![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
44 Cards in this Set
- Front
- Back
|
How does Gingivitis Develop & Occur?
|
I. Initial Lesion--Inflammatory Response to Biofilm -- 2-4 days irritaiton of bacterial accumulation--Slight marginal redness with enlargement
II. Early Lesion--Increased Inflammatory Response -- Dental biofilm thicker & older (7-14 days) -- Neutrophils -- Epithelial extensions & Rete ridges -- Gingivitis becomes evident -- **Reversible III. Established Lesion -- Chronic Inflammation -- Formation of Pocket Epithelium -- Bleeding on Probing -- Marginal Redness, bleeding on probling, spongy marginal gingiva IV. Advanced Lesion -- Bacteria from supragingival biofilm enter the sulcus & provide the source for subgingival biofilm. -- Alveolar bone destruction -- Inflammation spreades thru blood vessels to bone marrow then PL -- connective tissue fibers below JE destroyed, epithelium migrates along root surface -- coronal portion of JE becomes detached -- Pocket formation, mobility, bone loss, all signs of periodontitis -- JE continues to migrate |
|
|
Where does biofilm occur less frequently in the mouth?
|
Palatal surfaces of maxillary teeth may have the least biofilm because of the activity of the tongue.
|
|
|
What is Material Alba?
|
A loosely adherent mass of bacteria and cellular debris that frequently occurs on top of dental biofilm when biofilm removal is neglected.
|
|
|
Gingivitis develops how quickly when biofilm is left undisturbed on the tooth surface?
|
2 to 3 weeks
|
|
|
Steps for Calculus Formation?
|
Calculus formation occurs in three basic steps: pellicle formation, biofilm formation, and mineralization.
Pellicle formation: the pellicle, or cuticle, is composed of mucoproteins from the saliva and is an acellular material. The pellicle begins to form within minutes after all deposits have been removed from the tooth surface. Biofilm maturation: microorganisms settle in the pellicle layer. Colonies are formed. In early calculus the colonies consist primarily of cocci and rod-shaped organisms. By the fifth day, the biofilm is mostly made up of filamentous organisms. The colonies grow together to form a cohesive biofilm layer. Mineralization: mineralization foci (centers) form. Undisturbed, within 24 to 72 hours, more and more mineralization centers develop close to the underlying tooth surface. Eventually, the centers grow large enough to touch and unite. Mineralization first occurs within the inter-microbial matrix. The filamentous microorganisms provide the matrix for the deposition of minerals. As the deposit ages, mineralization within the bodies of the bacteria occurs. |
|
|
What is the critical pH for Enamel Demineralization?
|
4.5 to 5.5, below which the enamel demineralizes.
|
|
|
What is the most highly mineralized tissue in the body?
|
Dental Enamel
|
|
|
What is the difference between heavy calculus formers and light calculus formers?
|
Heavy calculus formers have higher salivary levels of calcium and phosphorus than light.
Light calculus formers have higher levels of parotid pyrophosphate. |
|
|
What is Dental Fluorosis?
|
It is enamel hyopomineralization that results from ingestion of too much fluoride.
Originally called "brown stain". Dr. Frederick McKay renamed it "mottled enamel". Damages ameloblasts White spots, brown spots, cracks & pitting |
|
|
What is Enamel Hypoplasia?
|
The tooth enamel is hard but thin and deficient in amount.
Two types: 1. Systemic Hypoplasia -- chronologic hypoplasia resulting from ameloblastic disturbance of short duration. White spots or pits that could become stained with food pigments, etc... 2. Local hypoplasia (affects a single tooth). White spots, may become stained. |
|
|
What is Chlorohexadine?
|
A prescription mouthwash that has a broad antibacterial activity.
Antimicrobial and anti-gingivitis agent Attaches to bacterial cell membrane causing lysis. |
|
|
What does Chlorohexadine do?
|
Prevents & controls biofilm formation
Reduces viability of existing biofilm Inhibits & reduces development of gingivitis Reduces S. Mutans |
|
|
All about Intrinsic Staining with an Exogenous Source
|
Exogenous Intrinsic Staining is staining that comes from an outside source, not from within the tooth.
Examples: 1. Extrinsic stains such as tobacco, green stains, etc.. can provide a stain that becomes intrinsic. 2. Restorative materials such as silver amalgam, copper amalgam 3. Endodontic therapy such as silver nitrate, volatile oils, strong iodine 4. Stain in dentin--carious lesion |
|
|
What is Prevalence?
|
The total number of cases of a specific disease or condition in existence in a given population at a certain time.
|
|
|
What is Epidemiology?
|
Study of disease characteristics of populations.
These studies provide information on the trends and patterns of oral health and disease in populations. |
|
|
Criteria for Selecting Indices
|
Simple to Use and Calculate.
Requires minimal equipment & expense. Uses a minimal amount of time to complete. Does not cause patient discomfort. Has clear cut criteria that is readily understandable. Free from Subjective Interpretation Reproducible by the same examiner or different examiners. Has Validity and Reliability |
|
|
What Index do you use for Primary Teeth?
|
def
|
|
|
What is the Community Periodontal Index?
|
Designed by WHO as a component of a complete oral health survey.
Purpose: to screen & monitor the periodontal status of populations. CPI was later modified to form the PSR Index for scoring individuals. |
|
|
As a DH what factors would you consider when you recommend toothbrushes?
|
1. Patient:
Ability of the patient to use the brush and remove dental biofilm from all tooth surfaces without damage to the soft tissue or tooth structure. Manual dexterity of the patient. Age of the patient & the differences in the dentition and dexterity as related to age. 2. Gingiva Status of gingival or perio health 3. Position of Teeth Crowed teeth? Open contacts? 4. Compliance Patient preference may dictate which toothbrush / method used. Patient preferences and resistance to change Patient lack of motivation, ability or willingness to follow 5. Method Selected DH preferences |
|
|
What is the most common toothbrushing method?
|
Modified Bass Method
|
|
|
How do you take care of toothbrushes?
|
Supply of brushes
Brush replacement Cleaning toothbrushes Brush storage |
|
|
Hippocrates
|
The writings of Hippocrates (300 BC) include descriptions of diseased gums related to calculus and of complex preparations for the treatment of unhealthy mouths.
|
|
|
Toothbrush Uses?
|
Biofilm Removal
Application of treatment or preventive agents (toothpaste) Contribute to halitosis control Sanitation of oral cavity |
|
|
Pivoting
|
A swinging motion of the hand and arm carried out by balancing on the fulcrum finger. The hand pivot is used to assist in maintaining adaptation of the working end.
|
|
|
Digital Motion Activation
|
Moving the instrument by flexing the thumb, index, and middle fingers.
Motion activation is the act of moving the instrument in order to produce an instrumentation stroke on the tooth surface. |
|
|
Drive Finger
|
The finger used to turn the instrument handle while holding the instrument in a modified pen grasp. Either the index finger or the thumb acts as the drive finger to turn the instrument. The finger used to roll the handle determines the direction in which the working end will turn.
|
|
|
All About the Fulcrum
|
A finger rest used to stabilize the clinician's hand during periodontal instrumentation.
It improves the precision of instrumentation strokes, prevents sudden movements that could injure the patient, and reduces muscle load to the clinician's hand. Functions: Serves as a "support beam" for the hand during instrumentation. Enables the hand and the instrument to move as one (a unit) as strokes are made against a tooth. Allows precise control of stroke pressure and length during periodontal instrumentation. Keep it straight, with the tip of the finger supporting the weight of the hand. May be 1 to 4 teeth away from tooth that is being worked on. Rest is on the same arch as the tooth being instrumented. Used as the pivot to rotate the hand and arm as well as the instrument. |
|
|
What are the parts of a sickle?
|
Design Characteristics of a Sickle:
Working-End Design--it has several unique design characteristics. a. Pointed back b. Pointed tip c. Triangular cross section d. Two cutting edges per working end e. Face is perpendicular to the lower shank--cutting edges are level with one another Face: The level cutting edges mean that the lower shank must be tilted slightly toward the tooth surface to establish correct angulation. Function: Removal of medium to large calculus |
|
|
What are the parts of a curet?
|
Design Characteristics of a Curet:
Working-End Design--it has several unique design characteristics. a. Rounded back b. Rounded toe c. Semi-circular cross section d. Two parallel cutting edges per working end e. Face is at a 90* angle to the lower shank--cutting edges are level with one another Face: Due to the face being perpendicular to the lower shank, the lower shank must be tilted slightly toward the tooth surface to establish correct angulation. Function: Removal of small to medium calculus |
|
|
Definition of Adaptation?
|
The act of placing the first 1 to 2 mm of the working end's lateral surface in contact with the tooth.
Correct adaptation of the working end to the tooth surface requires positioning the working end so that the leading-third of the working end is in contact with the tooth surface. |
|
|
What is the definition of a Periodontal Pocket?
|
A diseased sulcus.
A pocket formed as a result of disease or degeneration that caused the junctional epithelium to migrate apically along the cementum. |
|
|
What is a JE?
|
It is the soft epithelial tissue that forms the base of a gingival sulcus or periodontal pocket.
In a healthy sulcus it attaches to the enamel of the crown near the CEJ. In a Perio pocket the JE forms the base of the pocket by attaching to the root surface somewhere apical to (below) the CEJ. Attaches to the cementum of the root. |
|
|
What does it feel like when you probe and reach the base of the sulcus--the Characteristics?
|
Healthy sulcus: 1-3 mm
Periodontal pocket: >3mm Base of the sulcus or pocket feels soft and elastic (compared with the hard tooth surfaces & calculus deposits). With slight pressure, the tension of the attached periodontal tissue at the base of the pocket can be felt. |
|
|
What are the uses for Explorers?
|
Used to determine the health of the periodontal tissues, tooth anatomy, and the texture of tooth surfaces.
Specifically used to detect, by tactile means, the texture and character of tooth surfaces before, during, and after periodontal instrumentation to assess the progress and completeness of instruments. Used to examine tooth surfaces for dental anomalies and anatomic features such as grooves, curvatures, or root furcations and to assess dental restorations and sealants. |
|
|
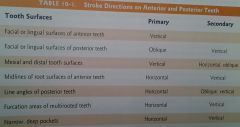
Oblique Strokes
|
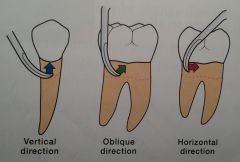
Should always be made in a coronal direction away from the soft tissue base of the sulcus or periodontal pocket.
Uses: Most commonly on Facial & Lingual Surfaces of Posterior Teeth. |
|
|
Vertical Strokes
|
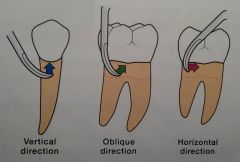
Should always be made in a coronal direction away from the soft tissue base of the sulcus or periodontal pocket.
Anterior Teeth: Use on Lingual, Facial, and Proximal Surfaces. Posterior Teeth: Use on Mesial & Distal Surfaces |
|
|
Horizontal Strokes
|
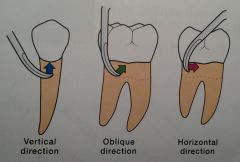
Most useful when working around the line angles of a posterior tooth or at the midline of an anterior tooth.
Working-end does NOT come in contact with JE. Posterior Teeth: Around Line Angles In Furcation Areas In Deep Pockets that are too narrow to allow vertical or oblique strokes. Anterior Teeth: Facial and Lingual Surfaces of the narrow mesial-distal width of root surface. Working End in a toe-down position. A short controlled horizontal stroke is made on the tooth surface. |
|
|
Root Debridement Stoke?
|
A type of instrumentation stroke used to remove residual calculus deposits, bacterial plaque, and by-products from root surfaces exposed due to gingival recession or within deep periodontal pockets.
Characterized by: A shaving stroke made with light pressure with the cutting edge against the tooth cementum. A stroke that is slightly longer than a calculus removal stroke. |
|
|
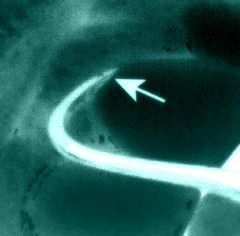
Where would you use a horizontal stroke versus the place you would use a vertical stroke:
|
|
|
|
What is an Assessment Stroke?
|
A type of instrumentation stroke used to locate calculus deposits or other tooth surface irregularities hidden beneath the gingival margin.
Characterized by: Fingers relaxed in the modified pen grasp. Feather-light strokes against the tooth surface. Also known as an exploratory stroke. |
|
|
Design Characteristics of Area Specific Curets
|
Design Characteristics of Area Specific Curets:
Cross Section: Semi-circular cross section Working-end: Rounded back and toe One working cutting edge per working-end. Face: Face tilts at approximately a 70* angle to the lower shank. One cutting edge is lower than the other in relation to the lower shank. Tilted face means that the lower cutting edge is SELF-ANGULATED--the lower cutting edge is automatically at the correct angulation when the lower shank is parallel to the tooth surface to be instrumented. Cutting Edges: Curved Cutting Edges--the curved cutting edges and rounded toe enhance adaptation to rounded root surfaces and root concavities. Application: Each curet is limited to use on certain teeth and certain surfaces. Function: Instrumentation of crown & root surfaces. Standard curets are used to remove light calculus deposits and for deplaquing. Rigid Gracey curets can remove medium-size deposits. |
|
|
All About Tartar Control Ingredients
|
Ingredients that help inhibit supragingival calculus may contain:
Pyrophosphate salts Zinc Salts (zinc chloride & zinc citrate) Sodium hexametaphosphate Triclosan / copolymer |
|
|
What are the Inorganic Components of Calculus?
|
Calcium (Ca)
Phosphate (P) Carbonate (CO3) Sodium (Na) Magnesium (Mg) Potassium (K) |
|
|
Instrument Quiz from the other day: Ms. Evans said she was going to ask questions about which Gracey you would use. Here is the information from the other day. I hope you all can read it.
|

|

