![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
108 Cards in this Set
- Front
- Back
|
What is the prototypical psychotic illness?
|
Schizophrenia
|
|
|
Do all patients with Schizophrenia have the same symptoms?
|
No, there are several related symptom clusters
|
|
|
How important is Schizophrenia to public health / health-care expenses?
|
~2.5% of total healthcare expenses in US
|
|
|
How prevalent is Schizophrenia? Males vs Females?
|
Lifetime prevalence: 0.6-1.9%
~ 1% worldwide Lifetime prevalence in men and women equal, but average age of onset is lower in men |
|
|
What is the peak age of onset of schizophrenia in males vs females?
|
- Males: 15-25 years
- Females: 15-35 years |
|
|
Who is the "father of modern psychiatry"?
|
Emil Kraepelin
- Munich-based professor - Clearly differentiated manic-depressive illness from progressive illness he called "dementia praecox" - a premature deteriorating disorder |
|
|
Who named schizophrenia?
|
Eugen Bleuler
- Zürich-based professor - Characterized "the group of schizophrenias" as having in common a split among affect, thought, emotion, and behavior |
|
|
What are the "four A's" that Bleuler coined?
|
4 A’s were presumed to lie at the core of schizophrenia and fundamental aspects of the disorder:
- Affect: inappropriate or flattened affect-emotions incongruent to circumstances/situation - Autism: social withdrawal- preferring to live in a fantasy world rather than interact with social world appropriately - Ambivalence: holding of conflicting attitudes and emotions towards others and self; lack of motivation and depersonalization - Associations: loosening of thought associations leading to word salad / flight of ideas / thought disorder |
|
|
What is the term for inappropriate or flattened affect / emotions, which may be incongruent to the circumstances / situation, in schizophrenia?
|
Affect
|
|
|
What is the term for social withdrawal, preferring to live in a fantasy world rather than interact with social world appropriately, in schizophrenia?
|
Autism
|
|
|
What is the term for the holding of conflicting attitudes and emotions towards others and self, lack of motivation and depersonalization, in schizophrenia?
|
Ambivalence
|
|
|
What is the term for the loosening of thought associations leading to word salad / flight of ideas / thought disorder, in schizophrenia?
|
Associations
|
|
|
Who characterized the "first rank symptoms" of schizophrenia?
|
Kurt Schneider:
- Münich based professor - Characterized thought broadcasting, thought withdrawal, voices arguing or commenting, and somatic passivity as first-rank, but non-specific symptoms |
|
|
What are the characteristics for diagnosis of schizophrenia in DSM-IV-TR?
|
2 (or more) of following, each present for a significant portion of time during 1-month period (or less if successfully treated):
(1) Delusions (2) Hallucinations (3) Disorganized speech (eg, frequent derailment or incoherence) (4) Grossly disorganized or catatonic behavior (5) Negative symptoms (ie, affective flattening, alogia, or avolition) Note: only one symptom is required if delusions are bizarre or hallucinations consist of voice keeping up a running commentary on person's behavior or thoughts, or 2 or more voices conversing with one another |
|
|
What are the social / occupational dysfunction for diagnosis of schizophrenia in DSM-IV-TR?
|
For a significant portion of the time since the onset of the disturbance, one or more major areas of functioning such as:
- Work - Interpersonal relations - Self-care Are markedly below the level achieved prior to the onset (or when the onset is in childhood or adolescence, failure to achieve expected level of interpersonal, academic, or occupational achievement). |
|
|
What is the duration for diagnosis of schizophrenia in DSM-IV-TR?
|
*Continuous signs of the disturbance persist for at least 6 months.
- This 6-month period must include at least 1 month of symptoms (or less if successfully treated) that meet Criterion A (i.e., active-phase symptoms) and may include periods of prodromal or residual symptoms. - During these prodromal or residual periods, the signs of the disturbance may be manifested by only negative symptoms or two or more symptoms listed in Criterion A present in an attenuated form (e.g., odd beliefs, unusual perceptual experiences). |
|
|
What disorders must be excluded to make a diagnosis of schizophrenia in DSM-IV-TR?
|
Schizoaffective and Mood Disorder exclusion:
These disorders with psychotic features have been ruled out because either (1) no major depressive, manic, or mixed episodes have occurred concurrently with active-phase symptoms, or (2) if mood episodes have occurred during active phase symptoms, their total duration has been brief relative to duration of active and residual periods |
|
|
Besides psychological disorders, what else must be excluded to make a diagnosis of schizophrenia in DSM-IV-TR?
|
Substance / general medical condition exclusion:
- Disturbance is not d/t direct physiological effects of a substance (eg, drug of abuse or medication) or a general medical condition |
|
|
If a patient has a pervasive developmental disorder, how do you make a diagnosis of schizophrenia in DSM-IV-TR?
|
If there is a history of Autistic Disorder or another Pervasive Developmental Disorder:
- The additional diagnosis of Schizophrenia is made only if prominent delusions or hallucinations are also present - Present for at least a month (or less if successfully treated) |
|
|
How does the symptomology / characteristics of diagnosing schizophrenia differ in DSM-5:
2 (or more) of following, each present for a significant portion of time during 1-month period (or less if successfully treated): (1) Delusions (2) Hallucinations (3) Disorganized speech (eg, frequent derailment or incoherence) (4) Grossly disorganized or catatonic behavior (5) Negative symptoms (ie, affective flattening, alogia, or avolition) Note: only one symptom is required if delusions are bizarre or hallucinations consist of voice keeping up a running commentary on person's behavior or thoughts, or 2 or more voices conversing with one another |
* You need at least one of the two (or more) symptoms to be (1) delusions, (2) hallucinations, or (3) disorganized speech (eg, frequent derailment or incoherence)
|
|
|
How does the symptomology / characteristics of diagnosing schizophrenia differ in DSM-5, for which disorders must be excluded to make a diagnosis of schizophrenia in DSM-IV-TR?
|
Must rule out:
DSM-IV-TR: - Schizoaffective and Mood Disorder exclusion DSM-5: - Schizoaffective disorder and depressive or bipolar disorder with psychotic features |
|
|
What are the positive symptoms of schizophrenia?
|
Symptoms in ADDITION to expected behavior:
- Delusions - Hallucinations - Behavioral disturbances: agitation or talkativeness |
|
|
What are the negative symptoms of schizophrenia?
|
Symptoms that are MISSING from expected behavior:
- Social isolation - Withdrawal - Poor grooming - Anergy - Loss of interest - Blunted affect |
|
|
What are the cognitive symptoms of schizophrenia?
|
- Impaired abstract thinking
- Impaired problem-solving - Disturbed memory |
|
|
How was schizophrenia historically classified?
|
DSM-5 eliminates these classifications:
- Catatonic - Disorganized - Paranoid - Residual - Undifferentiated |
|
|
What are the theories of etiology for Schizophrenia?
|
- Genetic predisposition is important (shown in twin studies)
- Anatomic changes present - Physiologic changes present - Biochemical factors involved |
|
|
What are the anatomic changes present in schizophrenia?
|
- Enlarged lateral ventricles
- Increased width of third ventricle - Sulcal enlargement |
|
|
What are the physiologic changes present in schizophrenia?
|
- Dorsolateral prefrontal cortex poorly activated
- Thalamus and cerebellum possibly involved |
|
|
What are the biochemical factors present in schizophrenia?
|
Dopamine D2 receptors are blocked by all antipsychotics
|
|
|
How are all anti-psychotics similar in mechanism?
|
Block Dopamine D2 receptors (they may have other effects too)
|
|
|
What are the signs of schizophrenia on a PET scan?
|
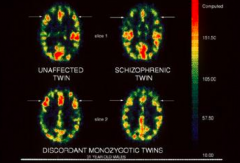
Reduced brain activity in the frontal lobes
|
|
|
How do you treat Schizophrenia?
|
Primary treatment: medications
- Atypical antipsychotics (dopamine-serotonin antagonists, eg, olanzapine, risperidone, quetiapine) - Generally used in preference to old-style neuroleptic (dopamine antagonists, eg, haloperidol, chlorpromazine, fluphenazine) Psychosocial interventions: - Housing, case management w/ emphasis on medication compliance and community involvement, supportive psychotherapy, vocational training |
|
|
What are the side effects of anti-psychotics for Schizophrenia?
|
- Acute dystonia
- Akathisia - Tardive dyskinesia (though less so w/ atypical antipsychotics) |
|
|
What is the prognosis for Schizophrenia?
|
- Exacerbations and remissions common
- Residual impairment is the rule - Positive sx less severe over time - Negative sx more severe over time |
|
|
What happens to the symptoms with time in schizophrenia?
|
- Positive sx less severe over time
- Negative sx more severe over time |
|
|
What is the effect of Schizophrenia on families?
|
High expressed emotion (EE)
- Criticism - Hostility - Over involvement - Tendency to do more poorly over time than others |
|
|
What is the long-term prognosis of Schizophrenia?
|
- 20-30% lead somewhat normal lives
- 20-30% experience moderate symptoms - 40-60% significantly impaired |
|
|
What are the other schizophrenia spectrum and psychotic disorders?
|
• Schizotypal (personality) disorder: Oddness
• Schizophreniform disorder: 1-6 months • Schizoaffective disorder: Mood symptoms • Brief psychotic disorder: 1 day-1 month • Delusional disorder: Functioning not markedly impaired except by delusions • Psychotic disorder due to another medical condition • Substance/medication-induced psychotic disorder • Catatonia specifier—various types • Other and unspecified schizophrenia spectrum and other psychotic disorders |
|
|
Which of the following is a historical name for schizophrenia?
a) Melancholia b) Dementia praecox c) Mania d) Kanner’s autism |
Dementia Praecox
|
|
|
Which of the following is eliminated from DSM-5’s criteria for schizophrenia?
a) Delusions b) Hallucinations c) Subtypes d) Disorganized speech |
Subtypes
|
|
|
Which of the following is a positive symptom of schizophrenia?
a) Delusions b) Loss of interest c) Blunted affect d) Impaired abstract thinking |
Delusions
|
|
|
What is psychosis?
|
- Derangement of personality
- Loss of contact w/ reality - Delusions - Hallucinations |
|
|
What is the prototypical psychosis?
|
Schizophrenia
|
|
|
How common is Schizophrenia?
|
- 12-month prevalence: 1.1% of US adult population
- Severe: not reported |
|
|
What are the positive symptoms of Schizophrenia?
|
- Hallucinations
- Suspiciousness - Grandiosity - Hostility - Excitement - Disorganized speech and behavior |
|
|
What are the negative symptoms of Schizophrenia?
|
- Blunted affect
- Emotional withdrawal - Inappropriate affect - Lack of spontaneity - Poor abstract thinking - Poverty of thought - Social withdrawal |
|
|
What is the NT hypothesis for Schizophrenia?
|
Dopamine Hypothesis:
- Schizophrenia results from hyperactivity of dopaminergic neurons or their receptors - Particularly those with terminals in limbic areas of brain - Mechanism of action of all effective antipsychotics: interact w/ dopamine systems |
|
|
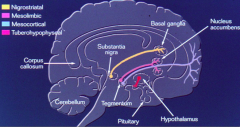
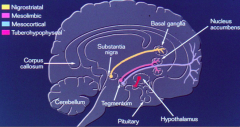
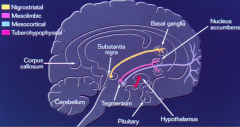
What are the dopaminergic pathways in brain?
|
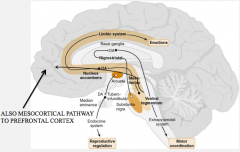
Use DA as pathway, and involved in therapeutic action of anti-psychotic drugs or side effects
- Mesolimbic pathway - Mesocortical pathway - Nigrostriatal pathway - Tuberoinfundibular pathway |
|
|
Where does Mesolimbic Pathway originate? Involved in?
|
- Originates in A10
Involved in: - Arousal - Memory - Stimulus processing - Locomotor activity - Motivational behavior |
|
|
Which pathway is responsible for positive symptoms of schizophrenia?
|
Dopamine hyperactivity in Mesolimbic Tract
|
|
|
Where does Mesocortical Pathway originate? Involved in?
|
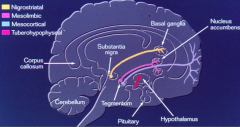
- Originates in A10
Involved in: - Cognition - Communication - Social activity |
|
|
Which pathway is responsible for negative symptoms of schizophrenia?
|
Diminished dopaminergic activity in the Mesocortical tract
|
|
|
Where does Nigrostriatal Pathway originate? Involved in?
|
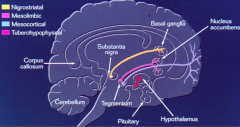
- Originates in A9
Dopamine blockade → ↑ EPS Blockade of 5-HT2a → ↓ EPS, parkinsonism |
|
|
Which pathway is responsible for Extrapyramidal symptoms of anti-psychotic drugs?
|
Nigrostriatal pathway:
- Dopamine blockade → ↑ EPS - Blockade of 5-HT2a → ↓ EPS, parkinsonism |
|
|
What is the Tuberoinfundibular Pathway involved in?
|
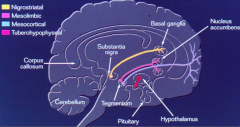
Dopamine blockade → ↑ Prolactin release
|
|
|
What do the anti-psychotic drugs act on?
|

Inhibits:
- Dopamine (D2/D3) receptors on presynaptic neuron - Dopamine (D2) receptor on postsynaptic neuron - Some act on D1 receptor on postsynaptic neuron (less common) |
|
|
What does lithium act on?
|

Inhibits:
- DA release from presynaptic neuron - IP → I conversion in postsynaptic neuron |
|
|
How do stimulants act?
|

Inhibits:
- Reuptake of DA into Presynaptic neuron |
|
|
Atypical antipsychotics act on what receptors?
|
- Block DA receptors (mostly DA2)
- Block 5-HT2 receptors in forebrain (often with greater potency than for DA receptors) |
|
|
What are the types of Dopamine receptors? Mechanism?
|

- D1 type (D1 and D5) --> activates AC (Gs)
- D2 type (D2, D3, D4) --> inhibits AC (Gi) - Autoreceptors |
|
|
What neurochemical effect confers upon some antipsychotic drugs decreased extrapyramidal symptoms and the ability to decrease the negative symptoms of schizophrenia?
a) Blockade of 5-HT2 receptors b) Blockade GABA receptors c) Stimulation of 5-HT2 receptors d) Blockade of NMDA receptors e) Stimulation of D1 receptors |
Blockade of 5-HT2 receptors
|
|
|
What are the typical antipsychotics?
|
- Chlorpromazine
- Fluphenazine - Thioridazine - Thiothixene - Haloperidol - Pimozide |
|
|
What are the atypical antipsychotics?
|
- Clozapine
- Olanzapine - Risperidone - Quetiapine - Aripiprazole - Ziprasidone |
|
|
What are the pharmacokinetic properties of antipsychotic drugs?
|
- Oral absorption: variable
- Lipid soluble - Protein binding - Large volumes of distribution - Complex metabolism |
|
|
Which of the following drugs is most likely to produce Parkinson-like side effects?
a) Buspirone b) Chlorpromazine c) Haloperidol d) Olanzapine e) Sertraline Which other ones would also produce some Parkinson-like side effects? |
Most likely: Haloperidol
2nd: Chlorpromazine 3rd: Olanzapine Not seen in: Buspirone, Sertraline |
|
|
What is the best way to treat Schizophrenia?
|
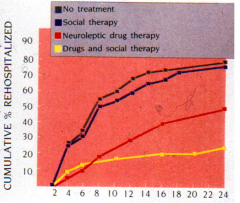
Antipsychotic drugs and social therapy (not curative though)
|
|
|
What are the useful actions of antipsychotic drugs?
|
- Decrease in psychotic behavior (typical drugs differ only in potency)
- Negative symptoms are not well treated by older typical agents - Atypical drugs effectively treat positive and negative symptoms |
|
|
What are some side effects of antipsychotic drugs?
|
*Sedation
*Extrapyramidal effects - Early reactions: dystonias, Parkinsonism, and akathisia (these reactions more with typicals) - Late reactions: tardive dyskinesia (less frequent with atypicals) * Neuroleptic malignant syndrome * Anti-cholinergic: dry mouth, blurred vision, urinary retention * Neuroendocrine effects: result of dopamine receptor blockade * Orthostatic hypotension * Weight gain: diabetes related events more common w/ atypicals * Allergic and idiosyncratic effects: liver, blood, and cutaneous - Cardiac effects (thioridazine) |
|
|
What are the features and onset of acute dystonia due to anti-psychotic drugs?
|
- Spasm of muscles of tongue, face, neck, and back
- Opisthotonus (spasm of the muscles causing backward arching of the head, neck, and spine) - Onset: 1-5 days (early reaction) |
|
|
What are the features and onset of parkinsonism due to anti-psychotic drugs?
|
- Bradykinesia
- Mask-like facies - Tremor - Rigidity - Shuffling gait - Drooling - Cogwheeling - Stooped posture - Onset: 5-30 days (early reaction) |
|
|
What are the features and onset of akathisia due to anti-psychotic drugs?
|
- Compulsive, restless movement
- Symptoms of anxiety and agitation - Onset: 5-60 days (early reaction) |
|
|
What are the features and onset of tardive dyskinesia due to anti-psychotic drugs?
|
- Oral-facial dyskinesias
- Choreoathetoid movements - Onset: months to years (late reaction) |
|
|
Which antipsychotic drug can cause cardiac effects?
|
Thioridazine
|
|
|
Which antipsychotic drug can cause weight gain? Implications
|
More common with atypicals:
- Olanzapine - Risperidone - Clozapine - Quetiapine Leads to more diabetes related events |
|
|
What are the anti-cholinergic side effects of antipsychotic drugs?
|
- Dry mouth
- Blurred vision - Urinary retention |
|
|
What causes the neuroendocrine side effects with antipsychotic drugs?
|
Result of dopamine receptor blockade
|
|
|
What causes Neuroleptic Malignant Syndrome? Symptoms? Treatment?
|
Cause: hypodopaminergic side effect of anti-psychotic drugs
Symptoms: Parkinson-like sx (muscular rigidity and tremor), mutism, and possible death Treatment: cooling and hydration, bromocriptine, and dantrolene |
|
|
What are the typical phenothiazine antipsychotic drugs? Structural differences?
|
- Chlorpromazine: aliphatic side chain
- Thioridazine: piperidine side chain - Fluphenazine: piperazine side chain |
|
|
What are the characteristics of Chlorpromazine?
|
Phenothiazine (typical) w/ aliphatic side chain
- Low to medium potency - Sedative - Pronounced anticholinergic actions |
|
|
What are the characteristics of Thioridiazine?
|
Phenothiazine (typical) w/ piperidine side chain
- Low potency - Sedative - Less extrapyramidal actions, anticholinergic |
|
|
What are the characteristics of Fluphenazine?
|
Phenothiazine (typical) w/ piperazine side chain
- High potency - Less sedative - More extrapyramidal reactions, less anticholinergic actions |
|
|
What are the typical thioxanthine antipsychotic drugs? Characteristics?
|
Thiothixene
- Non-nitrogen containing analog of phenothiazines - Pharmacology is similar to their equivalent phenothiazines |
|
|
What are the typical Butyrophenone antipsychotic drugs? Characteristics?
|
Haloperidol
- Not chemically related to phenothiazines - Pharmacologically similar to high-potency piperazine derivatives |
|
|
What are the characteristics of the other typical antipsychotic drug?
|
Pimozide
- Potent neuroleptic - Many side effects - Approved for treatment of Tourette's - Commonly used when Haloperidol does not work |
|
|
What is the relationship between sedating / CV signs and Parkinsonian signs for antipsychotic drugs?
|
Inverse relationship:
- The more sedating and CV signs, the fewer Parkinsonian signs - Vice versa |
|
|
Why were atypical antipsychotic drugs developed?
|
- Need for better antipsychotic drugs
- Desired more acceptable side-effect profile - Desired more efficacious treatment of negative symptoms in schizophrenia |
|
|
What are the atypcial antipsychotics?
|
- Clozapine
- Olanzapine - Risperidone - Quetiapine - Aripiprazole - Ziprasidone |
|
|
What are the advantages of atypcial antipsychotics over typicals?
|
In general:
- ↓ incidence of extrapyramidal sx (better compliance) - Possibly ↓ incidence of tardive dyskinesia (TD) - Improves positive symptoms in many antipsychotic resistant or refractory patients - Improves negative symptoms (?) - Less impact on cognitive functioning (?) - More cost effective (???) |
|
|
Which drug is most likely to cause agranulocytosis?
a) Aripiprazole b) Clozapine c) Haloperidol d) Olanzapine e) Risperidone |
Clozapine
|
|
|
What is the mechanism of Clozapine?
|
- Blocks D4 receptors
- Blocks 5-HT2 receptors - Muscarinic antagonist |
|
|
What are the positive and negative effects of Clozapine?
|
Positive:
- Best efficacy - Improves + sx (even in patients not helped by others) - Improves - sx Negative: - Lowers seizure threshold (5-10% incidence of enhanced seizures) - Can cause fatal agranulocytosis (requires monitoring) * Last resort drug now |
|
|
What is the mechanism of Olanzapine?
|
- Potent 5-HT2 antagonist
- D1 and D2 antagonist (some D4 |
|
|
What are the positive and negative effects of Olanzapine?
|
Positive:
- Helps with + and - symptoms of schizophrenia - Few extra-pyramidal symptoms (5-HT>D) - Less seizure incidence (than Clozapine) - No agranulocytosis Negative: * Weight gain and diabetes - Reports of abuse |
|
|
What is the mechanism of Risperidone?
|
- D2 antagonist
- 5-HT2 antagonist - Active metabolite: Paliperidone |
|
|
What are the positive and negative effects of Risperidone?
|
Positive:
- Greater reduction in negative symptoms - Less extrapyramidal symptoms - Less seizure activity (than clozapine) - Less antimuscarinic (than clozapine) - Don't have to take daily (intramuscular depot prep available) |
|
|
What is the mechanism of Quetiapine?
|
- D2 antagonist
- 5-HT2 antagonist |
|
|
What are the positive and negative effects of Quetiapine?
|
Positive:
- Treats + and - symptoms of schizophrenia - Few extrapyramidal symptoms - No agranulocytosis - Augmentation of depression Negative: - Some reports of abuse - Shorter t1/2 (may be benefit in elderly) |
|
|
What is the mechanism of Ziprasidone?
|
- 5-HT2 antagonist
- D2 antagonist - May have 5-HT1a agonist (anxiolytic action?) |
|
|
What are the positive and negative effects of Ziprasidone?
|
Positive:
- No weight gain - Possible anxiolytic activity |
|
|
What is the mechanism of Aripiprazole?
|
- Partial D2 agonist
- 5-HT2 antagonist |
|
|
What are the positive and negative effects of Aripiprazole?
|
Positive:
- Also approved as an adjunct in depression (augmentation) |
|
|
What are the uses of antipsychotic drugs?
|
- Acute psychotic episodes
- Chronic schizophrenia - Manic episodes, bipolar disorder - Schizoaffective disorder - Augmentation of depression - Tourette's syndrome - Anti-emesis |
|
|
Which antipsychotic drugs can be used for manic episodes in bipolar disorder?
|
- Aripiprazole
- Olanzapine - Quetiapine - Ziprasidone - Risperidone |
|
|
Which antipsychotic drugs can be used for augmentation of depression?
|
- Aripiprazole
- Olanzapine - Quetiapine |
|
|
Which antipsychotic drugs can be used for Tourette's syndrome?
|
- Haloperidol
- Pimozide |
|
|
A 28 y/o patient with known schizophrenia presents with mutism and extreme psychomotor slowing. On physical examination this patient holds uncomfortable body positions for long periods of time. What is exhibited?
a) Catatonia b) Delusions c) Disorganization d) Paranoia |
Catatonia
|
|
|
A 35y/o patient with known schizophrenia tells her psychiatrist that she cannot listen to a news broadcast on the television or radio without worrying that the news story is referring to her. What symptom is this patient experiencing?
a) Hallucination b) Idea of reference c) Illusion d) Neologism |
Idea of Reference
|
|
|
Which of the following medications is most suitable for the treatment of schizophrenia?
a) Fluoxetine b) Haloperidol c) Imipramine d) Lithium e) Lorazepam |
Haloperidol
|

