![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
36 Cards in this Set
- Front
- Back
|
Describe the process of Excitation contraction coupling in cardiac myocytes |
- depolarisation spreads along the cell membrane - this opens L-type voltage gated Ca channels - Calcium flows into the cell, activates RyR in SR - stimulates more Ca release (CICR) - Ca binds to TnC, activates cross-bridge cycling |
|
|
How is calcium restored to normal levels after depolarisation? |
Pumped out of the cell by the NCX pump (3Ca:1Na) Pumped back into SR via SERCA |
|
|
Which component of the cardiac cell membrane can regulate the speed of transmission of action potentials between adjacent myocytes? |
The number of gap junctions between the two cells. If two myocytes have a lot of gap junctions between them, the transmission will be fast. If they have few gap junctions, it will be slow |
|
|
What initiates the heart beat? |
Stimulation from the SA node |
|
|
Describe the spread of Excitation around the heart |
- Stimulation from SA node - Rapid spread around atria - Prevention of spread to ventricles by annulus fibrosis, except via AV node - AV node conducts AP through bundle of His and Purkinje fibres, AP spreads through ventricles upwards from apex of heart |
|
|
What is the purpose of the annulus fibrosus? |
To electrically insulate the atria from the ventricles in order to ensure a time delay between atrial and ventricular contraction |
|
|
What is an ECG? |
An electrocardiogram is a recording of voltage changes, made at skin level, of extracellular currents produced by myocardial depolarisation. |
|
|
How large is the typical ECG in volts? |
1 mV |
|
|
Which currents do ECGs measure? |

The electrotonic extracellular current produced when one area of the heart is depolarised while another isn't |
|
|
Why do we need multiple leads when conducting an ECG? |
Because the ECG will only measure voltages that lie in their direct plane of measurement. Any currents that flow perpendicular or oblique to the axis of measurement won't be detected |
|
|
What does isoelectric mean? |
Two cells or regions have the same potential difference |
|
|
What is Einthovens triangle? |
A set of 3 leads connecting the different limbs of the body in order to provide multiple axes of measurement for ECGs |
|
|
Where is lead 1 placed in Einthovens triangle? |
From the left to the right arm (+ve on the left) |
|
|
Where is lead 2 placed in Einthovens triangle? |
From the left leg to the right arm (+ve on left) |
|
|
Where is lead 3 placed on Einthovens triangle? |
From the left leg to the left arm (+ve on leg) |
|
|
Why is the right leg left alone in ECG lead placement? |
So it can be used for earthing the patient |
|
|
Why is the depolarisation of the SA node not seen on an ECG? |
Because it is too small and slow, so the wave that would be produced is lost in the noise of the ECG |
|
|
What is the shape of SA node depolarisation? |
|
|
|
What is the shape of atrial depolarisation? |
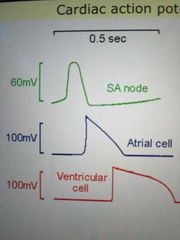
|
|
|
What is the shape of ventricular depolarisation? |
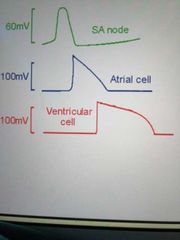
|
|
|
What event triggers the P wave? |
Atrial depolarisation |
|
|
What event triggers the QRS complex? |
Ventricular depolarisation |
|
|
What event triggers the T wave? |
Ventricular repolarisation |
|
|
Why is there a small delay between the electrical signal and the mechanical contraction of the cardiomyocytes? |
Because in this delay, ECC occurs |
|
|
When does the first heart sound occur on the ECG? |
Around the QRS complex |
|
|
When does the second heart sound occur on the ECG? |
On the descent of the T wave |
|
|
What is significant about the PR interval? |
It includes the delay that is imposed by the AV node, which allows the ventricles to properly fill |
|
|
How long should the PR interval be? |
<0.2s, if it is longer this is called heart block |
|
|
What is the significance of the ST interval? |

It should be flat, because the ventricles are contracting uniformly, meaning they are isoelectric. If it is raised, this is indicative of a STEMI |
|
|
What is a STEMI? |
ST Elevation in Myocardial Infarction - a raised ST interval on the ECG that indicates the ventricles aren't contracting uniformly. This could indicate a myocardial Infarction due to ischaemia |
|
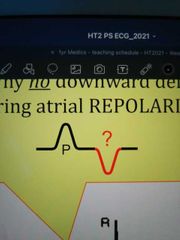
Why do you not see a downward deflection after the P wave to represent repolarisation of the atria? |
Because the AP of atrial contraction is triangular, meaning its repolarisation is much slower than its depolarisation. Because of this, the voltage between adjacent atrial myocytes undergoing repolarisation is too small to register on an ECG |
|
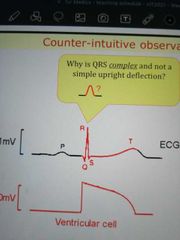
Why is the QRS complex a complex, and not a simple upward deflection? |

Because the direction of the dipole changes over the course of ventricular depolarisation |
|
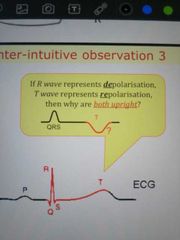
If the T wave represents repolarisation of the ventricles, why is it not a downward deflection on the ECG? |
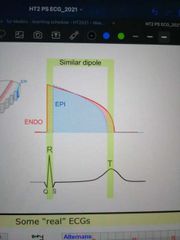
Because the epicardial cells have more K+ rectifying channels than the endocardial cells, meaning its AP is shorter. When superimposed on each other, this leads to the dipole facing the same direction for both de- and repolarisation, hence the upward deflection |
|
|
Draw a normal ECG |
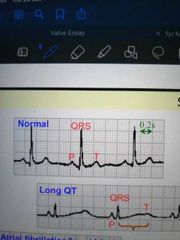
|
|
|
Draw an ECG displaying alternans |
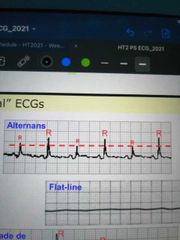
|
|
|
Draw an ECG displaying long QT syndrome |
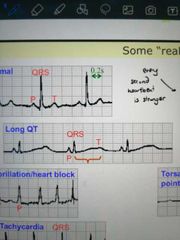
|

