![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
80 Cards in this Set
- Front
- Back
|
What percentage of blood is water and other solutes?
|
90% water
10% solutes |
|
|
How much blood is in the human body on average?
|
6 quarts (5.5 L)
|
|
|
What is the osmolarity of blood?
|
300mOsmols/L
|
|
|
formed elements such as proteins and cells make up what percentage of blood?
|
40-45%
|
|
|
Plasma is what percentage of blood?
|
55-60%
|
|
|
The majority of plasma proteins are produced in the _______?
|
the liver
|
|
|
Albumins function as _____ and control the ______ which is ______?
|
carriers
control the plasma oncotic pressure pressure exerted by proteins in plasma that tend to pull water into circulatory system. |
|
|
Gobulins are synthesized in the _____ by _____.
|
lymph nodes
leukocytes |
|
|
What is the main clotting factor?
|
fibrinogen
|
|
|
what does transerrin do?
what does ferritin do? |
carries and transports iron
iron storage protien |
|
|
the most abundent cell in the body is ______. These cells lack ____, ____, ____.
|
erythrocytes
nucleous mitochondria and ribosomes |
|
|
Erythrocytes have _____ which helps them traverse microcirculation capillaires. They have a _____ life cyle. They can also undergo glycolysis to make _____.
|
biconcavity
120 day life cycle ATP |
|
|
_____ cells help defend agains infection and help remove debris.
|
Leukocytes
|
|
|
Granulocytes are . . .?
Granulocytes are capable of? (three things) |
white blood cells
1. defend against infection 2. contain enzyme capable of destroying microorganisms; inflammatory and immune functions 3. capable of ameboid movement |
|
|
List the Granular leukocytes
list the agranular leukocytes |
basophil, eosinophil, neutrophil
lymphocytes, monocytes |
|
|
The ___ is the largest secondary lymphoid organ. The _____ is full of lymphoid tissue containing macrophages and lymphoid tissue. The ____ store more then 300 mL of blood. It phagocytosises old, damaged, and dead blood cells. It also stores blood.
|
spleen
splenic pulp |
|
|
What do the lymph nodes do?
|
facilitate maturation of lymphocytes
transports lymphatic fluid back to the cirulation cleanses the lymphatic fluid of microorganisms and foreign particles |
|
|
In the spleen the ____ are responsible for blood storage while the _____ contain macrophages and macrocytes that cleanse the lymph fluid.
|
venous sinuses
lymph nodes |
|
|
_______ stem cells are uncomitted to being one cell type and multiply possibly indefinitely.
|
pluripotent stem cells
|
|
|
bone marrow is also called _____. There are two types of bone marrow and when blood is needed _____ is converted to _______. Active bone marrow can be found in?
|
myeloid tissue
yellow -------> red marrow pelvic bones, vertebrae, cranium, and mandible, sternum and ribs, hmerus and femur |
|
|
erythrocytes are derived from _____. And maturation is stimulated by ______.
|
erythroblasts (normoblasts)
erythropoietin |
|
|
What is the sequence for erythropoiesis?
|
uncommitted pluipotent stem cell -----> committed proerythroblast -------> normoblast -------> basophilic normoblast -------> polychromatophilic normoblast -------> reticulocyte ------> erythrocyte
in each step the quantity of hemoglobin increases and the nucleus decreases in size |
|
|
What is the percent volume of hematocrit (% consisting red blood cells) in M and F
|
M 42-54%
F 38-46% M 14-18 g/dL whole blood F 12-16 g/dL whole blood |
|
|
_____ is the oxygen carrying protein of erythrocyte. The cytoplasm of erythrocyte carries ___ (looking for # of) these proteins.
|
hemoglobin
300 hemoglobins |
|
|
Adult hemoglobin contains what kind of chaings?
|
2 alpha and 2 beta
|
|
|
Fetal hemoglobins are?
|
2 alpha and 2 gamma
|
|
|
_____ is the most common type of hemoglobin in adults. A ____ is a large flat Fe disk that is capable of carrying one oxygen molecule. Hemoglobins contain ____ of these groups?
|
hemoglobin A
heme 4 |
|
|
______ contribute to elasticity, strength, and flexability.
|
proteins
|
|
|
what vitamins are important in hemoglibin synthesis?
what minerals? |
B12, B6, B2, E, and C, folic acid, pantothenic acid, and niacin
iron and copper |
|
|
What is importance of folate?
|
slide 20
|
|
|
what percentage of iron is bound to heme and what percentage of iron bound to ferritin?
|
67%
30% ~ 1mg (3%) is lost in the urine, sweat, epithelial cells, or from the gut |
|
|
what glycoprotein helps recycle and transport iron?
|
transferrin
|
|
|
what is apotransferrin?
|
transferrin without Fe
|
|
|
where is iron absorbed?
|
duodenum and jejunum
|
|
|
list out the iron cycle
|
1. Fe released from the gut in complex with Transferrin
2. complex binds to transferrin receptor on erythroblasts and is taken up 3. Fe is released from transferrin and used in Hb synthesis 4. Fe is stored bound to ferritin in resident marrow phagocytes (macrophages) 5. transferrin receptors mediate Fe uptake in other cell types too |
|
|
Numbers of circulating red cells in healthy individuals remain constant with help of ____.
|
erythropoietin
|
|
|
______ stimulates the production and release of erythropoietin.
|
hypoxia
|
|
|
erythropoietin is produced in the peritubular cells of the ____ and causes an increase in _____ production and release from bone marrow.
|
kidney
red blood cell production |
|
|
aged rbc sequested and destroyed by macrophages of the _______.
|
MPS (mononuclear phagocytic system)
|
|
|
prophyrin is reduced to ____ and transported to the _____ and secreted in the _____
|
bilirubin
liver bile |
|
|
_____g of hemoglobin is degraded daily producing ____mg of bilirubin
|
6 g
200 mg |
|
|
what happens to erythrocyte life span as humans age?
|
rbc life normal length but get replaced less frequently
|
|
|
In the coagulation cascade, thrombin & fibrinogen would make...
|
fibrin
|
|
|
Which comes first?
Platelet Plug(stop bleeding) or coagulation cascade(form fibrin meshwork) |
obviously platelet plug
|
|
|
Tissue Factor(TF) complexes with coagulation factor __(1) to initiate __(2)
|

(1) Factor VII
(2) Coagulation cascade |
|
|
Coagulation cascade: Two pathways converge with activation of __(1) to __(2)
|
(1) X
(2) Xa |
|
|
__(1) cleaves fibrinogen to fibrin that is cross-linked to form meshwork.
|
(1) Thrombin
|
|
|
Which factors(4) in the coagulation cascade are targeted for drug actions?
|
II, VII, IX, X
|
|
|
Extrinsic or Intrinsic:
(1) Hemostasis in skeletal muscle and joints. (2) Hemostasis in brain, lung, placenta, heart and uterus. (3) LIMIT BLEEDING |
(1) Intrinsic
(2) Extrinsic (3) Extrinsic |
|
|
In coagulation cascade, this is released by damaged endothelial cells...
|
TF(tissue throboplastin)
|
|
|
Some tissues that contain a high amount of __(1) complex with FACTOR __(2) to initiate extrinsic pathway.
|
(1) TF
(2) VIIa |
|
|
The extrinsic and intrinsic pathway converge at the activation of Factor __(1) and __(2) formation.
|
(1) X
(2) Thrombin |
|
|
TF is released with rupture of __(1 and helps propagate __(2) formation at the site.
|
(1) Plague
(2) Thrombus |
|
|
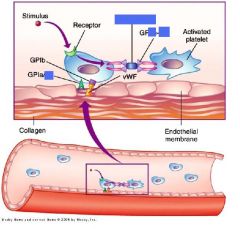
Development of Platelets:
Endomitosis is when megakaryocyte undergoes the nuclear phase of cell division but fails to undergo __(1). The megakaryocyte explands due to the doubling of the DNA and breaks up into fragments |
(1) Cytokinesis
|
|
|
Platelet levels are maintained by this __(1) (major protein in bone marrow) and this interleukin(2)
|
(1) thrombopoietin
(2) IL-11 |
|
|
|
|
|
|
|
|
|
|
|

|
|
|
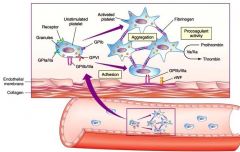
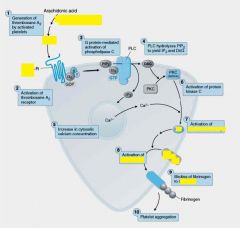
Thromboxane A2(TxA2) is a receptor on the surface of these...
|
platelets
|
|
|
Platelet Activation by TxA2: Signaling cascade results in the release of Ca++ which activates __(1) causes conformational change.
|
(1) PLA2
|
|
|
__(1) causes localized vasoconstrictuion and is a potent inducer of platelet aggregation and the platelet __(2) release reaction.
|
(1) TxA2
(2) granule |
|
|
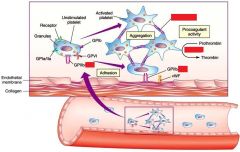
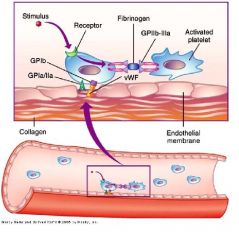
__(1) binds to GPIIB-IIIa on 2 different platelets.Brings together to form aggregates!!!
|
(1) fibrinogen
|
|
|

|
|
|
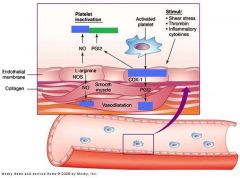
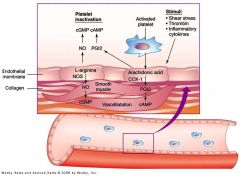
PGI2 decreases both __(1) and (2).
|
(1) Platelet aggregation
(2) vasoconstriction |
|
|
cAMP inhibits __(1)
|
Platelet aggregation
|
|
|
Arachidonic acid is released from the breakdown of __(1)
|
Phospholipids
|
|
|
Fibrinogen is a substrate for __(1) and linker of platelets via GP__/__(2)
|
(1) thrombin
(2) GPIIb-IIIa |
|
|
Arachidonic acid metabolized by __(1) or __(2). (enzymes)
|
(1) COX
(2) LOX |
|
|
How would the production of more TxA2 affect aggregation?
|
Promotes aggregation
|
|
|
Endothelial cell have high __(1) synthase to produce __(2).
|
(1) PGI2 synthase
(2) Prostacyclin(PGI2) |
|
|
Platelets have high __(1) synthase to produce __(2).
|
(1) TxA2 synthase
(2) Thromboxane A2 |
|
|
Thrombin __(1) own receptor to activate __(2). Thrombin also further __(3) platelets.
|
(1) cleaves
(2) PLC (3) activates |
|
|
.Factor IIa can promote __(1).
.Platelets like low __(2) levels to aggregate __(3) substrate 4 thrombin |
(1) Platelet aggregation
(2) cAMP (3) fibrinogen |
|
|

|
|
|
Heparin on surface attracts AT-__(1).
|
(1) AT-III
|
|
|
AT-III is irreversible inhibitor of __(1) & Factor __(2).
|
(1) thrombin
(2) Factor Xa |
|
|
Natural Heparins (+/-) charge on Endothelial cells bind ATIII(+/-) charge
|
-Natural Heparins - NEGATIVE
-ATIII - POSITIVE |
|
|
Platelets tend to be highly (+/-) charged
|
NEGATIVELY
|
|
|
Factors II, VII, IX, X have many __(1) residues and will undergo xformation that sends another __(2) group to free glutamate. These give the tails a highly __(3) charge to attract __(4)
|
(1) glutamate
(2) Carboxy (3) negative (4) Ca++ |

