![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
75 Cards in this Set
- Front
- Back
|
What is Therapeutic Exercise?
(definition) |
Systematic & planned performance of:
a. bodily movements b. postures c. physical activities |
|
|
Intent of Therex?
|
Provide patients/clients with means to:
a. remediate/prevent impairement b. improve, restore, enhance physical function c. prevent/reduce healt-related risk factors d. optimize overall health status, fitness, sense of well-being |
|
|
What is a "Patient" (vs Client)
|
with impairments and functional limitations DIAGNOSED by a PT and is receiving PT care to improve function and prevent disability
|
|
|
What is a "Client" (vs Patient)
|
no diagnosed dysfunction, engages in PT services to:
-promote health and wellness -to prevent dysfunction |
|
|
Aspects/Components of Physical Function:
|
1. Balance
2. Cardiopulmonary fitness / endurance 3. Coordination 4. Flexibility / Mobility 5. Muscle Performance 6. Neuromuscular control 7. Postural control/stability/equiliibrium 8. Stability |
|
|
Balance
(define) |
ability to align body segments against gravity to maintain or move body within available base of support without falling
|
|
|
Balance requires input/output from what systems?
|
sensory and motor systems
|
|
|
Coordination
(define) |
correct timing and sequencing of mm firing along with appropriate intensity of mm contraction leading to effective initiation, guiding, and grading of movement
|
|
|
Flexibility / Mobility
(define) |
Flexibility: ability to move freely w/o restriction
Mobility: ability to structures and segments of body to move and be moved to allow for ROM in functional activities. |
|
|
2 types of Mobility are...
|
Passive: dependent on soft tissue extensibility (contractile and non-contractile)
Active: requires neuromuscular activation |
|
|
Extensibility (of soft tissue)
(define) |
ability of soft tissue to return to its original length after a stretch has been released
|
|
|
Muscle Performance
(define) |
the ability to produce tension and do physical work
|
|
|
3 Factors of Muscle Performance
|
1. Strength:
2. Power 3. Muscle Endurance |
|
|
Neuromuscular Control
(define) |
Interaction of sensory and motor systems to correctly sequence coordinated movement.
Must respond to proprioceptive/kinesthetic info |
|
|
Postural control, postural stability & equilibrium
|
used interchangeably with static or dynamic balance
|
|
|
Stability
(define) |
ability of the neuromuscular system to hold a proximal or distal body segment in a stationary position or to control a stable base during superimposed movement
|
|
|
Agonist
|
muscles that act as prime movers
|
|
|
Antagonists
|
muscles that act in direct opposition to prime movers
|
|
|
Synergist
|
muscles that assist prime movers during functional movement patterns
fatigue easily |
|
|
Therapeutic Exercise Interventions
|
Wide variety of techniques
Chosen based on patient’s impairments, limitations and/or disability |
|
|
Safety Factors:
(as pertains to patient) |
-Medications: 3+ = risk of falling
-Patient unaccustomed to physical exertion: take vitals -Environment: Adequate space and proper surfaces -Accuracy with which exercise is performed -co-morbidities |
|
|
Safety Factors:
(as pertains to PTs) |
proper body mechanics
proper safety attire (gloves, masks) |
|
|
Disablement Models (generic definition)
|
Relationship between a person’s health status and function... includes interrelationships between:
-Pathology -Impairments -Functional limitations -Disabilities, handicaps, societal limitations |
|
|
Early models of Disablement include:
|
Nagi and International Classification of impairments, disabilities and handicaps (ICIDH)
|
|
|
New Framework for Disablement model:
|
International Classification of Functioning, Disability and Health (ICF)
- activity at the center; less emphasis on disease, more emphasis on function -everything relates to activity |
|
|
Three major categories of Impairments
|
Anatomic
Psychological Physiological |
|
|
Anatomic Impairments
(define or explain) |
-an abnormality or loss of structure
-CANNOT be remedied with PT -Modifications can be made to function in light of anatomic impairments ex: hip anteversion, structural genu verum, loss of limb |
|
|
Psychological Impairments
(define or explain) |
-CANNOT be remedied with PT
-can offer a listening ear, or advise to see other professionals |
|
|
Physiological Impairments
(define or explain) |
-an alteration in any physiologic function
-PTs can impact this most ex: reduced Force production, reduced endurance, reduced mobility, pain, altered movement patterns,etc. |
|
|
Types of Physical Impairments (ICF breakdown)
(list) |
Musculoskeletal
Neuromuscular Cardiovascular Integumentary |
|
|
Musculoskeletal
Physical Impairment (ICF breakdown) |
pain, mm weakness, decreased mm endurance, limited ROM, joint hypermobility, faulty posture, mm length/strength imbalances
|
|
|
Neuromuscular
Physical Impairment (ICF breakdown) |
pain, impaired balance or postural stability, incoordination, delayed motor development, abnormal tone (flaccid or too much tone in mm), ineffective/inefficient functional movement strategies
|
|
|
Cardiovascular
Physical Impairment (ICF breakdown) |
decreased aerobic capacity, impaired circulation, pain with sustained activity (intermittent claudication; ex: riding a bike with impaired circulation)
|
|
|
Integumentary
Physical Impairment (ICF breakdown) |
skin hypomobility (immobile from scar tissue)
|
|
|
Primary/Direct Impairments
|
results from active pathology or disease
ex: shoulder impingment: result in pain decrease ROM Primary may lead to Secondary Impairments |
|
|
Secondary Impairments
|
-comes from the primary impairment, or pathology-
-can't just treat symptoms, have to look for cause ex: shoulder impingment: postural asymmetry because of altered use of upper extremity |
|
|
Composite Impairments
|
combination of primary/secondary
ex: cast for ankle break, causes issues with balance, weakness, asymmetry, etc.. |
|
|
Functional/Activity limitations
(component of the disablement model) |
-Person has difficulty or cannot perform tasks of daily living
-Refers to the person -Goal of therapy to remediate ex: feeding, dressing, making meals, going to store |
|
|
Participation Restriction/Disability
(explain) |
any restriction or inability to perform socially defined roles and tasks expected of an individual within a socialcultural and physical environment
|
|
|
3 Categories of Disability Prevention
|
Primary
Secondary Tertiary Therex works on all 3 areas of prevention |
|
|
Primary Disability Prevention
|
activities like health promotion
to prevent disease in at-risk population |
|
|
Secondary Disability Prevention
|
early diagnosis and reduction of severity/duration of existing disease
|
|
|
Tertiary Disability Prevention
|
use of rehab to reduce/limit progression
improving chronic or irreversible conditions |
|
|
Risk Factors to Disablement Models
|
Exist before the onset of a health condition
-Biological -Lifestyle -Physical environment -Socioeconomic |
|
|
Clinical Decision Making
(define) |
Process of reasoning and critical thinking that involves making judgments and determinations in the context of patient care
|
|
|
Clinical Prediction Rules (CPR)
|
treatment based on probabilities
|
|
|
Evidence Based Practice
(define) |
Use of current best evidence in making decisions about the care of an individual patient
|
|
|
6 steps of Evidence Based Practice
|
-Identify problem
-Search literature -Analyze evidence -Integrate evidence with expertise -Incorporate with patient management -Assess outcomes |
|
|
Patient Management Model
(list 5 components) |
1. examination
2. evaluation 3. diagnosis 4. prognosis 5. interventions |
|
|
Examination (pertaining to Patient Management Model)
(list 3 components) |
-History
(current/past info, subjective/objective) -Systems Review (vitals) -Tests & Measures (Functional outcome measures) |
|
|
Evaluation (pertaining to Patient Management Model)
(define) |
Interpretation of collected and relevant data
Fundamental to making a proper diagnosis of dysfunction and prognosis of functional outcomes May also suggest additional testing is needed PT or another practitioner |
|
|
Diagnosis Process
(define) |
Sequence of actions and decisions
-Leads to formation of diagnostic hypothesis -Classifies dysfunction 2 Categories |
|
|
2 Categories of Diagnosis
(define) |
1. Process: data collection through examination
-organization of data to reach an impairment based diagnosis 2. Category: a grouping that identifies and describes patterns or clusters of physical findings -pt’s may have differnet pathologies, but share similar impairments in the same categories |
|
|
Diagnostic Category
(define) |
Identifies patterns or clusters of physical findings
Describes impact of a condition at the system level Preferred practice patterns |
|
|
Cluster
|
a set of observations or data that frequently occur as a group for a single patient
|
|
|
Syndrome
|
an aggregate of signs and symptoms that characterize a given disease or condition
|
|
|
Prognosis
|
Prediction of patient’s optimal level of function
-As result of treatment plan Anticipated length of time needed -2x week for 6 weeks Plan of Care -Integral component of prognosis |
|
|
Goal Setting
(define and key points) |
Collaboration and negotiation between patient and therapist
Make goals patient centered -Helps the patient be an active participant in the rehab process Make them functional |
|
|
Interventions
(define) |
Any purposeful interaction a PT has that directly relates to a patient’s care
|
|
|
Interventions
(list 3 categories) |
-coordination, communication, and documentation
-procedural interventions -patient-related instructions |
|
|
Patient Related Instruction
|
As physical therapists we:
-Educate -Facilitate change -Motivate Spans 3 domains of learning -Cognitive -Affective -Psychomotor |
|
|
Outcomes
|
A way to measure quality, efficacy and cost-effectiveness of services
tools: oswestry, NDI, ROM, Muscle performance |
|
|
Effective Exercise Instruction
|
Positive relationship with patient
Know patient’s learning style Identify patient’s attitudes toward exercise Less complicated exercises first? |
|
|
Concepts of Motor Learning
|
Integration of motor learning principles
Internal processes for skilled movement or task through practice -Relatively permanent retention Modifies way sensory information is central nervous system is processed -Cannot be directly observed |
|
|
Types of Motor Tasks
(3 types) |
Discrete task
-Any activity with discreet beginning, end Serial task -Series of discreet movement done in a particular sequence (eating with fork, brushing teeth) Continuous task -Repetivitive movements (walking riding bike, stairs) |
|
|
Conditions & Progression of Motor Tasks
(4 task dimension) |
1) environment in which the task is performed.
What are you trying ith person to make more challenging, incorporate tasks 2) The inter-trial variability of the environment that is imposed on the task. 3) Need for the patient’s body to remain stationary or move during the task. 4) Presence or absence of manipulating of objects during the task |
|
|
environment conditions of motor learning
(chart) |
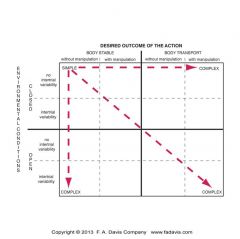
Top left, is simple, bottom
Closed environment: objects, surface around patient don’t move, no rolling chairs Open environment: object, support surface, other people, can all be in motion (moving bus, crowded stairways) Inter trial variability: absent or none (nothing is changing); like walking on a single surface, no change Some inter trial variability: similar task but changing the environment Body stable: simple task (maintain posture) Body transport: rolling over in bed, or any type of transfer (table to chair, sit-stand, walking/jumping) Manipulation of objects: ( walking with free hands, vs cup of coffee; or walking on crowded sidewalk) |
|
|
Stages of Motor Learning
(3 stages) |
Cognitive
-Patient or you, have to think about each component of taks (seq to complete task) Associative -Less mistakes, can fine tune task, patient req less feedback and may be able to make corrections before they occur Autonomous -Final stage: movements are automatic, don’t need to pay attention, can maybe do simult other tasks -Propably won’t see patients in this stage, cuz they are likely discharged |
|
|
Variables That Influence Motor Learning
|
Understanding
-Interest in task -The more you explain, and meaningful, then more likely learning and compliance will occur Attention -Outcomes versus details -How they focus on it; a person that knows the outcome, they will learn better (why they need to do the exercise) Demonstration -Showing what is expected, pre-practice (verbal instructions) |
|
|
Practice
|
Most important variable to learning a motor skill
Skill acquisition and retention affected by: -Amount -Type -Variability Part versus whole practice -Part: effective in early stage of motor development (practice most difficult stages first) -Whole: better for continuous / serial tasks |
|
|
Practice Order (for motor skills)
|
blocked
-best during cognitive, sit-stand reps, repeat/predictable random -change task slightly, sit-stand from differing heights random-blocked -task done more than once, random parts |
|
|
Feedback (source, focus, timing)
|
source:
intrinsic (internal) extrinsic (external; PTs feedback) focuse of feedback: -knowledge of performance: about quality of activity -knowledge of results: how this will help them Timing/Freq: -concurrent (tactile, verbal) -immediate post-response (after each trial) -delayed/summary: |
|
|
Frequency of Feedback
|
extrinsic: less is better
constant: (concurrent) during or after each rep variable/intermittent: promotes retention of skill vs constant summary: recap, most effective at ASSOCIATIVE stage of learning |
|
|
Adherence to Exercise
|
Designing a program a patient will follow
-ex. exercise length/duration Patient related factors: -tailer to patient, gender sometimes plays a role Impairment related factors: -acute (short time) vs chronic (do forever) Program related factors -appeal to interest of patient, need equipment?... |
|
|
Considerations in Exercise Prescription
|
Stage of healing
Tissue irritability and symptom stability Patient’s time and willingness to participate Time between PT visits |

