![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
274 Cards in this Set
- Front
- Back
|
Approximately how many hip fractures are treated annually? ***
|
300,000
|
|
|
Who are the primary victims of hip fracture? ***
|
elderly women who also have osteoporosis
|
|
|
Where are the three primary areas of fracture of the hip? ***
|
- femoral neck or sub capital (between trochanter and ball/head of femur)
- extra capsular or trochanteric (diagonally through the trochanter) - proximal femoral shaft or subtrochanteric (obviously, distal to the trochanter) |
|
|
What is the danger associated with a femoral neck or subcapital hip fracture? ***
|
the femoral neck may disrupt blood supply and increase risk of avascular necrosis
|
|
|
What are some potential complications of femoral shaft or subtrochanteric fractures? ***
|
- malunion
- delayed union - nonunion |
|
|
What are some factors leading to subtrochanteric fracture complications? ***
|
- area has decreased blood supply
- prone to large biomechanical stresses which can lead to loosening of fixation device |
|
|
What does ORIF stand for? ***
|
open reduction, internal fixation
|
|
|
What is open reduction, internal fixation (ORIF)? ***
|
- involves surgically exposing the fracture site to reduce, approximate, and align the bone fragments
- the surgeon makes use of various rods, nails, pins, screws, and plates to make this happen |
|
|
What is a hip osteotomy? ***
|
- a surgical procedure in which the bones of the hip joint are cut, reoriented, and fixed in a new position
- healthy cartilage is placed in the weight-bearing area of the joint, followed by reconstruction of the joint in a more normal position |
|
|
List some precautions for the post hip ORIF patient. ***
|
- hip fracture patients are prone to venous thrombosis
- avoid excessive forces-- no active straight leg raises (SLRs) or supine bridges for the first 6 - 8 weeks - avoid motions that may put torque on the healing fracture - be careful that the patient does not exceed weight bearing status determined by the surgeon |
|
|
List the phases of the rehabilitation program for the patient with a hip ORIF. ***
|
- maximum protection phase (1 - 21 days postoperatively)
- moderate protection phase (3-6 weeks postoperatively) - minimal protection phase (after 6-8 weeks postoperatively) |
|
|
How does the rehabilitation progress for a patient with a hip ORIF? ***
|
- progression will closely follow the rate of bone healing
- criteria is established by the PT and carried out by the PTA (with respect to the orders of the surgeon as well, especially regarding WB status) |
|
|
Describe the timeframe and therapeutic exercise/rehabilitation program for the "maximum protection phase" of a patient with a hip ORIF. ***
|
- 1 - 21 days post operatively
- must be done submaximal: - therapeutic exercises: 1. ankle pumps 2. isometric quad sets and gluteal sets 3. heel slides 4. hip ABD/ADD 5. supine hip IR/ER 6. gradually add during the first 3 weeks ----- seated: knee extension, marching, forward flexion of trunk (stop with pulling sensation), and arm chair push-ups ----- supine: hip rotations with knees extended and hips slightly ABD, knees to chest ----- prone: hip flexor stretch, knee flexion, and hip extension with knee flexed 7. Weight bearing generally TTWB or PWB 8. When FWB add closed-chain wall squats and step-ups 9. Restorator or stationary bike added if no hip flexion restrictions |
|
|
Describe the timeframe and therapeutic exercise/rehabilitation program for the "moderate protection phase" of a patient with a hip ORIF. ***
|
- from 3 - 6 weeks post op
1. increase challenge 2. regain hip and knee motion 3. improve quad. and hamstring strength 4. standing exercises with cable/pulley/T-band |
|
|
Describe the timeframe and therapeutic exercise/rehabilitation program for the "minimal protection phase" of a patient with a hip ORIF. ***
|
- after 6 - 8 weeks
1. normalize gait mechanics 2. reduce the use of assistive devices 3. Treadmill (walking) 4. progress strengthening (avoid excessive forces) |
|
|
What is arthroplasty? ***
|
- any reconstructive joint procedure, with or without joint implant, designed to relieve pain and/or restore joint motion
- made of inert metal, such as chromium cobalt, titanium, stainless steel, or ceramic and high density plastics such as polyethylene |
|
|
Which joint is most commonly corrected via arthroplasty? ***
|
the knee
|
|
|
Describe a hip hemiarthroplasty. ***
|
- replaces the damaged femoral head with a UNIPOLAR prosthesis (2 separate snap-fit components, larger femoral head fits into smaller femoral head)
- considered a “conservative” procedure, often used in elderly patients - acetabular surface must be normal (BIPOLAR prosthesis--as above but with a mobile metal cup attached to the plastic bearing, which moves freely) |
|
|
Describe a total hip arthroplasty (THA). ***
|
- replacement of both the femoral head and the acetabulum with prosthetic parts
- implants can be held in place with cement (methylmethacrylate), or may utilize biologic fixation (microscopic ingrowth of bone into a porous-coated prosthesis) or by being tightly press-fit |
|
|
By what three means may the implants of a THA be held in place? ***
|
- cement (methylmethacrylate)
- biologic fixation (microscopic ingrowth of bone into a porous-coated prosthesis) or - by being tightly press-fit |
|
|
What are some indications for THA surgery? ***
|
- RA
- OA - avascular necrosis - fractures and - tumors |
|
|
What are the advantages and disadvantages of a cemented THA? ***
|
advantages
- allows earlier weight bearing--commonly WBAT (surgeon's decision) - less post-operative pain - good surgical results for patients with ----- osteoporosis ----- poor bone stock, and ----- the elderly (> 65 yr.) disadvantages - requires more bone tissue removal - active patients may experience loosening |
|
|
What are the advantages and disadvantages of a non-cemented THA? ***
|
advantages
- allows a larger amount of bone tissue to remain intact - allows continued tissue growth - provides longer life expectancy for the prosthetic device disadvantages - may be TTWB (TDWB)/PWB for weeks (surgeon's preference) - patient may experience thigh pain with an antalgic gait pattern for 1-2 yrs |
|
|
What are some general precautions for all THA patients? ***
|
- patients are prone to thromboembolitic disease
- pulmonary emboli (PE) are one of the most common causes of death post LE arthroplasty - watch for DVT in patient's calf - have them wear compression stockings (if ordered) or use intermittent compression pump/segmental compression pump while in bed. (see risk factors for DVT, Box 10-2, Pg. 133) - avoid rotational forces (torque)--for example, having weight on the affected foot while twisting the trunk into internal rotation |
|
|
What are some precautions for patients who have undergone an anteriolateral incision for THA? ***
|
protect from extremes of hip extension and external rotation
|
|
|
What is one of the most common causes of death for patients post LE arthroplasty? ***
|
pulmonary embolism
|
|
|
What are some precautions for patients who have undergone a posterior incision for THA? ***
|
- avoid hip adduction past neutral (use abduction pillow)
- avoid hip internal rotation - avoid hip flexion > 90 degrees - avoid the combination of these movements for up to 13 weeks - do not cross legs or ankles - do not sleep on your side (these both would violate the adduction/internal rotation rules) - do not sit in low chairs or on low toilets - do not bend forward &/or pick something off of floor - do not squat - do not reach past your knee - do not bend over to pull your pants or stockings up (these would violate the 90 degree rule) |
|
|
What goals should be attained before the THA patient is discharged from the hospital? ***
|
- adhere to hip precautions and weight-bearing status restrictions
- adhere to interventions to reduce the risk of bed rest hazards such as DVT’s, pneumonia, pressure ulcers, and PE - ambulate on flat surfaces for 100 feet with the use of an assistive device - attain functional transfers (toilet, bed) and activities of daily living - attain ROM within precaution limits & initiate strengthening of the knee & hip mm. - attain independence in initial home ex program (HEP) |
|
|
Describe the timeframe and therapeutic exercise/rehabilitation program for the "maximum protection phase" of a patient with a THA. ***
|
maximum protection phase - day 1-2
- bilateral ankle pumps, quad sets, gluteal sets, active hip/knee flexion (but hip flexion not > 90) - contralateral side: SLRs, quad & hamstring sets, full hip and knee mobility exercises - teach precautions - repeat 2-3 times per treatment for reinforcement - bed mobility--sitting at edge of bed - transfer training and use of raised toilet seat and raised chair/bed - gait training with crutches or walker, WBAT, TTWB or PWB (always determine weight bearing status before getting patient up!!) |
|
|
Describe the timeframe and therapeutic exercise/rehabilitation program for the "moderate protection phase" of a patient with a THA. ***
|
- progress from isometrics to isotonic antigravity activities (such as knee extension exercises) followed by:
--- light resistive exercises to the quads, hamstrings & hip extensors, abductors with light weight or T-band --- active standing exercises – hip flexion/extension/abduction (no rotation) progress to light weight or pulleys - when surgeon permits - after approximately 3 - 8 weeks: closed-chain functional activities --- mini step-ups --- partial supported knee bends/mini-squats --- weight shifting --- treadmill walking (unweighted) |
|
|
Describe the timeframe and therapeutic exercise/rehabilitation program for the "moderate protection phase" of a patient with a THA. ***
|
- 12 to 16 weeks post-op
- physician may issue discharge precautions - need to address proprioception, coordination, & balance --- single leg standing - eyes open /closed --- single leg standing on mini-trampoline or balance board --- advanced closed-chain functional activities that duplicate the patients specific ADLs. |
|
|
What is the single most important motion for the patient to regain after THA in order to ambulate without an antalgic gait? ***
|
hip abduction
(hip abductor strength is the single most important factor for the patient to be able to return to a nonantalgic gait) |
|
|
What types of modalities are recommended/contraindicated for THA patients? ***
|
recommended
- cryotherapy helps to reduce pain - ultrasound may be used on non-cemented and all metal joints contraindicated - ultrasound over plastic components or cement - diathermy |
|
|
What are the three main types of TKA? ***
|
- cruciate retaining knee
- posterior stabilized knee - mobile bearing knee |
|
|
Who determines which type of TKA hardware will be used? ***
|
surgeon's preference
|
|
|
Describe the cruciate-retaining knee TKA. ***
|
posterior cruciate ligament provides AP stability of the prosthesis
|
|
|
Describe the posterior-stabilized knee TKA. ***
|
cruciates are resected & AP stability is provided by the conformity of the components & by a central tibial spine
|
|
|
Describe the mobile-bearing knee TKA. ***
|
polyethylene insert that articulates with the femoral component and with the metallic tibial tray. Intended to reduce stress & fatigue wear.
|
|
|
What are the three types of TKA fixation? Which is most common? ***
|
- cemented
- uncemented - combination of the two known as hybrid (in hybrid fixation = tibial component is cemented & the femoral component is uncemented) - cemented is still most common method TKA |
|
|
What is the recent trend for TKAs with regards to incisions? What is the benefit? ***
|
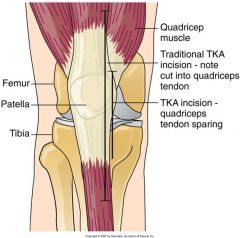
- more recent trend is for minimally invasive surgical approach
- no or little quadriceps cut - skin incision 3-5” vs. 8-12” - it appears to result in: --- less pain & blood loss --- a shortened hospital stay --- improved ROM/strength --- less time on crutches or walker |
|
|
What is the theory behind preoperative exercise before TKA? ***
|
- may help some patients
- the better conditioned a patient is before surgery the better they may perform after surgery |
|
|
What are some general aspects of postoperative rehabilitation after TKA? ***
|
- tailored to the individual
- educate the patient & family - weight bearing is usually FWB but some surgeons may limit weight bearing when a biologic fixation is used - often limited weight-bearing if certain conditions are present: ---severe osteoporosis --- fracture --- concomitant osteotomies, or bone grafts --- if it is a revision TKA - contact surgeon if there is any doubt about weight bearing status |
|
|
What are the milestones of function to be achieved post TKA? ***
|
- ambulation with an assistive device
- independent transfers - achievement of ROM - initiation of strengthening - understanding the HEP |
|
|
If there is doubt or uncertainty regarding the patient's weight-bearing status, what is it assumed to be? ***
|
- assume NWB until proven otherwise
(better to err on the side of caution) |
|
|
Describe the initial rehabilitation plan for a patient post TKA. ***
|
- focus is on tissue healing & reducing pain and inflammation
- continuous passive motion (CPM) facilitates early knee flexion - combination pneumatic compression/cryotherapy - aggressive rehab to gain knee flexion while controlling pain & inflammation --- passive knee flexion and extension --- active heel slides and supine wall slides --- forward & backward pedaling on a stationary bike --- rolling back & forth on a rolling stool (guard patient) (my take: since we are instructed not to put patients on stools, should find a rolling armchair) |
|
|
Post TKA, what movement is essential for a normal gait pattern and for efficient function of the LEs? How can this be achieved? ***
|
- full knee extension
- lie prone on plinth with knee and lower leg hanging off edge--let gravity work or may use weights - sit in chair with feet propped up on stool (may or may not place weight on knee) - pull to straighten knee vs. T-band - backward walking on land or in a pool |
|
|
What is arthrofibrosis with respect to post-TKA sequelae? How is it prevented? ***
|
- a process that occurs when diffuse scar tissue or fibrous adhesions form within or around a joint
- prevent with gentle patellar and scar mobilization after the incision site is stable to promote functional ROM - mobilization is performed in all planes (superior-inferior and medial-lateral) |
|
|
What effect does decreased superior mobility of the patella have post TKA? ***
|
it interferes with the quadriceps muscles' ability to straighten the knee and may result in an extensor lag
|
|
|
What effect does decreased inferior mobility of the patella have post TKA? ***
|
it interferes with the patient's ability to achieve full flexion of the knee
|
|
|
What is an extensor lag? What may cause it? ***
|
- occurs when range of active extension is less than the range of passive extension
- decreased superior mobility of the patella post TKA |
|
|
What benefits may post-TKA NMES have? ***
|
when used with active contraction of the quadriceps it will recruit a greater portion of type II fibers
|
|
|
What other modalities/tactics may be used for post-TKA quadriceps facilitation? ***
|
- biofeedback
- tactile stimulation |
|
|
What are some other post-TKA interventions? What should be avoided? ***
|
- quad sets
- SLRs - open-chained LE exercises progressed as tolerated (add hip abduction/adduction and hamstring curls) - as strength increases and pain decreases add closed chain exercises: --- mini-squats --- front & lateral step-ups --- stool pulls (probably better wheeled armchair pulls) --- lunges as tolerated --- stationary bike, pool therapy and walking program may be added - avoid squats and leg press performed at 90 degrees of flexion - avoid high impact activities |
|
|
What is a TSA? ***
|
- total shoulder arthroplasty
- involves replacement of both the glenoid and the humeral head |
|
|
What is a shoulder hemiarthroplasty? ***
|
replacement of the humeral component of the shoulder only
|
|
|
What is a constrained TSA? ***
|
- a TSA in which the joint is hinged or locked in some way, thus reducing the available motions
- provides stability at the cost of mobility |
|
|
What is an nonconstrained TSA? ***
|
a replacement that more closely resembles the human shoulder and its available motions
|
|
|
Which TSA is more common, a constrained or nonconstrained? ***
|
nonconstrained
|
|
|
How are the humeral and glenoid portions repaired in a TSA? ***
|
- the humeral component is either press-fit or cemented
- the glenoid portion is always cemented (as it really has nothing to hang on to--the glenoid fossa is flat) |
|
|
Which types of patients most often undergo TSAs? ***
|
most performed on patients with:
- OA - RA - avascular necrosis or - post-traumatic fractures |
|
|
Why do patients often wait to undergo TSA? ***
|
- mainly because it is an arm, and doesn't affect their ability to ambulate
- they typically wait until they are really limited in ADLs before undergoing TSA |
|
|
What is a 4-part fracture? ***
|
a fracture in which the humeral head snaps off the shaft and additionally breaks into three pieces (greater tuberosity, lesser tuberosity, and humeral head)
|
|
|
Describe a reverse TSA. What is the advantage ***
|
- a TSA in which the humeral and glenoid portions are reversed (i.e., the portion screwed into the scapula is rounded and the humeral portion is cupped)
- reverse TSAs seem to stay in place better and have increased ROM (of course, this also reverses the arthrokinematics of the joint to concave on convex) |
|
|
Upon what does the outcome of a TSA depend? ***
|
- chiefly on the status of the rotator cuff
- if the infraspinatus or subscapularis is involved, the outcome is poorer--less stable |
|
|
What muscles typically affect the success of TSA operations? ***
|
- infraspinatus
- subscapularis the outcome of the TSA will be poorer if these muscles are weakened/degraded--repair won't be as stable |
|
|
TSAs primarily ______ _____ rather than improve other symptoms. ***
|
relieve pain
|
|
|
Which patients tend to get the best ROM results from TSAs? ***
|
patients with
- OA or - osteonecrosis (average of 140˚ flexion & 45˚ of ER) |
|
|
What are some general considerations for post-TSA patients? ***
|
- while the shoulder is not a weight bearing joint, it still achieves joint compressive loads equal to the weight of the arm when it is abducted
- the glenohumeral joint is quite unstable because there is little contact between the bones & because it is subjected to shear forces in many directions - stability in the shoulder is achieved through appropriate tension of the soft tissues - the shoulder is prone to posterior instability especially with shoulder elevation & horizontal adduction (easier to sublux with posterior movement & posterior instability) |
|
|
Describe the timeframe and therapeutic exercise/rehabilitation program for a patient in the initial stages post TSA. ***
|
- day 1 or 2
--- PROM --- supine PROM flexion, PROM/AAROM into external rotation to a limit of 40˚, keep elbow bent rather than extended --- pendulum exercises (Codman’s – using body to move arm—straight line and circles) in standing --- progress into sitting AAROM as soon as possible, if rotator cuff is involved, perform ER with cane so pt does the assist - patient will be in a sling for at least 2 weeks--they need to take arm out often and perform ROM to the distal joints (elbow flex/ext/pron/sup, wrist flex/ext/deviations, fingers flex/ext etc.) precaution: passive external rotation to 40˚ and active internal rotation are limited for the first 4 -6 weeks; also no lifting/holding anything |
|
|
What is the time frame and which exercises are included in the second phase of interventions for patients post TSA? ***
|
- 10-14 days postoperatively--outpatient PT
- as patient can show shoulder control during supine exercises, progress to upright functional ROM activities while stressing increased ROM: --- wall walking --- cane or wand activities (supine) and --- pulleys - after about 6 weeks, strengthening starts with: --- isometrics in various angles --- scapular stabilizations --- scapular strengthening – rowing motions, serratus anterior strengthening, scapular clocks (move scapula up, down, in, out) & table top activities such as weight shifts (resting on hand) Precautions: - rowing motion should only go as far back as the mid-coronal line of the body - instruct your patient that when strengthening the rotator cuff, pain-free motion below 90˚ of flexion with NO weight (resistance) can be performed throughout the day - lifting, pulling, or pushing with the extremity should be avoided until instructed by the surgeon - initially, all shoulder flexion movement should be done with the elbow flexed |
|
|
What ROM limitations are to be taken with a post-TSA patient? ***
|
limits are on:
- passive external rotation to 40˚ and - active internal rotation are limited for the first 4 -6 weeks; also |
|
|
How should a post-TSA patient be progressed? ***
|
progress activities; may use:
- manual resistance - hand weights - elastic bands - aquatic therapy elastic bands should be used primarily at midrange, where it is safest patient should continue with HEP of stretching and strengthening |
|
|
What is a TEA, and when are they typically used? ***
|
- total elbow arthroplasty
- useful when conservative management of a painful or unstable elbow caused by OA or RA is unsuccessful |
|
|
What are the four main designs of TEA? ***
|
- constrained
- semiconstrained - unconstrained - resurfacing - currently a semiconstrained hinge type and an unconstrained surface replacement are used most often |
|
|
Most common TEA ***
|
currently a
- semiconstrained hinge type and an - unconstrained surface replacement are used most often |
|
|
What is the primary goal of TEA? ***
|
relief of pain
|
|
|
What is the typical life expectancy of a TEA? ***
|
generally they last 8-15 years
|
|
|
What is the main functional complication post TEA? ***
|
difficulty gaining elbow extension, which can limit ADLs such as rising from a chair by pushing on the armrests
|
|
|
Describe the timeframe and therapeutic exercise/rehabilitation program for a patient in the initial stages post TEA. ***
|
- cryotherapy with compression to decrease swelling.
- rehabilitation begins when patient is able to remove arm from extension splint (about 5-7 days post op after semiconstrained TEA) - splint worn at night and between exercise sessions for 6 weeks after surgery - AAROM begun on day 7 – flexion-extension as well as pronation & supination at 90 degrees of elbow flexion--elbow kept close to the body during all exercises - AROM & NMES for the biceps & triceps at 2 weeks for semiconstrained |
|
|
Describe the timeframe and therapeutic exercise/rehabilitation program for a patient in the later stages post TEA. ***
|
- after 6 weeks the extension splint is discontinued
- ROM exercises can performed away from the body - light resistance to elbow - ADLs to increase strength |
|
|
What precautions should be taken with a post-TEA patient (especially unconstrained)? ***
|
- unconstrained: splinting between 30-90 degrees of flexion recommended to prevent dislocation & promote implant stability
- PROM & AAROM limited to between 30-150 degrees of flexion - aggressive PROM should be avoided - HEP should be performed many times each day - for first 2-3 months post TEA: lifting limited to 1-2 lbs and thereafter a life-long limit of 5 lb is imposed. |
|
|
After total elbow arthroplasty, which movement of the elbow is the hardest to regain and maintain? ***
a. flexion b. extension c. supination d. pronation |
b. extension
|
|
|
After total shoulder replacement that does NOT require the repair of the supraspinatus muscle, only the subscapularis is violated. How does this impact the initial stages of rehabilitation? ***
a. no precautions necessary b. limited passive external rotation and active internal rotation per surgeon c. limited passive internal rotation and active external rotation per surgeon d. limited passive external rotation. |
b. limited passive external rotation and active internal rotation per surgeon
|
|
|
After a posterior approach total hip arthroplasty, which of the following precautions is NOT required to prevent dislocation? ***
a. limiting flexion of the hip to less than 90 degrees b. limiting hip adduction c. limiting hip internal rotation d. limiting hip external rotation |
d. limiting hip external rotation
|
|
|
A patient who has undergone a total joint replacement of the hip complains of increased leg swelling, calf pain, and shortness of breath. You suspect which of the following? ***
a. pneumonia b. prosthetic loosening c. deep vein thrombosis d. decreased aerobic capacity and postoperative pain |
c. deep vein thrombosis
|
|
|
After a right total hip arthroplasty, your patient exhibits a Trendelenburg gait. You notice that his hip drops on the left side. In order to correct this, you must do which of the following? ***
a. strengthen the right hip abductors b. strengthen the left hip adductors c. strengthen the left hip abductors d. strengthen the right hip adductors |
a. strengthen the right hip abductors
|
|
|
The most important difference between the minimally invasive total knee replacement and the traditional total knee replacement is which of the following? ***
a. the type of implant b. the limited incision into the quadriceps muscle c. the limited skin incision d. the method of fixation of the implant to the bone |
b. the limited incision into the quadriceps muscle
|
|
|
After total knee arthroplasty, what is the optimal amount of flexion range of motion needed for a patient to rise comfortably from a chair? ***
a. 90 degrees b. 75 degrees c. 105 degrees d. 95 degrees |
c. 105 degrees
|
|
|
What is the most important factor in normalizing gait after a total knee arthroplasty? ***
a. obtaining more than 95 degrees of flexion b. full extension c. normal (5/5) quadriceps strength d. normal (5/5) hip abduction strength |
b. full extension
|
|
|
Patients with which disease process tend to achieve the most active ROM after total shoulder arthroplasty? ***
a. rotator cuff tear b. rheumatoid arthritis c. osteoarthritis with functioning rotator cuff and deltoid d. osteoarthritis with a nonfunctioning deltoid |
c. osteoarthritis with functioning rotator cuff and deltoid
|
|
|
Which of the following is NOT an indication for arthrodesis? ***
a. quadriceps femoris paralysis b. chronic osteoarthritis c. unstable joint from neurological disease d. avascular necrosis e. chronic osteomyelitis |
b. chronic osteoarthritis
|
|
|
What are connective tissue dysfunctions? ***
|
- a group of diseases that generally share the clinical and pathological features of widespread inflammation
- chronic systemic inflammatory conditions with an autoimmune etiology |
|
|
What is another term for connective tissue dysfunctions? ***
|
rheumatic diseases
|
|
|
How many rheumatic diseases are there? ***
|
over 100
|
|
|
What can all rheumatic diseases/connective tissue dysfunctions cause? ***
|
arthritis
|
|
|
What characterizes all rheumatic diseases/connective tissue dysfunctions? ***
|
- chronic pain
- progressive damage to joints and soft tissues resulting in functional impairment typically - widespread inflammation - chronic systemic inflammatory conditions with autoimmune etiology |
|
|
What is SLE? ***
|
systemic lupus erythematosus
|
|
|
What is systemic lupus erythematosus? What potentially causes it? ***
|
- an autoimmune disease that results from the body producing antibodies directed against its own tissue
- possibly genetic, hormonal, environmental, drug induced |
|
|
What are the most common clinical features of SLE? ***
|
- most common symptoms: fatigue & arthralgia (joint pain)
|
|
|
Besides fatigue and arthralgia, what are some other systemic signs and symptoms of SLE? ***
|
systemic manifestations:
- symmetrical arthritis most often at knees, wrists, & interphalangeal joints, generally not deforming - avascular necrosis (bone death due to poor blood supply) frequently bilateral & asymptomatic; possibly caused by corticosteroid use - fever - malaise - weight loss - anorexia - myalgias: muscle tenderness & weakness |
|
|
What types of skin conditions/rashes may accompany SLE? ***
|
- rash on malar region of face (butterfly-shaped)
- rash on trunk & UEs - discoid symptoms – chronic, scaly, & scarring rash to sun exposed areas - mouth or nose sores - purpura (purple splotches that can become wounds) - livedo (bluish mottling of skin legs/hands) |
|
|
Besides the fatigue, arthralgia, skin conditions and systemic signs/symptoms, what other conditions may an SLE patient experience? ***
|
- alopecia (hair loss)
- Raynaud’s phenomenon - panniculitis (inflammed fatty tissue at abdomen) - kidney disease (lupus nephritis) - proteinuria (protein in urine) - anemia, leukopenia (decrease in # of WBCs) - cardiopulmonary - pleurisy or pericarditis - neuropsychiatric: seizures, stroke, HA, psychosis, most common is depression |
|
|
What is RA? ***
|
rheumatoid arthritis
|
|
|
What is rheumatoid arthritis? ***
|
- chronic, systemic inflammatory disease of unknown etiology
characterized by - symmetrical polyarthritis of peripheral joints - morning stiffness - malaise - fatigue - periods of remissions and exacerbations |
|
|
What causes the damage in RA? ***
|

- inflammation and tissue destruction caused by antigen-presenting cells and T cells
- increased expansion of T cells stimulates synovial secretion - increased synovial secretion causes synovial proliferation called pannus which destroys articular cartilage and bone |
|
|
What are the diagnostic criteria (7) used for classifying rheumatoid arthritis?
How many need to be present for a positive diagnosis? *** |
1. morning stiffness at joints lasting at least one hour (which contradicts the "articular manifestations of RA" slide which stated 2 hours)
2. arthritis of 3 or more pairs of joint areas 3. arthritis of hand joints--at least 1 area swollen in wrist, MCP, or PIP joint. 4. symmetric arthritis 5. rheumatoid nodules (fatty tumors, different from OA nodes), over bony prominences (usually elbow or Achilles’) or extensor surfaces 6. serum rheumatoid factor – positive (about 80% test positive) 7. radiographic changes typical of RA at hand and wrist the patient has RA if they exhibit 4 of the 7 criteria note: criteria 1-4 must be present for AT LEAST 6 weeks |
|
|
What are some of the joint-specific manifestations of RA in the UEs? ***
|
shoulder
- synovitis of glenohumeral joint with inflammation throughout the area - erosions and superior subluxation fairly common - loss of flexion and abduction elbows - to minimize pain, patients may hold the joint in flexion and pronation - this causes a flexion contracture & functional impairment if loss of as little as 30 degrees of extension (functional difficulties such as push off/sit-to-stand) wrist - zig zag deformity – radial deviation at wrist and ulnar deviation at fingers. fingers - angle of pull changes to cause: - swan-neck deformity – PIP hyperextension with MCP & DIP flexion - boutonniere deformity – DIP hyperextension (due to avulsion/rupture of extensor hood) & PIP flexion |
|
|
What are some of the joint-specific manifestations of RA in the LEs? ***
|
hips: rarely involved in RA
knees: - effusions at knee cause it to distend and stretch the joint capsule and contribute to ligamentous attenuation (breakdown) - possible Baker’s cyst may occur (popliteal) foot and ankle: - synovitis at ankle, talonavicular and/or MTP joints - inflammation of talonavicular joint causing pronation & eversion and flattening of longitudinal arch - claw toes – MTP weakness leading to plantar subluxation of metatarsal heads & cock-up deformity of toes - hallux valgus: bunion first toe |
|
|
What may happen to tendons with RA patients? ***
|
they may rupture due to persistent inflammation and breakdown
|
|
|
What are some of the joint-specific manifestations of RA in the spine? ***
|
- C1 – C2 instability or subluxation possible
- initially pain & headache - may lead to UE paresthesias & LE weakness - paralysis or death if not stabilized |
|
|
What are the common articular manifestations of rheumatoid arthritis? ***
|
- morning stiffness usually lasting at least 2 hours (which contradicts the "diagnostic criteria for classifying RA" slide which stated 1 hour)
- synovial inflammation - structural damage - joint pain and swelling - persistent synovitis may lead to loss of cartilage, bony erosion and ultimately, irreversible structural damage |
|
|
What are the common systemic and nonarticular manifestations of rheumatoid arthritis? ***
|
systemic:
- fatigue - malaise - subjective weakness - depression - low-grade fever cutaneous - nodules can be a soft or firm mass, and tend to develop on extensor surfaces (especially forearm) - Sjogren’s syndrome – dry mouth and eyes - some may show photosensitivity, Raynaud’s phenomenon, or vasculitis |
|
|
What are spondyloarthropathies? Name three. ***
|
- a group of inflammatory diseases involving the synovium, entheses (where tendon/ligament attaches to bone), spine, and peripheral joints
include: - Ankylosing Spondylitis - Reactive Arthritis (Reiter’s syndrome) - Psoriatic Arthritis |
|
|
With what antigen are spondyloarthropathies strongly associated? ***
|
HLA-B27 (protein on surface of WBCs) antigen
|
|
|
Describe Ankylosing Spondylitis (AS). ***
|
- chronic systemic inflammatory disorder, primarily causing enthesitis (inflammation at site of ligament insertion into bone) and synovitis of the spine
- causes fibrosis and then ossification of the ligaments and joint capsule, ultimately causing ankylosis (fusion) - "squaring” of the vertebrae occurs, the term “bamboo spine" describes the appearance when AS has caused complete fusion of the vertebral column - almost always involves the sacroiliac joints (SI) - progresses from SI toward cervical spine. |
|
|
What are some symptoms of AS? ***
|
- low back pain and stiffness that worsens with inactivity
- fatigue - malaise - weight loss - low-grade fever and - anorexia |
|
|
When is the typical onset of AS, and in which gender is it more common? ***
|
- onset in late adolescence and early adulthood (average age of 26)
- much more common in men |
|
|
Describe the typical posture of an AS patient. ***
|
- forward head
- protracted and internally rotated shoulders - increased thoracic kyphosis - flattened lumbar spine - also lumbar lordosis that fails to reverse with forward bending |
|
|
What is the other name for Reactive Arthritis? ***
|
Reiter's Syndrome
|
|
|
Describe Reactive Arthritis/Reiter's Syndrome. ***
|
- systemic disease that begins suddenly (within days or weeks) after a venereal infection or gastroenteritis
- prognosis good, usually fully resolves in 3-12 months - joint pain and inflammation most often at hips, knees, and ankles - plantar fascia and Achilles tendon enthesopathy can impair ambulation - skin rash occurs on the sole of the foot or the palm of the hand; flaky plaques that become scaly |
|
|
What are the signs and symptoms of Reactive Arthritis/Reiter's Syndrome? ***
|
- joint and eye inflammation
- enthesopathy - cutaneous lesions - malaise - fever and - fatigue - joint pain and inflammation most often at hips, knees, and ankles - plantar fascia and Achilles tendon enthesopathy can impair ambulation - skin rash occurs on the sole of the foot or the palm of the hand; flaky plaques that become scaly |
|
|
Describe Psoriatic Arthritis (PA). ***
|
- autoimmune inflammatory disorder involving chronic activation of T helper-1 cells
- affects skin and joints - psoriatic skin lesions usually precede joint manifestations - usually affects large joints like the knees and one or two DIP or PIP joints in an asymmetrical pattern - in women it mainly affects the small joints of the hands, feet, wrists, ankles, knees, and elbows - men show more involvement of the DIP with changes in the nail bed or asymptomatic and asymmetrical spinal arthritis - when it starts in childhood it usually resolves but progression is worse if there is a family history and extensive skin involvement - 1/3 of patients also develop eye inflammation - enthesitis occurs where the Achilles tendon and the plantar fascia attach to the calcaneus - spondylitis may occur resulting in fusion - nails show pitting, may crack, turn brownish yellow or separate - psoriatic skin lesions on extensor surfaces of knees & elbows |
|
|
Describe Polymyalgia Rheumatica (PMR). ***
|
- systemic inflammatory disorder that primarily causes pain and stiffness in the neck, shoulder, and pelvic girdle muscles
- other symptoms include: --- low-grade fever --- fatigue --- anorexia --- anemia --- weight loss --- headaches and --- depression - type II (fast twitch) muscle fiber atrophy (musculoskeletal type) - giant cell arteritis (GCA) is a vasculitis of the medium and large arteries that commonly occurs with PMR - 10% can have sudden loss of vision - 2/3’s have claudication of the jaw muscles (pain with chewing), loss of taste, tongue numbness & pain |
|
|
Describe Polymyositis (PM) and Dermatomyositis (DM). ***
|
- rare autoimmune diseases that cause chronic inflammation in striated muscle
- proximal weakness affecting the muscles of the hips, and shoulders - neck flexors weak in 50% - ocular and facial muscle weakness occur but are very rare - symptoms: --- muscle pain --- morning stiffness --- symmetrical weakness --- fatigue --- malaise --- chills --- fever or --- weight loss generally come on rapidly - they may appear briefly and then remit spontaneously without treatment |
|
|
Describe Scleroderma (Sc). ***
|
- autoimmune connective tissue disease causing fibrosis of skin and internal organs
- 10 year survival rate about 40% - 60%. - two types: limited and diffuse --- limited or localized Sc primarily affects skin distal to the elbows and knees, the lungs, and sometimes skin of face or neck --- diffuse Sc or systemic sclerosis is more aggressive; fibrosis of the internal organs, musculoskeletal structures, blood vessels, GI tract, lungs, heart and kidneys, rash over trunk & proximal extremities. |
|
|
What are the two types of Sc and how does each affect the patient? ***
|
- two types are limited and diffuse
--- limited or localized Sc primarily affects skin distal to the elbows and knees, the lungs, and sometimes skin of face or neck --- diffuse Sc or systemic sclerosis is more aggressive; fibrosis of the internal organs, musculoskeletal structures, blood vessels, GI tract, lungs, heart and kidneys, rash over trunk & proximal extremities. |
|
|
What are the major and minor criteria required for a Scleroderma diagnosis? ***
|
- major required criteria is skin thickening proximal to the MCP joints
- minor criteria include --- sclerodactyly (sclerosis & tapering of fingers) --- digital ischemia --- abnormal skin pigmentation --- pulmonary fibrosis (primary cause of death in Sc is pulmonary hypertension) --- Raynaud’s phenomenon and --- lower esophageal dysphagia & dysmotility |
|
|
What is the primary cause of death for most Sc patients? ***
|
pulmonary hypertension
|
|
|
What is gout? ***
|
a condition caused by deposition of uric acid crystals in the joints and connective tissue
|
|
|
What are the three stages of gout? ***
|
1. hyperuricemia (high uric acid in the blood)
2. acute intermittent gout 3. chronic tophaceous gout |
|
|
How does gout progress through its three phases? ***
|
- initially -- warmth, swelling, pain, and erythema at a single joint
(most often starts at first MTP) - progresses to intermittent acute attacks - after 10 yrs. → chronic tophaceous gout |
|
|
What is pseudogout? ***
|
- similar to gout but is caused by deposition of calcium pyrophosphate dehydrate (CPPD)
- mostly deposited in cartilage which results in bouts of acute joint inflammation, usually in knees |
|
|
What joint is most often affected by pseudogout? ***
|
knees
|
|
|
How many subtypes of Juvenile Rheumatoid Arthritis are there? Name them. ***
|
3 subtypes
- Pauciarticular - Polyarticular - Systemic-onset JRA |
|
|
Which is the most common type of JRA? ***
|
pauciarticular
|
|
|
What is Pauciarticular JRA? ***
|
- most common form of JRA
- most common in boys - involves 4 or fewer joints - knees involved 75% of time - asymmetrical with enthesitis common - tends to be milder than other types - responds well to treatment - may remit in a few years |
|
|
Which type of JRA is most common in boys? ***
|
Pauciarticular JRA
|
|
|
What joint is most commonly involved in Pauciarticular JRA? ***
|
the knee
|
|
|
What is Polyarticular JRA? ***
|
- second most common type
- more common in girls - involves 5 or more joints in a symmetrical pattern - may involve 20 or more joints including cervical spine & TMJs |
|
|
Which type of JRA is more common in girls? ***
|
Polyarticular JRA
|
|
|
What is Systemic-onset JRA? ***
|
characterized by:
- high-spiking fevers twice daily - rash on trunk & proximal extremities - feeling ill, fatigued, & experiencing loss of appetite |
|
|
What types of testing are done on patients with chronic rheumatic disorders? ***
(per the chart on page 68) |
- grip-strength test
- thumb to index strength test - time to walk 50 feet test - 6-minute walk test - Jepson Hand Function test, Grip Ability test, Grip Function test, Arthritis Hand Function test - Button test - Timed-stand test - Keitel Index |
|
|
What is the purpose of the Grip-strength test and how is it carried out? ***
(per the chart on page 68) |
- measurement of hand, wrist, and forearm strength
- patient squeezes the cuff of a sphygmomanometer inflated to 30 mm Hg as hard as possible; the highest level on the mercury column of 3 attempts is recorded (may also be measured with a Martin Vigorimeter) - motivation, handedness, pain threshold, and muscle weakness will affect scores, as will involvement of any joint from the elbow to the hand - grip strength measures have been shown in clinical trials to be sensitive to change in disease activity |
|
|
What is the purpose of the Thumb-to-index strength test and how is it carried out? ***
(per the chart on page 68) |
- measurement of hand and finger function
- measured with a Martin Vigorimeter - motivation, handedness, pain threshold, and muscle weakness will affect scores, as will involvement of any joint from the elbow to the hand - grip strength measures have been shown in clinical trials to be sensitive to change in disease activity |
|
|
What is the purpose of the Time to walk 50 feet test and how is it carried out? ***
(per the chart on page 68) |
- measurement of LE function
- individual walks 50 feet on a flat surface using any aides or assistive devices; time is recorded to the nearest tenth of a second - motivation can affect performance; low reliability, insensitive to changes in disease activity |
|
|
What is the purpose of the 6-minute walk test and how is it carried out? ***
(per the chart on page 68) |
- field test of fitness
- measures the distance the patient can walk in 6 minutes - motivation can affect performance; low correlation with standard laboratory tests of physical fitness; sensitive to change in exercise clinical trial in fibromyalgia; little information available for other disorders |
|
|
What is the purpose of the Jepson Hand Function test, Grip Ability test, Grip Function test, and Arthritis Hand Function test and how are they carried out? ***
(per the chart on page 68) |
- various measurements of hand function tested in persons with arthritis; activities tests are based on ADLs
- specific tasks (e.g., picking up cards, pouring water from a jug, writing) are performed in the presence of evaluator - may be used in clinical trials of specific hand treatments, following hand surgery, and in long-term outcome studies; some tests require special equipment |
|
|
What is the purpose of the Button test and how is it carried out? ***
(per the chart on page 68) |
- measurement of hand function that can be used in clinical practice
- standard board with 5 buttons; patients are timed while they unbutton and button using right and left hands separately, with scores from both hands averaged - motivation is an important factor; useful in disorders affecting hand function (e.g., RA) |
|
|
What is the purpose of the Timed-stand test and how is it carried out? ***
(per the chart on page 68) |
- measurement of LE function
- measures number of seconds it takes the patient to stand up and sit down 10 times from a chair using only the LEs - motivation, age, and nonmusculoskeletal co-morbid conditions may affect scores; sensitivity to change has not been determined |
|
|
What is the purpose of the Keitel Index and how is it carried out? ***
(per the chart on page 68) |
- measurement of UE and LE extremity function with emphasis on ROM
- measures performance of 24 standard tasks requiring peripheral and axial joint motion; performance is evaluated by a trained observer; takes 10-15 minutes to complete - motivation may be a factor; time and personnel to observe and score tasks are a factor in its use; scale is sensitive to short-term change |
|
|
What are some precautions mentioned for examination of patients with chronic rheumatic disorders? ***
|
- manual strength testing is not recommended for unstable joints
- watch for signs of crepitus (don’t push through it; it shows that the joint is already worn) - ask about functional levels instead (eating and eliminating most commonly) |
|
|
What is the most successful approach for interventions for patients with chronic rheumatic disorders? ***
|
multidisciplinary
includes: - patient education for self-management - cognitive behavioral interventions - medical interventions and - physical interventions |
|
|
Upon what factors does the successful treatment of patients with chronic rheumatic disorders depend? ***
|
success depends on:
- ongoing participation in home program - appreciation of the principles of pain management, rest, and joint protection - use of adaptive equipment for ambulation and ADLs - energy conservation and - proper use of splinting |
|
|
What types of activities constitute patient education for patients with chronic rheumatic disorders? ***
|
- individual or group instruction
(most success seen with the Arthritis Foundation's “Arthritis Self-Management Program”) covers: - disease pathology - drug therapy - exercise - use of joint protection devices - orthopedic perspectives - psychological counseling - dietetics and - information about unproven remedies |
|
|
What types of activities constitute rest and joint protection interventions for patients with chronic rheumatic disorders? ***
|
- both general rest and joint-specific rest are key components for management of chronic rheumatoid disorders
- balance between activity & rest is required during acute/active stages of inflammatory arthritis - it is important to remember not to push through—that will make things worse - sleep 8–10 hours nightly and rest 30–60 minutes each day - pacing of activities and planning of schedules is needed to avoid fatigue and joint flares - joint-specific rest needed to provide periods of unloading (usually via splinting) and promote function and activity despite joint swelling and pain - patient may modify activities, use assistive devices/adaptive equipment, and/or use protective or supportive splinting (e.g., extra-depth shoes, lever handles on faucets, etc.) |
|
|
What types of physical agents are useful in interventions with patients with chronic rheumatic disorders? ***
|
- heat: most commonly hot packs, warm water, and paraffin baths
(precaution: when there is acute inflammation heat may cause symptom exacerbation, and could further damage the joints) - cold: cold packs, ice massage, and cold water immersion may be applied - heat and cold: heat before exercise followed by cold afterward have been shown to improve function and decrease pain - electrotherapy: good research focused on wrist & hand shows that TENS can reduce pain and improve function - low-level laser therapy (LLLT): shown to reduce pain and morning stiffness and increase ROM in patients with RA |
|
|
What types of exercise are beneficial in interventions with patients with chronic rheumatic disorders? ***
|
generally follow recommendations for health & fitness in the apparently healthy population:
- whole body, repetitive activities most days of week for 30 minutes at 55-70% of MHR or RPE of 12-13/2-4 - cardio, 3-5 days of the week for 20-30 minutes at 70-85% of MHR or RPE of 14-16/4-7 - resistance, 2-3 days of the week (alternate days), 8-10 exercises with resistance sufficient to fatigue after 8-12 reps (10-15 reps if over 50 to 60 years old or frail) - flexibility, 2-3 days a week (minimally), 3-4 reps per stretch, hold for 10-30 seconds |
|
|
What precaution must be remembered when applying heat to joints of patients with chronic rheumatic disorders? ***
|
when there is acute inflammation heat may cause symptom exacerbation, and could further damage the joints
|
|
|
What precautions must be remembered when instructing a patient with a chronic rheumatic disorder in an exercise program? ***
|
do only 1–2 reps through ROM daily when in acute inflammatory phase
|
|
|
What are some general guidelines regarding exercise for patients with chronic rheumatic disorders? ***
|
- joint immobilization may lead to weakening of cartilage and periarticular structures
- regular joint motion and intermittent weight bearing that occurs with many forms of exercise may enhance joint health. - still need to adhere to general and joint specific recommendations for pacing and rest - precaution: do only 1–2 reps through ROM daily when in acute inflammatory phase. |
|
|
What types of ROM exercises are beneficial for patients with chronic rheumatic disorders? ***
|
- AROM and AAROM (avoid overstretching inflamed tissues)
- AROM and relaxation techniques (meditation, breathing exercises, contract/relax exercises) shown to produce functional gains & decrease pain in patients with RA - patient must be reminded that the goal is slow gains, not quick results |
|
|
What types of strengthening exercises are beneficial for patients with chronic rheumatic disorders? ***
|
- isometric and dynamic strengthening with light weight or elastic resistance at a level of 50% - 80% of maximal voluntary contraction (MVC) 2–3 times/week
- patient must be reminded that the goal is slow gains, not quick results |
|
|
What are the purposes of isometric and dynamic muscle conditioning exercises in patients with chronic rheumatic disorders? ***
|
isometric
- minimize atrophy - improve tone - maintain and increase static strength and endurance - prepare for dynamic and weight-bearing activity dynamic - maintain and increase dynamic strength and endurance - increase muscle power - improve function - enhance synovial blood flow - promote strength of bone and cartilage |
|
|
What are the recommendations for isometric and dynamic muscle conditioning exercises in patients with chronic rheumatic disorders? ***
|
isometric
- perform at functional joint angles - breathe normally, do not hold breath - intensity of 70% or less of MVC - duration: 6 seconds - frequency: 5-10 reps daily dynamic - able to perform 8-10 reps against gravity before increasing resistance - use functional movements - modify ACSM guidelines as appropriate |
|
|
What are the precautions for isometric and dynamic muscle conditioning exercises in patients with chronic rheumatic disorders? ***
|
isometric
- decreased muscle blood flow - may increase intraarticular pressure - may increase BP dynamic - may increase biomechanical stress on unstable or malaligned joint - need for power grip |
|
|
What type of aerobic exercise is beneficial for patients with chronic rheumatic disorders? ***
|
- moderate to hard (60% - 85% of max HR), 3 times weekly for 30–60 minutes
- can be land- or water-based - still need to protect weight bearing joints (good shoes, protective surfaces, pick activities without forceful impact to joints) |
|
|
How is aquatic exercise beneficial to patients with chronic rheumatic disorders? ***
|
exercise performed in water can
- reduce pain - increase muscle relaxation - reduce joint compression and - improve functional status - community-based water aerobic classes noted to be very successful |
|
|
What criteria apply to exercise programs for children with juvenile RA? ***
|
- children may safely participate in either aquatic or land-based exercises without causing exacerbation
- aquatic or land-based exercise 2x/ week x 6 weeks may reduce disease activity and improve endurance - JRA children may benefit more from land-based rather than aquatic exercise - weight bearing exercise is necessary for development of healthy bone growth - individualized & supervised strengthening exercise appears safe & effective in children as young as 8 - individualized exercise may be more appropriate for children with severe disease, whereas children with mild-moderate disease may benefit from group exercise programs - children with mild disease should be able to participate in most sport with proper screening and physical conditioning. However, highly competitive contact sports should be avoided during active disease. |
|
|
What criteria apply to exercise programs for patients with spondyloarthropathies? ***
|
- focus of treatment is postural reeducation to prevent forward flexion of the spine
- keep spine erect - flexibility exercises to the spine, hips, & shoulders emphasizing erect posture and maintaining the ability to lift arms overhead - breathing exercises - stretching: pectorals & hip flexors - strengthen: posterior spine extensors, scapular retractors, hip extensors, abdominal strengthening to help support the spine & improve posture |
|
|
What criteria apply to exercise programs for patients with scleroderma? ***
|
- maintain joint ROM and soft tissue flexibility
- focus on face, especially the mouth to help patient to eat & brush teeth and the fingers to maintain the ability to perform fine motor skills and ADLs - mouth stretching and oral augmentation exercises - hands: stretching & paraffin |
|
|
The patient history helps in selection of interventions for patients with connective tissue dysfunctions because of which of the following? ***
a. many of these pathologies are chronic and systemic, thus lifestyle adaptations need to be developed b. selection of interventions is based on previous experiences and outcomes c. the behavior of symptoms may vary based on activity level, medications, and compensatory mechanisms d. it identifies patient education opportunities to help them become self-managers e. all of the above |
e. all of the above
|
|
|
Joint manifestations of RA include which of the following? Mark all that apply. ***
a. acute synovitis b. morning stiffness c. swan-neck deformities d. Heberden’s nodes e. joint erosions and juxta-articular osteoporosis |
a. acute synovitis
b. morning stiffness c. swan-neck deformities |
|
|
Scleroderma is characterized by which of the following? Mark all that apply. ***
a. fibrosis of the skin b. history of silicone breast implants c. fibrotic changes in the blood vessels, musculoskeletal structures, and internal organs, including pulmonary, renal, cardiac, and gastrointestinal systems d. exposure to organic solvents and drugs like bleomycin e. symptoms including Raynaud’s phenomenon, reduction in flexibility, and fatigue |
a. fibrosis of the skin
c. fibrotic changes in the blood vessels, musculoskeletal structures, and internal organs, including pulmonary, renal, cardiac, and gastrointestinal systems d. exposure to organic solvents and drugs like bleomycin e. symptoms including Raynaud’s phenomenon, reduction in flexibility, and fatigue |
|
|
The three subtypes of JRA based on clinical manifestations and course within the first 6 months include which of the following? Mark all that apply. ***
a. Pauciarticular JRA b. Systemic JRA c. Monoarticular JRA d. Polyarticular JRA e. Juvenile ankylosing spondylitis |
a. Pauciarticular JRA
b. Systemic JRA d. Polyarticular JRA |
|
|
In patients with spondyloarthropathies, Schober’s test measures which of the following? ***
a. intrinsic tightness b. forward head positioning c. spinal mobility d. ulnar drift e. hip mobility |
c. spinal mobility
|
|
|
Polymyalgia rheumatica commonly occurs concomitantly with which of the following? ***
a. headache from giant cell arteritis b. rigidity in the spine and neck c. proximal muscle weakness d. presence of the HLA-B27 antigen |
a. headache from giant cell arteritis
|
|
|
Successful management of polymyositis and dermatomyositis includes which of the following? Mark all that apply. ***
a. rest b. vigorous exercise when CPK levels are high c. strength training when CPK levels are low d. conditioning activities to improve functional abilities e. ice |
c. strength training when CPK levels are low
d. conditioning activities to improve functional abilities |
|
|
Interventions that can be effective for managing symptoms and loss of function associated with inflammatory arthritis include which of the following? ***
a. joint protection b. patient education c. ultrasound d. aquatic therapy e. exercise f. all of the above |
f. all of the above
|
|
|
Studies on children with arthritis demonstrate that physical activity has which of the following effects? Mark all that apply. ***
a. a decrease in disease activity/severity b. more affected joints c. increased mobility and strength d. increased aerobic fitness e. improved function |
a. a decrease in disease activity/severity
c. increased mobility and strength d. increased aerobic fitness e. improved function |
|
|
What is the pathology behind localized inflammation? ***
|
- preferred practice pattern 4E: Impaired joint mobility, motor function, muscle performance, and range of motion associated with localized inflammation
- similar to connective tissue dysfunction except focuses on localized inflammation rather than systemic - wide range of stimuli can provoke localized inflammation, resulting in inflammatory response and possibly chronic inflammation |
|
|
What are the components of the functional joint complex? ***
|
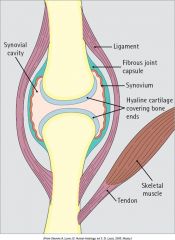
- synovial fluid helps nourish articular cartilage and lubricate joints and tendon sheathes
- articular cartilage is avascular and has a limited capacity for repair - cartilage is protected from wear by a form of self-lubrication - movement through physiological range of motion helps nourish the articular cartilage - damage to muscles, tendons, ligaments around a joint and subchondral bone can cause increased wear on the cartilage |
|
|
Describe osteoarthritis (OA). ***
|
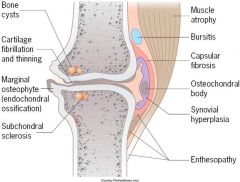
- degenerative joint disease.
- most common type of arthritis in the world - knees most common joint affected - characterized by breakdown of the cartilage and periarticular bone changes (osteophyte formation and subchondral sclerosis) |
|
|
What is the most common type of arthritis in the world? What joint does it most commonly affect? ***
|
- osteoarthritis, OA, degenerative joint disease
- the knees |
|
|
Progression of OA ***
|
- microcracks lead to
- fissuring and pitting down to subchondral bone and - fragments of cartilage may fall into the joint, causing - mild synovial inflammation, leading to - full thickness loss of articular cartilage, prompting the body's - attempts to regenerate causing osteophyte formation at joint margin |
|
|
What are the primary risk factors for OA? ***
|
- increased age
- obesity - hip injury - congenital or developmental hip disorders and - genetic predisposition to the disorder |
|
|
What is bursitis? ***
|
- bursae are fluid-filled sacs located at numerous points throughout the body
- may become inflamed by --- trauma --- overuse --- rheumatoid arthritis --- crystal arthropathies (e.g., gout) or --- infection |
|
|
What is capsulitis? ***
|
inflammation of the joint capsule, most commonly glenohumeral joint (frozen shoulder)
|
|
|
What is a ligament sprain? ***
|
- stretch or tear of a ligament
- graded according to severity --- first-degree = stretch of the ligament --- second-degree = partial tear of ligament --- third-degreee = full tear of ligament |
|
|
What is a muscle strain? ***
|
- stretch or a tear of a muscle
- most common injury in sports - typically occur near the myotendinous junction of muscles crossing two or more joints - graded according to severity --- first-degree = stretch of the muscle or tendon --- second-degree = partial tear of muscle or tendon --- third-degreee = full tear of muscle or tendon |
|
|
What is tendinitis? ***
|
- acute inflammatory condition of the tendon and its surrounding structure that may lead to degeneration
- often, persistent low-grade inflammation and gradual weakening of tissues until microtrauma occurs |
|
|
What are the risk factors for tendinitis? ***
|
- sudden increase in physical activity
- age (peak age 30-50) - reduced vascularity - abnormal joint alignment - strength deficits or imbalances |
|
|
What are the five grades of tendinitis? ***
|
can be divided into five stages of severity:
--- grade 1 - least severe pain, occurs only with activity, doesn't affect performance, generalized tenderness, disappears between sessions --- grade 2 - minimal pain with activity, local tenderness, does not interfere with activity intensity or duration --- grade 3 - interferes with activity but usually disappears between sessions, localized tenderness --- grade 4 - interferes with intensity of training and doesn't disappear between sessions, significant pain, crepitus, swelling, tenderness --- grade 5 - most severe, interferes with sports and ADLs, symptoms are chronic or recurrent, tissue changes and altered muscle function |
|
|
What is tenosyovitis? ***
|
inflammation of the synovial sheath
|
|
|
What data is collected in the patient history portion of the examination for a patient with localized inflammation? ***
|
- patient’s description of their current condition and its evolution
- description of the activity when the symptoms started - nature of a patient’s symptoms - visual analog scale can be used to establish a baseline for symptom severity - work history: --- repetitive movements --- exposure time --- environmental risk factors --- posture-related risk factors --- psychological stresses |
|
|
What data is collected in the tests and measures portion of the examination for a patient with localized inflammation? ***
|
- posture should be tested
- girth and volumetric measurements can be used to detect joint effusion, edema, or muscle atrophy - measures of ROM can help identify inflamed structures - assessment for local warmth, swelling and redness, temperature changes, tenderness, and muscle atrophy or hypertrophy - assessment of motor performance is necessary - degree and direction of joint play tested and compared to uninvolved side - standardized walking tests (2-minute, 6-minute, 12-minute), shuttle (use of sound to pace, e.g., metronome); incremental shuttle walking test, and self-paced - patients with localized inflammation involving the lower extremities may have reduced gait speed or a noticeable limp as a result of pain - patient’s ergonomics and body mechanics at work, home, and in the leisure environment are tested |
|
|
What are the findings in the evaluation, diagnosis, and prognosis of patients with local inflammation? ***
|
Preferred practice pattern 4E: Impaired joint mobility, motor function, muscle performance, and ROM associated with localized inflammation – patients have:
- temperature changes - joint swelling - loss of ROM - altered function - joint line tenderness - fluctuance – feels “boggy,” longstanding edema, accumulation of pus - localized pain when the inflamed tissues are stressed |
|
|
What interventions are undertaken during the acute stage of local inflammation? ***
|
- controlling the inflammatory process (PRICE)
- minimizing further injury - promoting healing - minimizing associated signs and symptoms |
|
|
What interventions are undertaken during the restorative stage of local inflammation? ***
|
- establishing full pain-free ROM
- increasing or restoring flexibility - improving or restoring cardiovascular and muscular fitness and performance - addressing any other neuromuscular deficits |
|
|
What interventions are undertaken during the acute stage of osteoarthritis? ***
|
PRICE (protect, rest, ice, compression, and elevation) during the acute stage of localized inflammation
|
|
|
What interventions are undertaken during the chronic stage of osteoarthritis? ***
|
- thermotherapy to decrease stiffness in patients with chronic localized inflammation
- superficial heat - ultrasound - E-stim (negative polarity decreases edema, but never place directly over the edema—burn risk) - TENS for pain - iontophoresis (improved ROM & decreased pain) - manual therapy - therapeutic exercise |
|
|
What are the criteria and precautions for implementation of therapeutic exercise with a patient with OA? ***
|
- therapeutic exercise – may not change course but may lessen the pain and disability.
- begin slowly and progress gradually, avoiding rapid or repetitive movement of the affected joints - joint should be moved through it’s full ROM at least several times each day to prevent contractures - isometrics to maintain strength. - low-impact exercises to large muscle groups - walking, bicycling, swimming, at a RPE of 11 – 16 - stretching of major muscle groups with a 10-30 second hold, at least 3 times, 2-3 times /wk (to keep ROM in worn-down joint; not going to do heavy resistive exercise; except if impending TKA – you want the mm as strong as possible before surgery) - PNF - wearing a neoprene support sleeve at knee is recommended for increased proprioception & feeling of stability |
|
|
What types of orthotics are used with a patient with OA and why? ***
|
braces, taping, and splints are recommended to limit the load imposed on the affected structures
|
|
|
What types of patient education are used with a patient with OA and why? ***
|
- information about pathology
- methods to reduce inflammation and pain - joint protection strategies - methods to increase function (exercise and ADL training) - modification of the home and work environment - coping strategies (pain, mobility) |
|
|
How are joint protection and tool modification incorporated into the treatment program for a patient with OA? ***
|
- assistive devices can be used to reduce joint impact during ambulation
- an assessment of environmental barriers in the home, community and/or work is recommended |
|
|
How can pacing strategies help improve quality of life of an OA patient? ***
|
- pacing strategies can enhance energy conservation
- may allow a patient whose symptoms are exacerbated by their current level of activities to complete those activities and achieve their goals without further injury |
|
|
List 7 common joint protection principles. ***
|
- respect pain
- avoid improper postures or positions - avoid staying in one position for a long time - use the strongest and largest joints and muscles for the job - avoid sustained joint activities - maintain muscle strength, joint ROM, and conditioning - use assistive devices and/or splints |
|
|
What psychosocial factors should be considered/included in the treatment program for patients with localized inflammation. ***
|
psychosocial management of chronic inflammatory diseases:
- lack of cures, gradual decline, and necessity of long-term adaptation can result in stress, depression, and learned helplessness - intervention should include: --- stress management --- coping skills --- cognitive restructuring --- problem solving --- behavior modification --- altering a patient’s perception and responses to pain --- teaching the difference between harm and hurt --- educating family members about the patient’s condition |
|
|
Which of the following cells has phagocytic properties during the inflammatory stage? ***
a. fibroblast b. macrophage c. neutrophil d. permanent |
b. macrophage
|
|
|
A therapist examines a patient diagnosed with osteoarthritis who reports difficulty in performing household tasks due to stiffness and aching in the fingers. The therapist notes that the finger joints are stiff and not inflamed and includes superficial heating and exercises to decrease stiffness in the plan of care. Which of the following would be the ideal way to follow this plan of care? ***
a. perform ROM exercises followed by a hot pack. b. apply paraffin to decrease the stiffness and follow this with ROM exercises. c. teach daily active ROM exercises to be done at the end of each day. d. teach home use of paraffin. |
b. apply paraffin to decrease the stiffness and follow this with ROM exercises.
|
|
|
A patient with arthritis has stiff finger joints that are inflamed and warm. The therapist selects joint rest as part of the plan of care. Which of the following would be the ideal way to follow this plan of care? ***
a. begin an aquatics program. b. increase the resistance and decrease the number of repetitions of the patient’s exercise program. c. select a splint that supports the involved joints. d. instruct the patient to perform several repetitions of their active ROM daily. |
c. select a splint that supports the involved joints.
|
|
|
A therapist examines a patient with a diagnosis of frozen shoulder syndrome. The examination revealed the following PROM impairments of the left shoulder: external rotation 10 degrees, flexion 60 degrees, and abduction 40 degrees. The history and physical examination help the therapist to conclude the patient is in the descending phase of the pathology and she plans to use ultrasound and mobilization to increase the ROM. The most important aspect of this patient’s home program is which of the following? ***
a. ROM exercises b. strengthening exercises c. cryotherapy d. understanding and following joint protection principles |
a. ROM exercises
|
|
|
What is the most prevalent chronic condition in the U.S., as well as the leading cause of disability
|
arthritis
|
|
|
SLE is three times higher in what population than would be expected by their representation in the general population?
|
African Americans
|
|
|
What percentage of SLE patients are female?
|
90%
|
|
|
Why are women typically more predisposed to autoimmune disease?
|
it is thought that since estrogens promote immune responses and increase the production of autoantibodies, that female sex hormones promote both disease activity and etiology
|
|
|
Ankylosing spondylitis (AS)
|
a form of inflammatory arthritis that has a predilection for the SI joints, axial spine, and ligamentous/tendinous insertions
|
|
|
Arthritis
|
- encompasses over 100 types of rheumatic diseases
- literal translation means inflammation of the joint |
|
|
Cytokines
|
proteins secreted by a variety of cells to help regulate immunological responses (e.g., interleukin, tumor necrosis factor, lymphokines and interferon)
|
|
|
Dactylitis
|
inflammation of a finger or toe
|
|
|
Dermatomyositis
|
diffuse inflammatory disease of striated muscle that leads to symmetric proximal muscle weakness with a dermatological component
|
|
|
Effusion
|
excess fluid in the joint resulting from joint irritation or inflammation of the synovium
|
|
|
Enthesitis
|
inflammation where ligaments and tendons attach to bone
|
|
|
Inflammatory arthritis
|
systemic arthritis that involves inflammation of the synovium of the joint
|
|
|
Interleukin-1 (IL-1)
|
substance from monocytes and macrophages important int the acute phase response
|
|
|
Gout
|
disease characterized by acute episode of arthritis resulting from the deposition of uric acid crystals at the joint or in surrounding tissues
|
|
|
Lupus
|
a chronic inflammatory autoimmune disease that may affect the skin, joints, and internal organs
|
|
|
Mauskopf
|
loss of facial expression as the result of tightening/tautness of the skin resulting from scleroderma
|
|
|
Myositis
|
inflammatory disease of striated muscle
|
|
|
Pannus
|
excessive proliferation of synovial and granulation tissue that invades joint surfaces
|
|
|
Polymyalgia rheumatica (PMR)
|
condition characterized by stiffness and pain at the shoulder girdle without weakness; usually seen in women over 50 in conjunction with an elevated erythrocyte sedimentation rate (ESR)
|
|
|
Polymyositis
|
diffuse inflammatory disease of striated muscle that leads to symmetric proximal muscle weakness
|
|
|
Pseudogout
|
synovitis caused by the deposition of calcium pyrophosphate dehydrate crystals resulting in arthritis; articular chondrocalcinosis
|
|
|
Psoriatic arthritis
|
spondyloarthropathy with concomitant psoriasis
|
|
|
Raynaud's phenomenon
|
an intermittent vasoconstriction of the distal small arteries, arterioles and capillaries that results in blanching, erythema, and cyanosis of the hands
|
|
|
Reactive arthritis
|
spondyloarthropathy with enteric or venereal infectious trigger (also known as Reiter's syndrome)
|
|
|
Reiter's syndrome (RS)
|
triad of arthritis, conjunctivitis and urethritis (also known as reactive arthritis)
|
|
|
Rheumatoid arthritis (RA)
|
systemic disease characterized by inflammation of the joint synovium
|
|
|
Schober's test
|
a measurement of spinal mobility in patients with spondyloarthropathy
|
|
|
Sclerodactyly
|
sclerosis and tapering of the fingers in progressive systemic sclerosis
|
|
|
Scleroderma
|
a chronic disease of unknown etiology that causes sclerosis of the skin and organs (GI tract, heart, lungs, and kidneys) and arthritis
|
|
|
Sjogren's syndrome (SS)
|
disease of the lacrimal and parotid glands resulting in dry eyes and mouth; frequently occurs with RA, SLE, and scleroderma
|
|
|
Spondyloarthropathy
|
inflammation of the spine and sacroiliac joints; describes a category of diseases that includes ankylosing spondylitis, reactive arthritis/Reiter's syndrome, and psoriatic arthritis
|
|
|
Systemic lupus erythematous (SLE)
|
systemic inflammatory disease characterized by small-vessel vasculitis and a diverse clinical presentation
|
|
|
Systemic sclerosis
|
a chronic disease of unknown etiology that causes sclerosis of the skin and organs (GI tract, heart, lungs, and kidneys) and arthritis
|
|
|
Tenosynovitis
|
inflammation of the synovial lining of the tendon sheaths
|
|
|
Tenosynovitis
|
inflammation of the synovial lining of the tendon sheaths
|
|
|
Tophi
|
deposits of uric acid crystals around the joints
|
|
|
Uveitis
|
inflammation of the iris, ciliary body, and choroids, or the entire uvea
|
|
|
Vasculitis
|
inflammation of the blood or lymph vessels
|
|
|
Xerostomia
|
dry mouth
|
|
|
Xerophthalmia
|
dry eyes
|
|
|
Arthrodesis
|
the surgical fusion of the bony surfaces of a joint with internal fixation such as pins, plates, nails, and/or bone graft
|
|
|
Arthrofibrosis
|
increased fibrous tissue in a joint that limits ROM
|
|
|
Arthropathy
|
any disease or abnormal condition affecting a joint
|
|
|
Arthroplasty
|
any reconstructive joint procedure with or without an implant that is designed to relieve pain and restore motion
|
|
|
Avascular necrosis
|
death of bone cells as a result of loss of a blood supply
|
|
|
Cruciate-retaining (or -sparing) knee
|
a total knee replacement in which the posterior cruciate is retained for stability
|
|
|
Extensor lag
|
when the knee's PROM into extension exceeds the AROM into extension
(this term is synonymous with quadriceps lag) |
|
|
Fascial arthroplasty
|
removal of the bone from one or both of the articular surfaces of a joint and allowing a fibrotic scar to form in the space that remains
|
|
|
Hemiarthroplasty
|
replacement of one side of a compartment of a joint (e.g., replacing only the humeral portion of the shoulder joint)
|
|
|
Methylmethacrylate
|
epoxy cement used in cemented total joint surgery to attach the implant to the bone surface
|
|
|
Mobile bearing knee
|
a total knee replacement in which a polyethylene insert articulates with the femoral component and the metallic tibial tray
|
|
|
Osteolysis
|
softening or destruction of bone
|
|
|
Posterior stabilized knee
|
a total knee replacement in which both cruciate ligaments are excised and the stability of the knee depends on the implant
|
|
|
Resection arthroplasty
|
removal of one or both articular surfaces of a joint (also known as excisional arthroplasty)
|
|
|
Angiogenesis
|
development and formation of blood vessels
|
|
|
Fibroblast
|
connective tissue cell that secretes proteins (collagen, glycosaminoglycans, elastin, and glycoproteins) to help form the extracellular matrix; have the ability to differentiate into other cells (e.g., osteoblasts, chondrocytes, and myofibroblasts)
|
|
|
Macrophages
|
large cells whose primary role is phagocytosis and removal of pathogens; they produce a variety of substances (e.g., ascorbic acid, fibronectin, lactic acid, and angiogenesis growth factor) to promote angiogenesis and wound debridement
|
|
|
Fluctuance
|
abnormal condition in which the area under the skin being palpated feels "boggy" or viscous; indication of pus accumulating, especially if the surrounding area is indurated
|
|
|
Myofibroblasts
|
fibroblasts that differentiated to resemble smooth muscle (contains myofilaments) for the specialized function of approximating (contracting) the borders of an injury
|
|
|
Neutrophils (granulocytes)
|
phagocytic white blood cells
|
|
|
Osteonecrosis
|
necrosis of the bone (also avascular necrosis and ischemic necrosis of the bone)
|
|
|
Osteitis pubis
|
noninfectious inflammation of the pubis
|
|
|
Trendelenburg gait
|
disorder of the hip abductors caused by weakness or an inhibition; during the stance phase, the body weight is transferred to the affected side and the hip abductors on the affected side are unable to support the pelvis, resulting in a pelvic drop or tilt toward the swing limb
although typically seen in adults, this gait pattern may be seen in children with a slipped capital femoral epiphysis |

