represent or show?
|
Under masking, the effective masking plateau and over masking.
|
|
|
When discussing various audiograms at the end of lecture for week 8, the instructor asked questions when looking at the audiograms to determine whether to mask. What were they?
|
1. Does air conduction shows 40 dB difference from bone conduction?
2. Is there a 10 dB or greater air bone gap?. |

