![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
10 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
What are the factor considered to operate a child? |
Body build: 1. Infant has wide abdomen, board costal margin, narrow pelvis.- so transvers incision is better for visualise abdomen better. 2. The edge of the liver is below the costal margin and bladder is intraabdominal which is common site for traumatic injury. 3. Ribs are horizontally placed and more flexible. So ventilation requires more diaphragmatic movement and ribs fracture are rare, if not abused. 4. The umbilicus is low lying in position- so a stoma in a infant should be cautiously done thus not interfare with umbilicus. 5. Mainatance of temparature : A) Infant has a less subcutaneous fat than older chield, immature vasomotor activity, more heat evaporation through pulmonary ventilation. There skin surface area is greater than their weight. B) head is 18% in proportion to body than adult 9%. Head should be insulated. C) in OT, environment should be warm D) infusion should be warm and inspired air should be insulated and humidify. E) core temparature sho7ld be monitorand maintain 3) Airway: A) head is large and neck is short, so flexon tendency occur in infant B) epiglottis lies posteriorly and larynsx is high up, so straight blade laryngoscope is necessary. C) in a unconscious infant large toungue trend to obstruct the airway. D) uncuffed airway tube is preferred as cricoid cartilage is the narrowest area. |
|
|
|
How will you prepare a 3 year old child for laparotomy |
1. A complete history is taken. 2. Complete physical examination is done 3. Investigation : A) investigation for dx B) investigation for anaesthetic checkup: 1. Cbc, blood Group and rh typing Urine rme, s.creatinine, chest xray, coagulation profile. Liver function test: if jaundice is present. 4. Focus should turn to specific comorbidity. A) optimization of co morbidity. B) refer to specific specialist for mx of comorbidity. 5. Arreange for blood if needed. 6. Bowel preparation for laparotomy. 7. Finally, list the operation, and monitor the patient post operative ly. |
|
|
|
What are the factor that u considered to prescribing fluids in paediatric age group? |
1. Before prescribing fluid to a child, weight, vital sign, fluid and electrolyte requirement should be known. 2. Should know the four reasons thats why fluid should be given. 3. Should know how to calculate the fluids 4. Should be care full about the harmful effect of low sodium fluid in child. 5. Know how to recognise and manage hyponatremia <135 mmol in children 6. Understand how bodys response to trauma and stress affect fluid balance. Fluid management for 4 reasons: 1) circulating collapse and ressusitation: 0.9%nacl or blood or 4.5%albumin 2) fluid for previous fluid loss: 0.9% nacl + 0.15% kcl or hartmann 3) fluid for on going fluid loss: 0.9% nacl + 0.15% of kcl or hartmann 4. Maintainace fliud: A) outside infant age: plasmalyte 148 or hartmann +- glucose or 0.9% nacl+ 0.15%kcl+- glucose. B) maintance inside infant age: 1) for first 48 hours fluid should be given 10% glucose at 60 ml/ kg/ day. 2) in day 2 sodium 0.18% + 0.15% kcl 3) from day 3- 4-5 ml/kg/hour or 100-120 ml/kg/day should be given. 4. In preterm baby or those <2 years should give 180 ml/ kg/day. |
|
|
|
How will you evaluate 3 minth old child with profund vomitting? |
Before evaluating the vomiting, cause should be identified: 1. Bilious vomiting: older child Intussusseption Intestinal malrotation with volvulus. Incernated hernia. In infant: Duodenal / jejunal/ ileal atresia Hurshpung disease. Anorectal malformation Necrotising enterocolitis. 2. Non bilious vomiting: Infantile hypertrophic pyloric stenosis. Gastroesophageal reflux. Feeding difficulty Non specific cause: infection, raised icp, metabolic disorder. Evaluation: 1. History taking about vimitous: color, nature, onset, duration, projectile or not, natal history: preterm/ term / maternal polyhydraamnios Abdominal : pain, constipation, cough, sore thoart 2. Clinical examination: State of dehydration, mental state. Look sign of raused icp Abdominal examination including DRE. 3. investigation : Imaging: xray abdomen, usg of the abdomen, blood for routine test Urine rme, cs |
|
|
|
What is acute scrotum? How can you evaluate a 5 years old child with acute rt scrotal pain for 10 hours? |

Another pic |

|
|
|
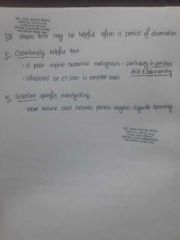
How will you evaluate a child having rt lower abdominal pain for 36 hours? |

|
|
|
|
Sergical techniques in children? |
1. Gentle handing. 2. Avaoid tension 3. Minimise contamination and tissue necrosis 4. Abdominal incision can be closed by absorbable suture 5. Bowel anastomosis can be done by interrupted or continueous single layer extramucosal suture. 6. Skin closure can be done by absorbable subcuticular suture. |
|
|
|
What are the pattern of pediatric trauma? Mx of trauma |
1. Lap belt: small intestine or lumber spine. 2. Bicycle handle: pancrease, bowel, mesentery, liver. 3. Straddle: urethra, pelvis 4. Run over : severe crush injury of chest and abdomen. Mx Use atls protocol to manage the child but remember some difference. 1. Avoid overextension of the neck which can obstruct airway of a child. 2. Use a broselow tape if weight can not measure. 3. Blood pressure is often normal until >25% of circulatory volumn is lost. 4. Cardiorespiratory arrest due to hypoxia, not to vascular cause. 5. Non operative management for isolated liver or splenic injury can be manage by non operative treatment. 6. Cervical spine injury is often absent in a radiograph. 7. Lung contusion can be present with out present of rib fracture. 8. Pattern skin bruising often suggest a underlying organ injury. 9. In astable child, abdominal injuries are best assess by the CT scan. |
|
|
|
Name some common pediatric surgical condition? |
Inguinoscrotal: Inguinal hernia Hydrocele Undescended testis Acute scrotum: Torsion Epididymorchitis Penis: Hypospedius Phimosis Paraphymosis Box infection Midline hernia Ihps Intussusseption |
|
|
|
Evaluation of acute abdominal pain in children over 3 years of age? |

Another |
|

