![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
115 Cards in this Set
- Front
- Back
|
What is described as an acute demyelination when it reaches its highest point, in less than 4 weeks?
|
Nadir
|
|
|
What is the most frequent cause of acute flaccid paralysis worldwide that is also among the most dramatic neurologic emergencies?
|
Guillain-Barre Syndrome (GBS)
|
|
|
What is the mechanism of GBS or acute inflammatory demyelinating polyradiculoneuropathy?
|
Affects nerve roots and peripheral nerves leading to motor neuropathy and flaccid paralysis (AIDP)_
|
|
|
What do macrophages do in GBS or AIDP?
|
They attack and strip myelin sheaths, sometimes the nerves are then remyelinated.
|
|
|
Which disease is caused by an autoimmune response directed against Schwann cell membranes?
|
AIDP
|
|
|
Which disease in purely motor?
|
Acute Motor Axonal Neuropathy (AMAN)
|
|
|
T/F DTR and sensory nerves are lost with AMAN.
|
F
|
|
|
Is GBS ascending or descending paralysis?
|
Ascending
|
|
|
Is Miller Fisher Syndrome (MFS) ascending or descending paralysis?
|
Descending
|
|
|
What are the differences between AMAN and AIDP?
|
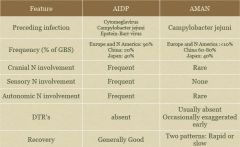
|
|
|
MFS usually affects which muscle first?
|
Eye muscles
|
|
|
What are the 3 main signs of MFS?
|
Opthalmoplegia
Ataxia Areflexia |
|
|
Which disease is more severe than AMAN and affects both motor and sensory fibers?
|
Acute Motor and Sensory Axonal Neuropathy (AMSAN)
|
|
|
What is recovery like with AMSAN?
|
Often slow and incomplete
|
|
|
What is the disease as described by the following:
most rare variant of GBS often accompanied by encephalopathy high mortality rate (cardiovascular involvement) recovery is slow and incomplete impaired sweating, no fear formation, photophobia, dry nasal and oral mucosa, peeling of skin, nausea, dysphagia, constipation/diarrhea lethargy, fatigue, headache, decreased initiative orthostasis, blurred vision, abdominal pain, disturbed micturition |
Acute Panautonomic Neuropathy
|
|
|
What are cardinal clinical features of GBS?
|
Progressive, rapidly evolving
Fairly symmetric muscle weakness accompanied by absent or depressed DTR weakness Usually starts in proximal leg (10% begin in arms or facial muscles) |
|
|
What are ANS symptoms of GBS that occur in 50% of patients?
|
Low cardiac output
Cardiac dysrhythmias Marked fluctuations in blood pressure |
|
|
What are sensory symptoms of GBS?
|
Distal hyperesthesias
Paresthesias Numbness Decreased vibratory and position sense Stocking-and-glove presentation not dermatomal distribution |
|
|
What percent of GBS patients have facial and oropharyngeal weakness?
|
50%
|
|
|
What percent of GBS patients have oculomotor weakness?
|
15%
|
|
|
What percent of GBS patients require assisted ventilation?
|
20-30%
|
|
|
What are characteristics of pain with GBS?
|
Prominent severe pain in lower back in AIDP
72% of pt’s report pain during the course of their illness Muscle aching typically associated with vigorous or excessive exercise Symmetrically in large-bulk mm The pain was more disturbing at night Severe burning, etc. |
|
|
What is the recovery like for GBS?
|
Varied
Gradual recovery of muscle strength 2-4 weeks after progression has stopped or the condition has plateaued 50% of pts may show minor neurological deficits and 15% may show persistent residual deficits in function 80% become ambulatory within 6 months of onset of symptoms Most common long-term deficits: weakness of anterior tib, weakness of foot and hand intrinsics, quads, gluts, fatigue and endurance 5% die |
|
|
What percent of GBS patients make an excellent/complete recovery with no
permanent damage even after a severe attack? |
70%
|
|
|
What percent of GBS patients are disabled or weak after 3 years?
|
10-20%
|
|
|
What percent of GBS patients are severly disabled and may need a wheel chair to get around?
|
5-10%
|
|
|
What are diagnostics criteria for GBS?
|
Progressive weakness and areflexia (ascending, bilateral symmetric)
Sensory involvement Cranial nerve involvement Autonomic dysfunction Absence of fever |
|
|
How do you confirm GBS?
|
Electrodiagnostic Studies
Cerebrospinal Fluid |
|
|
What is tested in the electrodiagnostic studies?
|
3 sensory nerves
3 motor nerves |
|
|
If someone has GBS, what will the CSF have?
|
High protein without increase SBC
|
|
|
What percent of patients that present with GBS have it following a benign respiratory or GI illness?
|
2/3
|
|
|
What are the 1st symptoms of AIDP?
|
Pain
Numbness Parasthesia Weakness |
|
|
What is the lowest point of AIDP?
|
2 weeks (50%) to 4 weeks (90%)
|
|
|
What are signs and symptoms of AIDP?
|
Motor, sensory and autonomic dysfunction
|
|
|
What are motor dysfunctions of AIDP?
|
Flaccid paralysis/paresis (bilateral, symmetrical)
Severe cases see mm wasting in 2 weeks Absent DTR’s (hallmark sign) |
|
|
What are sensory dysfunction of AIDP?
|
Paresthesias
Pain May have distal loss of vibration, proprioception, touch and pain |
|
|
What is the prognosis for the nadir for AIDP?
|
Some patients have a fulminating course of progress with
maximal paralysis within 1-2 days of onset 50% of patients reach the nadir (point of greatest severity) within 1 week 70% by 2 weeks 80% by 3 weeks in some cases increasing weakness continues for 1-2 months ** at 8 weeks it's considered GBS and not AIDP |
|
|
What are autonomic dysfunctions of AIDP?
|
Cardiovascular signs (Sinus bradycardia, hypertension, cardiac arrhythmias and
postural hypotension) Urinary retention Constipation (bowel paresis and ↓ gastric motility) Abnormal vasomotor tone Sialorrhea Anhidrosis |
|
|
What are general signs of AIDP?
|
Fatigue
Muscle Tenderness |
|
|
What poor prognostic factors lead to mortality with AIDP?
|
Bulbar dysfunction
Autonomic dysfunction Severe weakness Age>60 years Prolonged ventilation Hypokalemia Pulmonary infections |
|
|
What factors lead to poor functional recovery with AIDP?
|
bulbar dysfunction
autonomic dysfunction severe weakness Age>60 years prolonged ventilation hypokalemia pulmonary infections |
|
|
What are complications of AIDP?
|
Anemia
Respiratory distress Contractures Joint dislocation Anxiety/depression Cardiac Arrythmia Skin breakdown Heterotopic ossification Thomboembolism Pneumonia Aspiration Urinary retention Ileus Persistent paralysis |
|
|
What are the 2 types of immunotherapy for AIDP?
|
Plasmapharesis (plasma exchange) [PE]
Intravenous immunoglobulin (IVIG) |
|
|
When is plasmapheresis more effective?
|
If started withing 7 days of symptom onset
|
|
|
With plasmaphersis, what is the optimal number of exchanges with severe AIDP?
|
4
|
|
|
Is the risk of relapse of AIDP higher with PE or IVIG?
|
PE
|
|
|
Which immunotherapy decreases the duration of respirator dependence and the time to onset of improvement?
|
IVIG
|
|
|
What are the initial priorities for therapy with GBS?
|
Prevent contractures
Protect skin integrity ROM Pulmonary function |
|
|
What should the PT teach the family of a GBS patient?
|
Disease progression, prognosis, and treatment
ROM exercises Splinting and orthotic devices Answering any other questions |
|
|
With GBS, what should be done intially?
|
Avoid Excessive Exercise
Energy Consumption Use of adaptive equipment |
|
|
What are pulmonary issues with GBS?
|
severity of dysfunction on a wide continuum
may have trach with mask to deliver O2 need to work with team on airway mgmt! work in upright postures, increasing time out of bed assist with secretion mgmt - cough assist be aware of suction needs and methods monitor O2 sats and RR during activity breathing exercises, postural drainage, incentive spirometry be aware of aspiration risk |
|
|
What are cardiovascular concerns for GBS?
|
influenced by Autonomic system - ↑resting HR, unstable BP
risk for DVT poor functional endurance and mm endurance (REST!) work on vertical tolerance |
|
|
What kind of progression is necessary for musculoskeletal and neuromuscular rehab with GBS?
|
Graded Progression
|
|
|
What are functional mobility examples used with GBS patients?
|
Incorporate activities throughout - can break down tasks to work on strength,
balance, endurance, etc Safety - balance, sensory dysfunction Bed mobility Transfers Balance - sitting, standing, gait w/c propulsion/management Gait training |
|
|
What is the GBS disability scale?
|
0- Healthy
1- Minor symptoms or signs of neuropathy but capable of manual work/ capable of running. 2- Able to walk >10m w/o assist but incapable of manual work/running. 3- Able to walk 10m across open space with assist or assistive device 4- Confined to a bed or chair-bound 5- Requiring assisted ventilation (any part of day or night) 6- Death |
|
|
What are key differences between AIDP and chronic inflammatory demyelinating polyradiculoneuropathy (CIDP)?
|
Rate of progression
- CIDP slower, lowest point can be 4-8+ wks - Up to 20% can see periods of remission and relapse Response to treatment: - CIDP responds better to corticosteroids - Also responds to IVIg and plasmapheresis Asymmetry of symptoms more common in CIDP, except in kids Proximal mm affected as much as distal mm Motor symptom dominate more than in AIDP |
|
|
What is GBS in a "nutshell"?
|
GBS = autoimmune AIDP
Rapidly progressing symmetrical ascending weakness and sensory changes Phases Progressive: 2-4 wks Plateau: variable Recovery: 6-12 mos with 2-3 yrs for complete Early therapy correlated with ↑ recovery potential DO NOT OVER FATIGUE! |
|
|
What is the leading cause of death and disability in young adults in the US?
|
TBI
|
|
|
What percentage of falls account for TBIs? MVA? Struck against something? Assaults and violence? Other?
|
Falls: 29%
MVAs: 20% Struck against something: 19% Assaults/violence: 11% Other 13% |
|
|
How do you name lower limb orthotics?
|
First letter of each joint crossed.
Example: KAFO (Knee Ankle Foot Orthotic) |
|
|
If it is a swing phase only deficit, what orthotic would you use?
|
Leaf Spring
|
|
|
What type of orthotic is used to control rear foot and midfoot and some inversion and eversion?
|

|
|
|
Which orthotic is used to control stance phase and blocks movement of the ankle in all directions?
|
AFO
|
|
|
Which orthotic has the highest level of control below the knee and may be the most functionally disruptive?
|
AFO
|
|
|
Which type of orthotic is used to control dropfoot?
|
AFO- PLS
|
|
|
Which type of orthotic has a joint built into it?
|
AFO- Articulated Joint
|
|
|
Which type of orthotic can block PF and smooth out the 2nd half of stance phase?
|
AFO- Articulated Joint
|
|
|
Which type of orthotic has a rigid section over the proximal tibia?
|
AFO- Ground Reaction
|
|
|
Which orthotic applies an external extension moment to the knee and assists in weak quadriceps?
|
AFO- Ground Reaction
|
|
|
If a person with polio presents with weak DF, foot slap, stance valgus, and difficulty clearing during swing, which type of orthotic would you prescribe?
|
Drop Foot: PLS
Stance Valgus: AFO- Solid Ankle |
|
|
In a person with muscular distrophy that has weak DF, tight PF, and has difficulty clearing during swing, which type of orthotic would you use?
|
PLS
|
|
|
In a person with Charcot Marie-Tooth impairment that presents with DF and eversion insufficiency and has difficulty clearing during swing, which type of orthotic would you use?
|
Drop foot- PLS
Plantar flexor insufficiency: AFO Ground Reaction (Toe-off) |
|
|
If a person with myelomeningocele that has PF insufficiency, which type of orthotic would you use?
|
PF: Ground Reaction AFO
Ground Reaction with an articulated joint |
|
|
What differences would you expect
between an L4 MMC patient and an L4 complete SCI? |
Walking forces during childhood and
adolescence: Bony deformities Contractures |
|
|
What is the most common (80%) dysfunction that is prescribed bracing?
|
CVS- Equinovarus
|
|
|
With CVA- Equinovarus, which type of orthotic would you use?
|
AFO-FA with PF stop
|
|
|
Individuals with the earlier medical diagnosis of polio face the possibility of losing their ______________ and _________.
|
Functional Abilities
Independence |
|
|
After how many years does postpolio syndrome (PPS) usually occur?
|
30-40 years
|
|
|
What is the percentage of all polio survivors many experience PPS?
|
2/3
|
|
|
How does one contract acute paralytic polio?
|
Virus- from one of 3 strains of enterovirus
contaminated water/food fluelike infection <1% developed paralysis - anterior horn cell damage |
|
|
Patients with acute polio were left with which symptoms?
|
Flaccid Paralysis
- asymmetric - proximal > distal; LE > UE - Bulbar involvement (dysphagia, iron lung) Absent or diminished DTRs |
|
|
What is the mechanism of injury during polio?
|
Polio virus attacks neurons
Muscle left without innervation |
|
|
What would the functional compensation of a boy with polio look like?
|
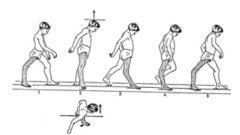
|
|
|
What is the possible recovery from acute polio recovery?
|
1. Recovery of neurons not irreversibly damaged
2. Reinnervation by collateral sprouting to orphaned muscle fibers (giant motor units) 3. Hypertrophy of innervated muscles fibers 4. Motor Learning/functional compensation 5. increased recruitment of the giant motor units |
|
|
What is the appropriate diagnosis for PPS?
|
Confirmed history of previous polio
Partial to complete mm strength loss followed by recovery stable course for at least 15 years onset of 2 or more signs and symptoms/new health problems Rule out other neurological conditions |
|
|
What are signs and symptoms of PPS?
|
New weakness (slowly progressing)
Fasciculations Cramps Atrophy Fatigue Muscle and joint pain Cold Intolderance |
|
|
What should the examination of PPS include?
|
Aerobic capacity/endurance
Assistive/adaptive devices muscle performance: MMT joint integrity/mobility ROM: tightness, contractures (what selective tightness is necessary) Environmental, home, work barriers Gait, locomotion, balance Orthotics Pain Posture: sleeping, sitting, standing, walking |
|
|
What are typical goals for PPS?
|
Prevent further decrease/progression in mm weakness - decrease the workload of muscles relative to their capacity
Increase strength if possible Decrease/minimize fatigue Minimize postural deviations Maintain and increase function, safety and quality of life Minimize gait deviations Prevent/alleviate pain |
|
|
What are possible interventions to deal with pain for PPS patients?
|
Rest
Postural corrections Cold/ice NSAID’s Orthotics ROM exercises |
|
|
What are possible interventions to deal with fatigue for PPS patients?
|
learning to manage energy
energy conservation nonfatiguing daily activities breaking up activities into parts daily rest periods including a nap short term sick leave Uncontrollable?>Disability retirement |
|
|
What are possible interventions to deal with posture and gait deviations for PPS patients?
|
Stretching - be careful not to take function away by stretching
Bracing/orthotics to support paresis (soft collars, corsets, low back supports, AFO, UE splinting/bracing) Assistive devices motorized mobility |
|
|
What are possible interventions to deal with locomtion for PPS patients?
|
(↑safety, ↑function & QOL, ↓energy expenditure, ↓fatigue, ↓ pain)
Energy conservation Assistive devices motorized mobility mvmt strategies |
|
|
What are possible interventions to deal with energy conservation for PPS patients?
|
activity analysis by type, time, distance, and intensity
breaking activities into parts frequent rest periods typical standing activities done in sitting, tall stool, rolling stool/chair reducing trips up/down stairs re-arranging kitchen, laundry, etc |
|
|
What are initial exercises that should be done with PPS patients?
|
Initial objective = ↓load on mm, eliminate pain and fatigue and build a reserve capacity
Pt’s with mm pain and fatigue are already getting too much exercise Stretching Strengthening - non-fatiguing - 1/2 intensity, 1/2 reps, double rest periods - Fatigue not > 30 minutes; no↑pain - only 3/5 or stronger muscles Cardiovascular - non-fatiguing - short intervals at 60% HR max - frequent rest periods - 1:2 work:rest ratio - Gradually progress Weight management |
|
|
What are the classifications for NRH Post-Polio?
|

|
|
|
What are the NRH Post-Polio Muscle Classifications?
|

|
|
|
How do you treat Class 1 PPS?
|
Increase strength and endurance
Stretching - increase flexibility Exercise - PRE’s w 1-2 min rests b/t sets If no cardiac or respiratory illness, then conditioning can follow ACSM guidelines |
|
|
How do you treat Class 2 PPS?
|
Increase strength in 4/5 muscles
Maintain strength in 5/5 muscles If other extremities weak then Class II muscles can be used for conditioning (compensation) Intervals with frequent rest periods Alternate exercise/rest days Gradually build intensity and duration |
|
|
How do you treat Class 3 PPS?
|
At least maintain strength; if possible, gain in mm that are deconditioned
AROM, PROM depending on strength Exercise in intervals with frequent rests; decrease pace compared with Class II Non-weight bearing exercises (pool) |
|
|
How do you treat Class 4 PPS?
|
Prevent further weakness
Decrease activity if overuse PROM, AROM depending on strength Nn-fatiguing exercise program in gravity eliminated positions or pool Carefully monitor strength!!!! Strengthening no more than 3x/week Cardio with only less affected limbs or with ADL’s Assistive devices, scooters, bracing |
|
|
How do you treat Class 5 PPS?
|
MaintainROM - PROM
Unable to use limbs for exercise Assistive devices Mechanized mobility Bracing |
|
|
What is the hallmark sign of Myasthenia Gravis (MG)?
|
Fatiguability
|
|
|
What is the pathology of MG?
|
no known causative pathogen
75% of pt’s have an abnormality of the thymus 10-15% have a thymoma antibodies to the nAChR impair the ability of ACh to bind to receptors In MG, antibodies are directed toward the nAChR at the NMJ of skeletal mm Results in: - Decreased number of functioning nAChR at the motor end-plate (blockage of ACh transmission) - Reduced postsynaptic membrane folds (immune response) - Widened synaptic cleft |
|
|
What is one way to get rid of MG?
|
Remove the thymus
|
|
|
How is MG diagnosed?
|
AChR antibody assay
EMG- shows decremental response to repetitive stimulation - Single fiber EMG is most sensitive test |
|
|
What should the exam for MG include?
|
Fatiguability
- look upward and sidewards for 30 seconds (ptosis and diplopia) - look at feet while in supine, 60 seconds - keep arms at 90 in sitting, 60 seconds - ten deep knee bends - walking 30 steps on both the toes and the heels - five sit-ups, lying down and sitting up completely |
|
|
What is the classification for MG?
|
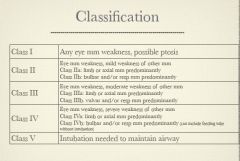
|
|
|
What are symptoms of MG?
|
asymmetrical ptosis
diplopia unstable or waddling gait change in facial expression dyshagia shortness of breath dysarthria |
|
|
Where would you typically see weakness with MG?
|
arms
hands fingers legs neck |
|
|
How do you treat MG?
|
Acetylcholine esterase inhibitors
Immunosuppression - prednisone (may be combined with ACh esterase inhibitors) - IVIG - Plasmaphoresis Thymectomy |
|
|
What percentage of patients with MG see improvement with a thymectomy?
|
85%
|
|
|
What are complications of MG?
|
Respiratory failure
Dysphagia Complications secondary to drug tx - long-term steroid use - osteoporosis, cataracts, hyperglycemia, HTN - gastritis, peptic ulcer disease - pneumocystis carinii |
|
|
What is the prognosis for MG?
|
Without treatment: 1/3 improve, 1/3 progress, 1/3 die
40% have ONLY occular symptoms only 16% of those with occular symptoms at onset remain exclusively occular at the end of 2 years. |
|
|
What should the patient with MG modify?
|
Diet:
- dysphagia: thicken liquids Activity - pt’s should be advised to be as active as possible but should rest frequently and avoid sustained activity - educate pt’s about fluctuating nature of weakness and exercise induced fatiguability |
|
|
How does a TBI occur?
|
• Acceleration
• Deceleration • Rotational forces • Causes: • compression • strain • shearing • displacement of brain tissue |

