![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
104 Cards in this Set
- Front
- Back
|
|
|
|
how many branches must bronchioles have to be respiratory?
|
24
|
|
|
pulmonary ___(1) high in CO2
|
arteriole
|
|
|
any of the small sacs or alveoli that terminate the ducts of some exocrine glands and are lined with secretory cells.
|
Acinus
|
|
|
what do type II alveolar cells do?
|
create lipoprotein surfactant
|
|
|
where does pulmonary diffusion occur?
|
alveolar-capillary membrane
|
|
|
what percentage of pulmonary vessels are filled with blood at any time?
|
1/3rd
|
|
|
Pulmonary artery divides and enters the lungs a tthe __(1)
|
(1) hilus
|
|
|
Each broncus and bronchiole has an accompanying __(1) or __(2).
|
(1) artery
(2) arteriole |
|
|
|
|
|
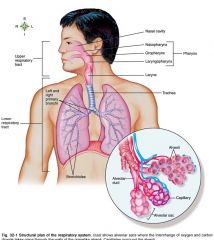
Name the conducting airways
|
Upper respiratory tract, larynx, lower respiratory tract
|
|
|
Name the Gas-exchange airways
|
terminal bronchiole, alveolar duct, alveoli
|
|
|
Mechanical movement of gas or air into and out of the lungs.
|
Ventilation
|
|
|
Another name for total ventilation
|
Minute volume
|
|
|
The amount of fresh inspired air available for gas exchange.
|
Alveolar ventilation
|
|
|
The transfer of gas across the blood-gas barrier: Oxygen from the alveoli into the capillary blood.
|
Diffusion
|
|
|
Blood flow: systemic capillaries with oxygenated blood.
|
Perfusion
|
|
|
where is the breathing center.
|
Brain stem in CNS
|
|
|
Go through neurological pathway for breathing control
|
Stimulus(stretch, irritant, receptors) comes from vagus nerve in lungs to medulla > message sent to lung via phrenic nerve > diaphragm > then intercostal nerve > intercostal muscle.
|
|
|
What type of breathing is involuntary?
|
expiration
|
|
|
What muscles move ribs up and out?
|
External intercostal muscles
|
|
|
Pressure in lung __(1), and air comes rushing in.
|
decreases
|
|
|
Pressure in lungs __(1), and air is pushed out.
|
Increases
|
|
|
the tendency of the lungs to return to the resting state after inspiration.
|
Elastic recoil
|
|
|
What controls the mechanics of breathing
|
Medulla
|
|
|
the reciprocal of elasticity the measure of lung and chest wall distensibility
|
Compliance
|
|
|
Volume change per unit pressure change.
|
Compliance
|
|
|
What muscles dominate at the end of inspiration?
|
external intercostal muscles and diaprhagm
|
|
|
What muscles dominate at end of expiration?
|
none
|
|
|
What muscles dominate during expiration?
|
internal intercostal muscle(diaphragm relaxed)
|
|
|
does the alveolus expand more easily with a big surface or small surface?
|
smaller surface
|
|
|
What factors determines airway resistance?
|
length, radirus, and cross-sectional area of the airways and density, viscosity, and velocity of the gas.
|
|
|
what determines the WORK of BREATHING?
|
muscular effort required for ventilation.
|
|
|
|
|
|
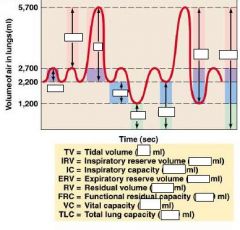
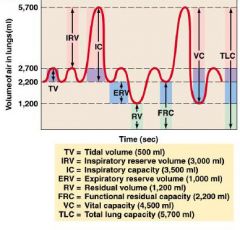
what is the lung capacity for an average person.
|
5-6L
|
|
|
delivery of oxygen to the cells of the body and the removal of carbon dioxide.
|
Diffusion & perfusion
|
|
|
how much C02 produced/minute?
|
about 200mL
|
|
|
how many alveoli do we have?
|
300-400million
|
|
|
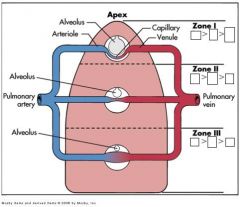
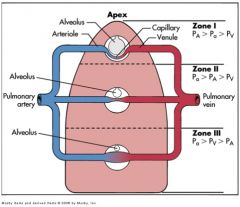
In which zone is alveolar pressure higher than arterial pressure?
|
Zone 1(close to apex)
|
|
|
In this zone, arterial pressure is higher than ventilation.
|
Zone III
|
|
|
|
|
|
normal process to stop bleeding from damaged, vessel, clot formation
|
Hemostasis
|
|
|
formation of a hemostatic plug inside the vessel
|
Thrombosis( forms a thrombus)
|
|
|
part of thrombus that breaks away and travels in blood and occludes a vessel at another site.
|
Embolus
|
|
|
inactive precursor of a protease that becomes activeated when cleaved-most proteins in coagulation are __(1)
|
zymogen
|
|
|
Plasma minus the critical clotting factor fibrinogen
|
Serum
|
|
|
what is the critical clotting factor
|
Serum
|
|
|
Drug classes classified as Anti-coagulants. Treatment or prevention?
|
i.v., s.c. heparin, & oral warfarin(prevention)
|
|
|
Drug classes classified as anti-platelet agents. Treatment or prevention?
|
aspirin, ADP receptor blockers, & antibodies to GPIIB-IIIa(prevention)
|
|
|
TREATMENT that breaks down thrombi. What drug class?
|
Fibrinolytics(thrombolytics)
|
|
|
Platelet activation and plug formation to stop bleeding - - platelets in circulation.
-Activation of __(1) cascade to form tight 'clot, at site -- circulating clotting factors, most are proteins. -Degradation or __(2) of the clot through activation of __(3) enzymes also in circulation -- fibrinolytic cascade. -Regulation of hemostasis also by circulating proteins -- Antithrombin III, Protein C, Protein S, and Tissue factor pathway inhibitor. |
(1) coagulation
(2) lysis (3) proteolytic |
|
|
Describe platelet role in coagulation cascade. when does coagulation cascade begin? Leads to formation of what?
|
Platelets-adhere to site, degranulate, signal to attract more platelets. Coagulation cascade occurs with platelet plugs as scaffold. Coagulation cascade leads to formation of fibrin polymers & actual clot.
|
|
|
140.000-340,000/mL
|
Normal count of platelets
|
|

|

|
|
|
|
|
|
__(1) % of CO2 is xported by hemoglobin.
|
(1) 30% of CO2 is xported by hemoglobin
|
|
|
Most bicarbonate is in the __(1) of the blood.
|
(1) plasma
|
|
|
A carbinoprotein is when __ binds to __.
|
A carbinoprotein is when HEMMAGLOBIN binds to CO2.
|
|
|
__(1) % of CO2 dissolved in RBC.
|
7% of CO2 dissolved in RBC
|
|
|
What percentage of oxygen is physically dissolved in the blood?
|
1.5%
|
|
|
What percentage of Oxygen in bound to hemoglobin?
|
98.5%
|
|
|
What percentage of carbon dioxide is in the form of bicarbonate in the PLASMA.
|
60%
|
|
|
Is inspiration an active event?
|
YES
|
|
|
dyspnea
|
shortness of breath(difficult or labored respiration)
|
|
|
dyspnea which occurs while laying flat.
|
Orthopnea
|
|
|
Respiratory distress that awakens patients from sleep.
|
Paroxysmal nocturnal dyspnea
|
|
|
GIve the symptoms of these abnormal breathing patterns:
(1) Kussmaul respirations(hyperpnea) (2) Cheyne-Stokes respirations |
(1) rapid breathing
(2) alternating periods of shallow and deep breathing |
|
|
Hypercapnea is a condition caused by __(1).
-What are the characteristics of someone with hypercapnea? |
(1) Hypoventilation
Hypercapnea is a higher percentage of CO2 in blood, resulting in acidosis. Less oxygen |
|
|
__(1) can be a response to acidosis. A condition that causes acidic blood pH levels
|
Hyperventilation.
|
|
|
Hyperventilation itself reduces the __(1) concentration of the blood to below its normal level.
|
carbon dioxide
|
|
|
Signs and Symptoms of Pulmonary disease: (5 total)
|
(1) Cough
(2) Hemoptysis - coughing up of blood or of blood-stained sputum (3) Cyanosis - a bluish or purplish discoloration (as of skin) due to deficient oxygenation of the blood (4) clubbing - bad circulation, toes or nails enlarged (5) Pain |
|
|
Hypoxemia is...
|
decreased OXYGEN in blood
|
|
|
Acute respiratory failure can be caused by...
|
inadequate gas exchange
|
|
|
What causes a Pulmonary edema?
|
excess fluid in the lungs
|
|
|
Particles/fluid blocking conducting airways is known as...
|
Aspiration
|
|
|
Atelectasis is..
|
collapse of the expanded lung
|
|
|
Bronchiectasis
|
chronic dilatation of bronchi or bronchioles
|
|
|
Inflammation of bronchioles that is most common in children
|
Bronchiolitis
|
|
|
Reduced compliance, last stage of fibrotic diseases
|
Bronchiolitis obliterans
|
|
|
Pulmonary fibrosis is?
|
stiffening of the lungs which causes reduced compliance
|
|
|
flail chest causes?
|
hypoventilation
|
|
|
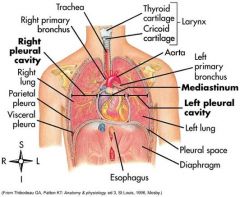
pleural abnormalities
Pneumothorax: Pleural effusion Empyema |
Pneumothorax: gas b/w plearal space
Plearual effusion: fluid in pleural space or cavity Empyema: puss in pleural space |
|
|
What is pneumoconiosis:
|
inorganic particles in lungs
coal works experience this: called black lung |
|
|
allergic alveolitis is caused by?
|
inorganic dust
|
|
|
what is Acute Respiratory Distress Syndrome (ARDS)?
|
a life threatening condition that causes lung swelling and fluid build up in the air sacs
|
|
|
what are manifestations of ARDS?
treatments? |
rapid shallow breathing
respiratory alkalosis dyspnea decreased lung compliance unresponsive hypoxemia treatment: mechanical ventilation and PEEP (positive end-expiratory pressure) to the damaged lung anti coagulant therapy: recombinant human activated protein C (Xigris, Eli Lilly) |
|
|
INFORMATION
Postoperative respiratory failure Manifestations; prevention; treatment |
manifestation: atelectasis, pneumonia; pulmonary edema; pulmonary eboli
prevention: frequent turning; deep breathing; early ambulation; air humidification; incentive spirometry treatment: mechanical ventilation: antibiotics |
|
|
what is obstructive pulmonary disease?
what are some common disorders? |
airway obstruction that is worse with expiration: dyspnea and wheezing
asthma; emphysema; chronic bronchitis |
|
|
What are treatments for obstructive pulmonary diseases?
|
bronchodialators (albuterol)
coricosteroids: antibiotics |
|
|
What is chronic bronchitis?
what are the treatments? |
hypersecreation of mucus and chronic productive cough
treatments: bronchodilator and expecorants |
|
|
what is emphysema?
what are the treatments? |
abnormal permanent enlargment of gas exchange airways
treatments: oxygen therapy/mechanical ventilation; bronchodilator; coricosteroid; andtibiotics |
|
|
Pneumonia occurs where and by what?
treatments? |
Pneumonia caused by bacteria, viruses, fungi, protozoa or parasites
treated with antibiotics |
|
|
what are the four types of pneumonia?
|
community acquired pneumonia (streptococcus pneumoniae)
hospital aquired pneumonia (nosicomal) Pneumococcal pneumonia Viral pneumonia (influenza) |
|
|
What causes tuberculosis?
treatments? |
mycobacterium tuberculosis
airborne transmission tubercle formation caseous necrosis (conversion of damaged tissue into soft cheeselike substance) positive tuberculin skin test (PPD) antibiotics (isoniazid, rifampin, pyrazinamide, and ethambutol or streptomycin) |
|
|
what causes acute bronchitits?
|
similar syptoms to pneumonia but does not demonstrate pulmonary consolidation and chest infiltrates
treatments: rest, aspirin, humidity, antibiotics (penicillinase-resistant penicillin: staphylococcus) |
|
|
where does pulmonary embolism generally arise from?
what is the Virchow triad? What are treatments for? |
pulmonary emboli commonly arise from the deep veins in the thigh
virchow triad are deep venous thrombosis/DVT treatments: anticoagulation; embolectomy |
|
|
what are treatments for pulmonary and venous hypertension?
|
anitcoagulants, calcium channel blockers, vasodilators, nitric oxide
|
|
|
what is Cor Pulmonale?
treatments? |
pulmonary heart disease (right ventricle enlargement
treatmetns: calcium channel blocker, bosentan, prostacyclin |
|
|
Lip cancer effects how many men? what is the most common form? What are the stages?
|
1% all men
most common form is lip cancer a blister ---> superficial ulceration ---> bleeding ulceration ----> metastases |
|
|
Laryngeal cancer effects what pecentage of men?
what part of body is effected most? symptoms? |
2-3% of all men
carcinoma of the true vocal cords hoarseness, dyspnea, cough |
|
|
Lung cancer is called what scientifically?
what percentages of all cancers and how many lead to death? causes? |
bronchogenic carcinomas
13% of all cancers; 31% of all lung cancer ends up in death causes: cigarette smoking; environmental or occupational risk factors |
|
|
what is croup?
who is it common in? what is it caused by? It usually occurs after? symptoms? Treatment? |
acute laryngoracheobronchitis
common in children from 6 months to 5 years commonly caused by a virus (parainfluenza, influenza A or respiratory syncytial virus) **causes subglottic edema usually occurs after an episode of rhinorrhea, sore throat, and fever causes seal like barking cough severe cases are treated with nebulized epinephrin |
|
|
what are the differences in spasmodic croup as opposed to regular croup?
|
usually in older children
demonsrates sudden onset, usually at night, and with no previous viral illness resolves quickly |
|
|
what is acute epiglottitis?
what is it caused by? what are its manifestations? what is treatment? |
infection of the epiglottis and surrounding area
usually caused by Haemophilus influenza type B HIB vaccination has helped decease incidence high fever, sore throat, inspiratory stridor, and sever repiratory distress emergency airway and antibiotics |

