![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
159 Cards in this Set
- Front
- Back
|
what responds to an increased level of hydrogen ions in the blood and spinal fluid to increase rate and depth of respiration?
|
Chemoreceptors in the medullar oblongata and the carotid body.
Excess levels signal respiratory center in the medulla oblongata. |
|
|
What is happening during systole and diastole and what makes the S1, S2, S3, S4 heart sounds?
|
Systole: ventricles contract and eject blood
Diastole: ventricles are filling S1: mitral and tricuspid closure S2: aortic and pulmonic closure (both S3&S4 occur during diastole as the ventricles fill) S3: (possible) ventricle filling in diastole S4: (possible) atrial contraction |
|
|
How do you figure out cardiac output and what does this mean?
|
Stroke volume (amount of blood ejected in one minute) multiplied by heart rate. This is the measure of the heart's ability to adapt to demands.
|
|
|
Briefly define systolic, diastolic, and pulse pressure
|
Systolic: force of blood against artery wall when the ventricles contract.
Diastolic: force against wall when heart is filling or relaxed. Pulse Pressure: difference between systolic and diastolic pressures. |
|
|
what are the three tissues that make up the breast?
|
1. glandular (mammary)
2. fibrous (connective) 3. adipose (fat) |
|
|
how many lobes are in each breast that ducts extend from to the lactiferous sinus'?
|
15-20
|
|
|
What is the purpose of Montgomery glands on the areola?
|
lubrication
|
|
|
What is the Tail of Spence in the breast?
|
glandular tissue that extends up to the axilla
|
|
|
What is Cooper's Ligament in the breast?
|
supports breast, runs vertically and attaches in the deep layer of subcutaneous tissue to the dermis.
|
|
|
What are the lymph nodes associated with the breast?
|
1. axillary nodes
2. internal mammary nodes (along sternum) 3. supraclavicular |
|
|
What is the earliest sign of puberty? (explain what age, length, and what it signifies)
|
Thelarche:
-ages 8-14 (but mammary ridge is present at 5-6weeks gestation) -4 years to complete -earliest sign of hypothalamus-pituitary-ovarian axis -estrogen has the greatest influence on breast growth at this time |
|
|
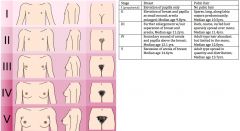
Describe the stages of Tanner Staging
|
|
|
|
Which organ produces antibodies, prothrombin, fibrinogen, other coagulation factors, and most plasma proteins?
|
The liver
|
|
|
List the functions of the anterior vs the posterior pituitary
|
AnterIor: prolactin, growth hormone, thyroid stimulating hormone, ACTH, melanocyte stimulating hormone, follicle stimulating hormone, and luteinizing hormone.
Posterior: stores and releases hormones produced by the hypothalamus (antidiuretic hormone (ADH, vasopressin) and oxytocin) |
|
|
List the stages of infection in order
|
1. Colonization
2. Invasion 3. Multiplication 3. Spread |
|
|
List the different types of infectious organisms
|
1.Virus
2.Chlamydiae, Rickettsiae, Mycoplasma, and Ureaplasma (similar to bacteria in reproduction and susceptability, but not in structure and metabolic capabilities) 3. Bacteria, spirochetes, mycobacteria 4. Fungi (including yeast) 5. Protozoa (single cell, trichomoniasis) 6. Helminths (parasitic worms) 7. Ectoparasites (arthropods; lice, tics, bed bugs, mites, fleas) |
|
|
Explain the difference between autosomal dominance and autosomal recessive traits and the risk associated with the offspring of the two parents
|
-Autosomal Dominance: only one copy of the gene (heterozygous) is needed for expression of the trait (so offspring may inherit from one parent, 50% chance) (Ex:Marfan Syndrome)
Autosomal Recessive: both genes must be the same (homozygous) for trait to be expressed. If only one parent has the gene the child is a carrier, if both parents have the gene the offspring have a 25% chance of expressing the trait. (Ex:Galactosemia) |
|
|
What are X linked diseases? And are most dominant or recessive?
|
-Most are recessive.
-Gene is not expressed in mother b/c she has another X gene for balance, but it acts as a dominant gene in the male offspring who inherits it and the trait is expressed (example: color blindness). -The mother is only affected if she has an X linked dominant (rare) or two copies of the x linked recessive. |
|
|
Sons of heterozygous women w/ an x-linked recessive gene have what chance of being affected?
|
50%
|
|
|
List the four factors that influence infection.
|
1. Mechanism of action
2. Infectivity: ability to invade and reproduce 3. Pathogenicity: ability to produce disease 4. Virulence: potency of a pathogen, i.e., number of organisms needed to produce disease. |
|
|
Describe the adaptation of the maternal immune system in pregnancy.
|
Adaptation promotes tolerance of products of conception. Includes delays in some immune reactions and increased susceptibility to some infectious organisms e.g., gram negative organisms and fungi. Transfer of immunoglobulins in the third trimester = mother more susceptible to colonization w/ organisms such as streptococci and staphylococci.
|
|
|
What is the leading, and then second leading cause of death in the U.S?
|
1. Heart Disease
2. Cancer Lung cancer has overtaken as leading cause of cancer DEATH in women. Colorectal cancer is the third leading cause of cancer DEATH in women. (breast cancer more common, but lung cancer = >deaths) |
|
|
Define dysplasia and what it means in terms of it becoming cancer.
|
Disordered growth of cells, w/loss of uniformity of cell size and orientation. Usually preceded carcinoma (precancerous) but dysplasia does not necessarily progress to cancer.
|
|
|
Define carcinoma in situ
|
dysplastic cells are marked and occupy the entire epithelial thickness, but do not invade the basement membrane.
|
|
|
In general, what age group is most vulnerable to cancers?
|
55-74
|
|
|
What is the leading cause of preventable mental retardation in the U.S.?
|
Fetal alcohol syndrome
|
|
|
What is the general guidelines on eating fish concerning mercury exposure?
|
Dont eat: king mackerel, shark, sword fish, tilefish
Yes (12oz/week):shrimp, canned light tuna, salmon, pollock, catfish, lobster, crab. Women of childbearing age, pregnancy, and nursing, and young children advised these guidelines. |
|
|
What BMI defines obesity, and extremem obesity?
|
obesity: at or >30
extreme obesity: at or >40 |
|
|
In regards to body circumference, what waist measurements signify high risk in men and women?
|
Waist >40 in men
Waist >35 in women |
|
|
What is the main problem with vitamin and herbal therapies according to the ACNM and what guidelines do they suggest when discussing them w/ pts?
|
-Problem: herbal remedies are not standardized
-Guidelines: routinely inquire about consumption/use. Herbal medicines are made from plant, parts of a plant, or combinations of plants. Acknowledge lack of standardization and variability in herb content. |
|
|
Define GTPAL according to the ACNM book
|
G= number of pregnancies
T= term deliveries > or = 37wks P=preterm deliveries (20-36wks) A=spontaneous or induced abortion <20wks L=number of living children *multiple gestation does not increase parity, it is evident in the number of living children. Outcomes w/ dates should be noted by the MW |
|
|
What kind of sound auscultated while examining the heart always suggests pathology?
|
S4 (atrial gallop) is Ten-es-SEE and always means pathology
|
|
|
What kind of an arrhythmia can be a normal finding in a young reproductive age woman? What should you do to assess it?
|
Sinus arrythmia
Have her hold her breath and see if it resolves. |
|
|
What are the auscultatory areas of the heart?
|
1.Aoritc valve area: 2nd R ICS, R sternal border
2. Pulmonic valve area: 2nd L ICS, L sternal border 3. Second pulmonic valve area: 3rd L ICS, L sternal border 4. Tricuspid area: 4th L ICS, lower L sternal border 5. Mitral (apical) area: apex of the heart in 5th ICS, midclavicular line |
|
|
What are the different grades of heart murmurs?
|
I. barely audible in a quiet room
II. quiet but clearly audible III. moderately loud IV. very loud, thrill easily palpated VI. very loud, audible w/ stethoscope not in contact w/ chest, thrill palpable and visible. |
|
|
What are the normal breath sounds heard when auscultating the lungs?
|
1. vesicular: heard over the periphery of the lung field (low pitch)
2. bronchial: are normally heard over the trachea and larynx (medium pitch) 3. bronchovesivular: 1st ICS both sides of sternum, between scapula and over the lung apices (high pitched) Bronchovesicular sounds can be heard all over in thin people and young children, otherwise abnormal in peripheral lung fields. |
|
|
What are the four adventitious lung sounds that can be heard, and which one can clear w/ coughing?
|
crackles, wheezes, ronchi, and pleural friction rub.
Ronchi MAY clear w/ coughing |
|
|
What are the 9 Fs of abdominal distention?
|
Fate
Fluid (ascites) Feces Fetus Flatus Fibroid Full bladder False pregnancy Fatal tumor |
|
|
공연
|
a public performance―하다 perform
|
|
|
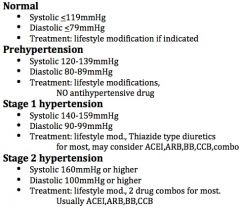
What are the classifications of blood pressure and basic treatments if indicated?
|
|
|
|
What is the most preventable cause of disease and death in the U.S.?
|
cigaretter smoking
|
|
|
Every pt who uses tobacco ______ be offered at least _______ _________.
|
should
brief treatment |
|
|
What are the effective pharmacotherapies for smoking cessation currently approved, and except in the presence of contraindications should be used?
|
1. FDA approved meds: bupropion SR, nicotine gum, inhaler, nasal spray, and patch.
2. Not FDA approved but may be used as second line tx: clonidine, and nortiptyline. 3. OTC nicotine patches are effective and should be encouraged. |
|
|
What drug is most frequently used by adolescents?
|
alcohol
|
|
|
What can longterm heavy drinking lead to?
|
heart disease
cancer alcohol related liver disease pancreatitis |
|
|
What constitutes binge drinking?
|
consuming 5 or more drinks on one occasion
|
|
|
What is recommended drinking limits for men and women?
|
2 drinks men
1 drink women per day |
|
|
What is the number one primary health care problem in the U.S.?
|
VIOLENCE AGAINST WOMEN
-experienced by 20-30% of all women at some time -7-20% of pregnant women are abused -most likely time for abuser to become homicidal is when the woman leaves -45-60% of children in the home of an abused mother/female are also abused |
|
|
What affects more women than HTN, GDM, or any other antepartum complication during pregnancy?
|
Violence in pregnancy
|
|
|
Even just moderate regular physical activity can help prevent what disease?
|
heart disease
diabetes colon cancer |
|
|
What are the basic exercise recommendations for preventing disease, maintaining weight, and loosing weight?
|
On MOST days of the week:
prevent disease: 30min maintain weight: 60min loose weight: 60-90min And do not exceed caloric requirements (umm... duh?:) |
|
|
You are a kick-ass Midwife and are going to SMOKE this exam: _____
|
YES!
You better believe it!!! :) :) :) |
|
|
What are the nutrition USDA Dietary Requirements for Americans (2005) in regards to:
fat, carbohydrates, sodium/potassium, folic acid? |
-Fat:20-35% of calories, should be polyunsaturated, monounsaturated.
-Carbohydrates: should be fiber rich, use added sugar rarely. -Sodium/Potassium: <2300mg sodium/day. -Folic Acid: 0.4mg/day. If hx of previous child w/neural tube defect, 4mg/day. |
|
|
What are the calcium requirements by age group?
|
-9-18yrs: 1,300mg/day
-19-50yrs: 1,000mg/day -51-older: 1,500mg/day -Postmenopausal ON estrogen: 1,000mg/day -Pregnant or Nursing: 1,200-1,500mg/day |
|
|
DSM IV criteria for major depression include ______ symptoms, present for a ______ period, and representing _______________. Either of the first ____ of DSM's criteria must be present.
|
a. 5 or more
b. 2 week c. a change from prior function d. 2 Criteria: 1. Depressed mood nearly every day for most of the say either by self-report or observation. 2. Diminished or absent pleasure in all or most activities, most of the day, most days. 3. Significant weight loss or gain, or decreased appetite every day. 4. Insomnia or hyper-insomnia 5. Psychomotor agitation/retardation 6. Fatigue or loss of energy 7. Feelings of worthlessness, or inappropriate or excessive guilt, possibly delusional. 8. Decreased ability to concentrate clearly, indecisiveness 9. Recurrent thoughts of death, suicidal ideation, suicidal plan or attempt. |
|
|
What is the frequency for Pap smears and STD testing according to the ACNM book?
|
2009 Version:
Pap Smear: -yearly beginning 3yr after sexual debut or at 21yrs. -ACOG says every 3yrs after 3 normals. -USPSTF recommends against routinely screening women older than 65yrs for cervical cancer if they have had adequate screening recently and were all normal (they are considered not high risk) Chlamydia/Gonorrhea/AIDS/Syphilis: chlamydia through age 25, then by risk |
|
|
What are the intervals for mammograms according to the American Cancer Society?
|
At or over age 40= yearly
Age 20-39 = clinical breast exam every 3 years |
|
|
What does the American Geriatric Society recommend for older women regarding mammograms?
|
Every year 65-75 y/o
Every 2-3 years >75 w/no risk factors |
|
|
What is the overall sensitivity of mammograms?
|
90-95% (5-10% false negative rate)
|
|
|
What can you tell a 40-49y/o pt that has had an abnormal mammogram reading who has no family history of breast cancer, or other risk factors?
|
95% of abnormal mammograms in women age 40-49 are false positives.
|
|
|
A premenopausal mammogram will miss_/_ of cancers?
___% of INVASIVE br ca is missed in women 40-49. |
1/3
25% |
|
|
What does ACOG recommend in regards to bone mineral density screening?
|
ACOG advises BMD testing for:
1. postmenopausal women who have sustained a fracture. 2. postmenopausal women <65y/o who have one or more risk facotrs: fracture as an adult, caucasian race, impaired eyesight despite adequate correction, hx or alcoholism. 3. Pre-or postmenopausal women w/ diseases/conditions w/ increased risk (endometriosis, hemophilia, lymphoma/leukemia, eating and nutritional disorders, rheumatoid arthritis, MS, tobacco, lithium, heparin) ***if no new risk factors, screening should not occur more than every 2 years. |
|
|
What is the 'gold standard' for bone density testing, and how are the results listed?
|
-dual-energy x-ray absorpiometry (DEXA)
-Gives T-scores: Normal: T-score above -1 Osteopenia: T-score between -1 and -2.5 Osteoporosis: T-score at or below -2.5 |
|
|
What is the frequency for colon-cancer screening?
|
-Fecal occult blood test annually >50y/o
-Sigmoidoscopy every 5 years after age 50 |
|
|
What is the frequency for a fasting lipid profile? And does it have to be fasting?
|
-Every 5 years beginning at age 20
- no (fasting or non-fasting) |
|
|
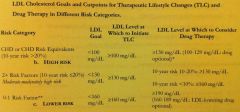
What are the LDL cholesterol primary targets of therapy?
|
<100 = optimal
100-129 = near optimal/above optimal 130-159 = borderline high 160-189 = high at or >190 = very high |
|
|
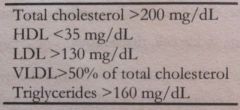
What are the low/desirable/high levels for HDL and total cholesterol?
|
|
|
|
What are the low/desirable/high levels for HDL and total cholesterol?
|
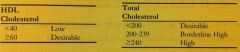
|
|
|
What are the LDL cholesterol goals and cut points for therapeutic lifestyle changes and drug therapy in different risk categories?
|
|
|
|
What diagnoses does CHD (coronary heart disease) encompass?
|
myocardial infarction, unstable angina, stable angina, coronary artery procedures like angioplasty or bypass surgery, or evidence of significant myocardial ischemia
|
|
|
According to the American Diabetic association, at what age and how often should a plasma glucose be drawn?
|
every 3 years after age 45
|
|
|
At what age, and how often should a TSH be drawn?
|
At age 45 every 2 years
At age 60 yearly for asymptomatic women *There are many conflicting reports, depends on who you are going by |
|
|
List assessments (lab tests) according to these age groups when a woman shows risk:
Ages 11-24, 25-64, 65-older |
Ages 11-24: Hbg, bactururia, STD, HIV, genetic counseling, TB skin test, fasting glucose
Ages 25-64 above plus: genetic testing/counsleing, TSH, colonoscopy, osteoporosis at and >60 Ages 65-older: Hgb, fasting glucose, STD, HIV, TB skin test, TSH, colonoscopy, osteoporosis |
|
|
If a woman is not on HRT, ERT, or OCs, _________ at or over ___ is diagnostic of menopause.
|
Follicle stimulating hormone
40mIU/mL |
|
|
Healthcare providers can and must assist in getting children vaccinated by telling parents about the _____________________ program, which provides funding for all recommended vaccines for eligible children.
|
Vaccines for Children Program
|
|
|
Who is the FluMist appropriate for? (influenza vaccine)
|
Healthy, non-pregnant persons aged 5-49 y/o w/out high-risk conditions who are not contacts of severely immunocompromised persons in special care units.
|
|
|
Who is the pneumococcal vaccination appropriate for?
|
Basically chronic disease dx, or immunocompromised, or one antimetabolites or has cochlear implants. This DOES NOT include asthma. Also Alaska Natives and some American Indians, residents of long term care facilities.
Revaccination is appropriate for some who are high risk and it has been 5 years since vaccination, and if >65 and were <65 at time of last vaccination. |
|
|
Who is the Hepatitis B vaccine appropriate for?
|
Basically if someone is at high risk for an STD including 2 or more partners in the past 6 months, occupational reasons including people who work with developmentally disabled persons, men who have sex w/ men, correctional facilities, if traveling to a country where Hep B is prevalent and will be there for more than 6 months.
|
|
|
Who is the MMR vaccine appropriate for?
|
-if born <1957 considered immune
-otherwise all should have at least one dose unles medically contraindicated -no MMR for HIV/AIDS people -2nd dose if exposed to measles, previously vaccinated w/killed virus or unknown type 1963-1967, students in postsecondary educational institutions, health care field, plan to travel internationally. -Do not give to persons allergic to eggs or neomycin -see other flash card for Rubella and pregnant women |
|
|
What are the special considerations regarding Rubella vaccine and pregnant women?
|
-unreliable/no hx of vaccination: give a dose unless currently pregnancy
-routinely determine immunity if of childbearing age and counsel on congenital rubella syndrome. Do not vaccinate women who are pregnant or plan of becoming pregnant w/in 4 WEEKS of vaccination. If a woman is not immune, she should receive the vaccination upon completion/termination of pregnancy before they leave the hospital. |
|
|
Who is the tetanus vaccine appropriate for?
|
-adult who hasn't had it before (primary series for adults is 3 doses, two 4 weeks apart and then the third 6-12 months later)
-booster if last dose was 10 or more years ago - |
|
|
Who is the Hepatitis A vaccination appropriate for?
|
clotting factor disorders, chronic liver disease, health care, men who have sex with men, traveling to a country where hep a is more common, because the pt wants to.
|
|
|
Who is the varicella vaccination appropriate for?
|
-all adults without evidence of immunity
-unless pt has history of varicella, or laboratory documented evidence |
|
|
Who is the meningococcal vaccination appropriate for?
|
asplenia, terminal ocmpliemnt component deficiences, first year college students living in a dorm, military, travel or live where more common. Revaccination at 5 years may be necessary.
|
|
|
Who is the HPV vaccination appropriate for? What strains does it cover?
|
-girls 9-26
-just FDA approved for boys -for strains 6,11,16,18 -also can be given to women who have not been infected by one or all of: 6,11,16,18 HPV |
|
|
What are the specific points to consider regarding vaccination of pregnant women?
|
-no live virus unless benefit of vaccine out-weighs risk of disease.
-only Adacel recommended for routine in pregnancy -hep B can be given for women who are high risk and test negative for hep B. -MMR: one month preior to prengnacy for immediately following delivery -Yellow fever and polio: only if traveling to where exposure risk is high -Varicella vaccine should be given to infant who's mother came down w/ varicella up to 5 days before or 2 days after delivery -CDC says varicella for all women after 1st trimester. |
|
|
What do you tell a pt who is asking about her concern over being vaccinated because she is breastfeeding?
|
-breastfeeding is not a contraindication for maternal immunization.
-also, vaccination is not a substitute for pediatric immunization. |
|
|
What kind of drug should be used in most pts w/ uncomplicated HTN? When should a second drug be used, and is this common?
|
-Thiazide type diuretics should be used w/ most pts w/ uncomplicated HTN
-Most need two or more drugs for goal BP less than 140/90 or 130/80 for pts w/ DM or chronic kidney disease. -If BP >20/10mmHg above goal BP, therapy w/ two agents, one of which usually should be a thiazide-type diuretic |
|
|
What are the 4 different blood pressure classifications in adults?
|
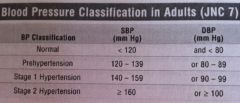
|
|
|
What are the compelling indications (6 total) for specific recommended drugs for HTN and what are the drugs?
|
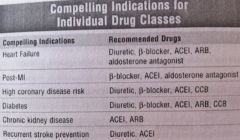
ACEI= angiotensin converting enzyme inhibitor
ARB= angiotensin receptor blocker BB= beta blocker CCB= calcium channel blocker |
|
|
Is angina usually experienced by women before a heart attack?
|
Yes but it may be atypical: upper abdominal pain, dyspnea, nausea, fatigue. Or also in neck, jaw, back and shoulders, pelvis, vauge fatigue. Classic picture not identified in women.
2/3 cardiac deaths in women are asymptomatic. Incidence lower in women, but post-MI morbidity is higher. |
|
|
How common is mitral valve prolapse in women, what is the symptomatology, and how do you assess for it?
|
-affects 6% of women
-associated w/ autosomal dominant inheritance -heard best at aortic area, late systolic apical murmur w/ a midsystolic click, widely spaced physiologic S2. -differential: thyrotoxicosis, MI, gastritis, esophageal reflux, pericarditis, angina |
|
|
Define hyperlipidemia and what it is a major risk for.
Describe associated symptoms, and physical exam findings. |
-elevated or abnormal levels of plasma lipids.
-risk factor for coronary artery disease -usually asymptomatic -PE: possibly carotid bruit, corneal arcus, xanthoma, hypertension |
|
|
What is the first line and on suggested treatment(s) for hyperlipidemia?
|
-management is to reduce LDL and total cholesterol levels w/ lifestyle mods for 3-6 months or drugs if necessary.
-Meds: vit B6 to reduce homocysteine levels,"statins" HMG-CoA, reductase inhibitors include Lescol, Mevacor, Pravachol, Zocor, Lipitor. May cause liver damage, muscle weakness, and GI distress. Niacin and bile acid sequestrants may be added to statins to lower the LDL even more, fibric acid derivatives like Lopid. -Educate: diet, exercise, med regimens & S/Es. -Follow-Up: support, reinforcement, monitoring of liver functions if on statins. |
|
|
the symptoms of dyspnea on exertion, palpitations, angina pectoris, light headedness, syncope, anorexia, and tinnitus can be symptoms of what?
|
Anemia
|
|
|
What physical assessment signs might you see upon assessment of someone w/ anemia?
|
-Pallor of the mucous membranes and skin
-Mild tachycardia -Peripheral edema -Systolic ejection murmurs from increased flow |
|
|
What things in a pts history could support the suspicion of anemia?
|
Blood loss
Alcohol abuse Diarrhea Jaundice Gallstones Chronic disease Drugs Familial causes |
|
|
What blood tests would possibly be appropriate for anemia?
|
(CBC)
-Mean corpuscular volume (MCV) Microcytic= small, iron deficience and thalassemias. Macrocytic= large, megaloblastic anemias. -Mean Corpuscular hemoglobin Concentration: color -Serum Ferritin: reflects iron stores -Reticulocyte count: young non-nucleated RBCs, a way to monitor RBC function. Ref=0.5-1.5%. Increased means production is accelerated (hemolyitc anemia, sickle cell, 3-4 post hemorrhage, cancer, splenectomy, slight increase in preg.). Decreased= iron deficiency, pernicious anemias, aplastic anemias, chronic infection, radiation therapy. -Differentiate between bone marrow production slow down and hemorrhage/hemolysis. -Check effectiveness of therapy and bone marrow recovery |
|
|
In iron deficiency anemia, what can be the causes and what lab tests and treatment would you do?
|
-Causes: blood loss, dietary deficiency, increased demand (pregnancy, lactation, adolescence)
-Labs: CBC--> RBC indicies change when Hgb falls below 8-9 MCHC (hypochromia)/Microcytosis (MCV) = pale, small RBCs, TIBC increases and serum iron is low. Iron stores can be determined by serum ferritin levels(10-200 ug/ml). -Plan: do CBC, confirm w/ serum iron, TIBC, saturation, serum ferritin. Follow up tests after treatment w/ iron supplements (325mg BID-TID) and iron rich foods. -Iron better absorbed if taken between meals but tolerated w/food sometimes. |
|
|
What is megaloblastic anemia usually caused by?
|
Folic acid deficiency or lack of B12 in diet
CBC = macrocytic RBCs (MCV), may be hypo or normo chromic |
|
|
What causes the sickling of RBCs in sickle cell anemia, how do you diagnose it, and what are the most common clinical manifestations?
|
-O2 reduction triggers sickling
-Manifestations: vaso-occlusive crisis -This is a homozygous expression of heoglobin S, if person just a carrier usually no clinical manifestations -Diagnosis by hemoglobin electrophoresis |
|
|
What is a basic definition of thalassemia?
|
Inherited disorder of hemoglobin synthesis, characterized by absent or diminished production of hemoglobin chains.
|
|
|
What is the difference between Alpha thalassemias and Beta thalassemias?
|
-Alpha talasemia trait: mild microcytic and hypochromic, if person had homozygous thalassemia probably not compatable w/ life.
Beta thalassemia minor (trait): decreased beta hemoglobin chains, usually microcytic/hypochromic anemia (mild). Might get worse in pregnancy because of hemodilution. Homozygous beta life expectancy is reduced, pregnancy probably not possible and very dangerous. |
|
|
What is the general treatment for Alpha/Beta thalassemias?
|
Treat iron deficiency as normal, but if not there don't because may cause iron overload.
Folic acid in pregnancy |
|
|
Define G6PD deficiency
|
X linked hereditary red blood cell enzyme deficiency
Female carriers usually asymtpomatic, but ingestion of some drugs (sulfonamides, nitrofuantoin or foods like favabeans or viral/bacterial infections) can cause mild hemolytic anemia. |
|
|
What are the implications to G6PD deficiency?
|
-increased incidence of UTIs
-Fetal exposure (or through breast milk) of maternal ingestion to the oxident drugs can cause hemolysis, fetal hydrops, and fetal death. |
|
|
What laboratory tests are appropriate for G6Pd deficiency?
|
-normal MCV but decreased erythrocytes and H&H.
-iron studies normal G6PD levels decreased -Electrophoresis normal -Total bilirubin elevated during hemolysis -Ehrlich stain=at or >5 Heintz bodies in 40% of RBCs. |
|
|
Compare the different results of an electrophoresis (see other side of this card)
|
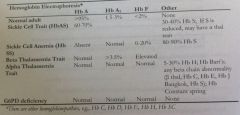
|
|
|
What is the most common type of carcinoma (skin cancer) and what are the risk factors/appearance
|
-basal cell carcinoma
-sun exposure, fair skin, >40y/o -looks like small papule that crusts over and over and bleeds -metastisis is uncommon |
|
|
What is the second most common type of carcinoma (skin cancer) and what are the risk factors/appearance
|
-squamous cell carcinoma
-skin, oral cavity, tongue, epithelium (scalp, back of hand, ear). -Appears as actinic keratosis or leukoplakia (white patch) on lips, oral mucosa or vulva. -usually begins as reddish-purple papule or plaque w/ scaly or crusted surface. -may mimic dermatits or appear nodular or warty and might itch/bleed. -More likely to metastisize than basal cell carcinoma |
|
|
What is the leading cause of cancer death in women <35 y/o?
|
-Malignant melanoma
-2/3 of deaths from skin cancer |
|
|
What are the risk factors for malignant melanoma, symptoms, and the ABCDs on physical exam?
|
-Risk: hx 6 or > sunburns, excessive sun exposure in first decade of life, indoor occupation w/ intense intermittent sun exposure, large congenital hairy nevus, fam hx, immune dysfunction. 40-50% arise from pigmented moles.
-may occur anywhere on body -Symptoms: enlargement, color change, pain/itch, bleeding -ABCDs: asymmetry, border (irregular), color (haphazard shades brown, blue, red, gray), diameter >6mm, surface or sensation difference. |
|
|
What is the treatment aim for acne? What kind of COCs would be better for this type of pt?
|
prevent scaring
use low androgen formulation like ortho try-cyclen |
|
|
What is the treatment for rosacea?
|
topical metronidazole gel or cream w/ oral abx if severe (ref->dermatologist)
|
|
|
How do you calculate BMI and what are the optimal BMIs for ages 25-35 and over 35?
|
weight (pounds) X 703 divided by [height (in.) squared]
Ages 25-35= BMI 19-25 Ages >35= BMI 21-27 |
|
|
Briefly define Hashimoto's disease
|
Chronic autoimmune throiditis
Has thyroid antibodies Average age onset 30-50 Differentiated by presence or absence of goiter |
|
|
Briefly discuss hyperthyoidism
|
Usually Graves disease
Usually presents w/goiter and exopthalmos increased T3, decreased TSH |
|
|
If you find a thyroid nodule, you need to _______
|
rule out cancer
thyroid scan, aspiration of nodule |
|
|
What are the different TSH levels?
|
Normal 0.1-5.0 (some sources 0.3-6mu)
|
|
|
What are the basic treatments for thyroid disease?
|
Hypo- levothyroxine sodium
Hyper- PTU or methimazole Evaluate q3 months Serum at upper end of normal and TSH at lower end of normal Euthyroid state takes 4-6wks |
|
|
What is the most common endocrine disorder?
|
diabetes mellitus (DM)
|
|
|
What is the target hemoglobin A1c (HgA1c) in a DM pt?
|
Below 7.2%
|
|
|
What are the blood glucose diagnostic results for diagnosing Diabetes Mellitus Type 1?
|
Random plasma glucose > or at 200
Fasting > or at 126 2hr 75gram load post glucose > or at 200 |
|
|
What is usually needed at minimum to treat DM type 2?
|
Diet
Exercise Oral hypoglycemic medication |
|
|
Diabetic ketoacidosis is seen in DM Type ___, and hyperglycemic nonketotic syndrom is seen in DM Type ___. What is hyperglycemic nonketotic syndrome?
|
Hyperosmolar syndrome
severe hyperglycemia (>600) No ketosis Hyperosmolarity and profound dehydration More common in older adults Lethargy, confusion and eventually coma Tx- insulin, fluid replacement, correction of electrolyte imbalance |
|
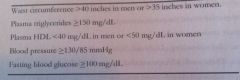
What is metabolic syndrome, and what should the MW make sure of in ongoing evaluation w/ the pt?
|
-insulin resistance syndrome or syndrome X, increases risk of cardiovascular disease and Type 2 DM
-pts should be screened regularly for DM -lifestyle changes ASAP reduce mortality from HTN, DM, cardiovascular disease (weight loss, exercise, treat dyslipidemia, enhance insulin sensitivity). -metabolic syndrome includes three of the following (see picture) |
|
|
What difference in presentation does influenza have vs the common cold?
|
influenza has an abrupt onset w/ high grade fever/malais etc. common cold pt presents w/ more of the erythmatous nasal/oropharyngeal irritation and low grade fever.
Both warrant: rest, hydration, Tylenol. Common cold: decongestants, zinc losenges started w/in 24hrs of onset. Influenza: may use antiviral medications amantadine or rimantadine |
|
|
When would you consider antibiotics for a throat infection?
|
Reasonable approach: treat all pts w/ fever, systemic symptoms, tonsillar exudate.
PCN K 500mg PO BID-TID PCN G 1.2million units Erythromycin 250-500mg po q6 for 10 days |
|
|
A pt presents w/excessive tearing, pale mucous membranes. All other systems negative. What is your main differential dx, tx?
|
Allergic rhinitis
Antihistamines: Chlor-Trimeton, Zyrtec, Claritin Nasal Steroids: Flonase, nasocort Ipratropium nasal spray |
|
|
How does vasomotor rhinitis differ from allergic rhinitis (presentation) and how would you treat this?
|
Vasomotor: nasal swelling engorgement w/out allergy or infection due to recumbency, cold, humidity, pregnancy
Meds: oral or topical decongestants. Afrin, nasal steroids, ipratropium nasal spray. Basically same tx as allergic rhinitis but w/out the antihistamine. |
|
|
This is a syndrome of acute, icteric liver inflammation, i.e., jaundice, and may even be asymptomatic spread by sexual activity, injection drug use, occupational exposure or perinatal transmission: ________
|
Hepatitis B
|
|
|
How is hepatitis B treated, and what may this infection cause long term?
|
Tx: HBV w/ antivirals alpha-interferon or lamivudine
May cause chronic illness, destruction of liver cells, cirrhosis, liver cancer, and death. |
|
|
GERD includes heartburn and often pt may present w/ noncardiac heartpain. How would you treat this pt? When would you be concerned?
|
Be suspicious: frequent/difficult to control heartburn, dysphagia, nocturnal wheezing, atypical chest pain, chronic cough, sore throat, nocturnal reurgitation.
Tx: diet modification, H2 blockers and proton pump inhibitors. Prolonged GERD: hyperplasia of junction, esphogeal lesions/cancer |
|
|
What is peptic ulcer disease?
Who is at high risk? How is it treated? |
-inflammation of the stomach or duodenum
-Male, >40, weight loss, abdominal/epigastric pain, occult blood (GERD would not have this) -Majority caused by H.pylori and should be treated (can = stomach cancer longterm) -eds: antimicrobials like metronidazole, tetracycline and acid lowering drugs. |
|
|
Diarrhea is usually self limiting, viral and sometimes bacterial. When should you be concerned?
|
Chronic diarrhea: over 2 weeks
Suspect: -parasites -absorption defects -cancer -alcoholism -hyperthyroidism -DM -inflammatory bowel |
|
|
What is the difference between cholecystitis and cholelithiasis? (in terms of primary care)
|
-Cholecystitis: inflammation
-Cholelithiasis: obstruction (gallstones) -s/s: epigastric pain, RUQ pain that radiates to back, intolerance of fatty foods, flatuence, heartburn, pruritis, jaundice. -Abdominal tenderness=cholecystitis -Jaundice= obstruction of common bile duct -drugs may dissolve stone, surgery may be needed. |
|
|
What is the most common form of joint disease and what joints are affected?
|
Osteoarthritis
Weight bearing joints -Weight loss, rest, PT. NSAIDs may or may not help. |
|
|
How is rheumatoid arthritis differentiated from osteoarthritis?
|
-systemic manifestations, peripher joints involved, fatigue, anorexia prodrome, 70-90% have RA factor, may have low back pain, sciatics.
-Refer to rheumatologist -Tx: avoidence of bad activities, cold/heat, NSAIDs/Tylenol, gradual exercise |
|
|
What is the management for carpal tunnel syndrome?
|
wrist splint
Vitamin B6 NSAIDs not very effective Reduction in repetative motions Frequest rest when must do motions Steroid injection if necessary Refer to ortho if no improvement in 6-8 weeks |
|
|
What is the T score and Z score in regards to BMD testing for osteoporosis?
|
T score: # of standard deiations from the mean of a 25-30 y/o
T score: # of standard deviations from the mean of a person the same age |
|
|
Why is osteoporosis so important?
|
2015: 41 million Americans will be dx
After a hip fx, 12-20% die in 6 months, half go to long term care facility. |
|
|
What % of osteoporosis can be affected by lifestyle factors and what modifications should you suggest?
|
-20% (80% = genetic)
- Diet: good calories, protein, vit D and calcium. If celiac disease, gluten free diet. |
|
|
What pharmacologic therapy is appropriate for osteoporosis?
|
-Bisphosphonates (Fosamax, Boniva) decreases bone turnover, = increased formation
|
|
|
What is the difference between a common migraine and classical migraine?
|
Common: w/out aura, 2 of: unilateral location, pulsating quality, moderate or severe intensity, aggravated by routine physical activity, PLUS one of: N/orV, photophobia, phonophobia
Migraine WITH aura = classical. aura lasts less than 60 min, h/a lasts 4-72hrs |
|
|
What are the (general) treatments for migraines?
|
Diet
Lifestyle Biofeedback, stress management Acute therapy (including erotamines/abortive therapy/NSAIDS) Prophylaxis (ergotamines, NSAIDS, betablocker, SSRIs etc.) |
|
|
What secondary headaches do you refer?
|
-increased intracranial pressure
-tumor -arteritis -acute effects of substance abuse -substance withdrawal -meningitis -drug rebound headache -subarachnoid hemorrhage |
|
|
What is the difference between tensions headaches and cluster headaches?
|
Tension: BILATERAL, pressing/tightness
Cluster: UNILATERAL, associated w/at least one of: lacrimation, nasal congestionn, rhinorrhea, miosis, ptosis, eyelid edema. |
|
|
What can be three causes (according to the ACNM) of seizures?
|
Metabolic disorders
Hypoglycemia Physical brain injury |
|
|
What are the five classifications of seizures?
|
-Primary generalized seizures: bilateral, symmetric w/out focal onset usually idiopathic
-Absence: brief 2-10sec. lapse of consciousness -Myoclonic: quick paroxysmal contractions of part of a muscle, group of muscles -Clonic Tonic: loss of consciuosness w/ clonic tonic convulsion, postictal confusion |
|
|
What are the general treatments for seizures, and as a Women's health care provider what is important for you to know?
|
Single drug therapy to avoid impaired effectiveness: carbamazepine, phyenytoin
SOME antiseizure meds reduce effeciveness of oral ocntraceptives. |
|
|
Define bronchitis and general treatment.
|
Usually viral, sometimes bacterial
Presents w/ productive cough, purulent sputum, rhonchi, sometimes fever, phys ex unremarkable NO abx. Maybe cough supressants. Bronchodilators like abuteral inhaler ok. ***Consider pertusis if cough lasts more than 2 weeks. |
|
|
What subjective data might a pt state who has pneumonia? What objective data might you find?
|
Caused by Strep. pneumoniae and Haemophilis influenzae.
Subjective: sudden onset of shills, 101F, rusty colored purulent sputum, chest pain, SOB. Objective: WBC at or >12,000, chest xray consolidation, culture=+ Tx: PCN V, erythromycin |
|
|
What are the signs of active TB and physical exam findings?
|
S/S: chronic cough w/ minimal sputum production, possible hemoptysis, low grade fever, weight loss, night sweats, may be asymptomatic.
Physical exam: apical rales possible, lymphadenopathy w/ cervical node, enlargement most common physical sign, often physical exam is unrevealing. |
|
|
What is the gold standard for TB diagnosis?
|
sputum culture
|
|
|
What is a major factor in increased morbidity and motality with asthma?
|
Under treatment and inappropriate therapy
|
|
|
What is an ominous sign of asthma?
|
Diminished wheezing when in distress
|
|
|
What is first line treatment for asthma?
|
Corticosteroids
|
|
|
What bacteria is responsible for most UTIs?
|
E. coli
|
|
|
What are the recommended treatment options for a UTI?
|
Bactrin
Trimethoprim Ciprofloxacin |

