![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
112 Cards in this Set
- Front
- Back
|
GI infectios agents associated with leafy vegetables or sprouts? (4)
|
1. ETEC
2. Cyclospora cayetanensis 3. Bacillus cereus 4. EHEC |
|
|
drinking unpasturized milk might lead to an infection with either which two infectious agents?
|
1. ETEC
2. Enterohemorrhagic E. coli (EHEC) |
|
|
what are the 9 GI infectious agents which can cause secretory diarrhea?
|
1. Vibrio Cholera (most profuse diarrhea)
2. ETEC 3. EPEC 4. Cryptosporidium parvum 5. Cyclospora 6. Rotavirus (most common cause in children) 7. Adenovirus (second most common in children) 8. Clostridium difficile (with leukocytes) 9. Bacillus cereus |
|
|
humans are the sole reservoire for what 2 GI bugs?
|
1. Salmonella typhi
2. Shigella |
|
|
these 4 bugs are spread in a fecal-oral transmission?
|
1. Heliobacter pylori
2. Rotavirus 3. Norovirus 4. Shigella |
|
|
which of the GI bugs are gram positive? (6)
|
1. Clostridium difficile
2. Clostridium perfringens 3. Bacillus cereus 4. Staphylococcus aureus 5. Clostridium botulinum 6. Listeria monocytogenes |
|
|
Which GI bugs like to grow on alkaline media such as TCBS? (2)
|
1. Vibrio cholera
2. Vibrio parahemolyticus |
|
|
Which GI bugs have spores? (4)
|
1. Clostridium difficile
2. Clostridium perfringens 3. Clostridium botulinum 4. Bacillus cereus |
|
|
Which GI bugs have cysts? (4)
|
1. Giardia lamblia
2. Taenia saginata 3. Taenia solium 4. Entamoeba histolytica |
|
|
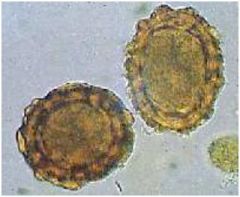
Which GI bugs have oocysts?
|
1. Cryptosporidium parvum
2. Cyclospora cayetanensis |
|
|
Which GI bugs are motile?
|
1. Vibrio cholera
2. Campylobacter jejuni 3. Yersinia enterocolitica and psuedotuberculosis (at 25 degrees C only) 4. Shigella 5. Clostridium difficile 6. Bacillus cereus 7. Listeria monocytogenes |
|
|
Which GI bugs have antibiotics as a primary treatment option? (6)
|
1. Giardia lamblia –
2. Helicobater pylori 3. Salmonella typhi 4. Yursinia spp. 5. Entamoeba hystolitica 6. Listeria monocytogenes |
|
|
Which 6 GI bugs cause damage by directly adhering to surface epithelium of the gut?
|
1. Vibrio cholerae
2. EPEC 3. Giardia lamblia 4. Entomoeba histolytica 5. Cryptosporidium parvum 6. Cyclospora |
|
|
Which GI bugs require antibiotics only when patient is immunocompromised?
|
1. Cryptosporidium parvum
2. Campylobacter jejuni 3. Shigella 4. Enteroinvasive E. coli (EIEC) |
|
|
Which GI bugs are primarly infections of children?
|
1. EPEC – specifically in hospital settings
2. Rotavirus 3. Adenovirus |
|
|
What am I?
Definitive diagnosis by endoscopy with culture of the organism, rapid urease test from biopsy specimen, or histological diagnosis via silver stain? |
Helicobacter pylori
|
|
|
What am I?
Fecal culture on media with alkalin pH such as TCBS is required for definitive diagnosis? |
Vibrio cholerae
|
|
|
What am I?
A history of travel in areas with poor sanitation. Cultrue on MacConkey agar will produce growth. ELIZA for LT is positive. PCR can be used, but mostly for epidemiological reasons |
ETEC
|
|
|
What am I?
Infant or young child often recent hospitalization which bateria which grow on MacConkey agar? |
EPEC
|
|
|
What am I?
Must specifically request tests for this bug. Positive results include fecal culture growth on TCBS media and possible leukocytes in stool |
Vibrio parahemolyticus
|
|
|
What am I?
DFA and ELIZA can be used to look for fecal antigens and for cysts or trophozoites |
Giardia lamblia
|
|
|
What am I?
Identification of oocysts in feces using concetration techniques and specialized acid fast stains. DFA can be used to look for oocysts as well. |
Cryptosporidium parvum
|
|
|
What am I?
Stool examination and ID of oocysts based on wet-mount examination and size. DFA and acid fast characteristics of oocysts may also be utilized. |
Cyclospora cayetanensis
|
|
|
What am I?
Seen frequently in children. Agglutination, ELIZA, and EM can be used. At peak infection fecal excretion exceeds 10 to the 11th. |
Rotavirus
|
|
|
What am I?
Ususally associated with clusters of gasteroenteritis. Antigen detection by EIA, PCR, or EM. Responsible for cruise ship gastroenteritis outbreaks. |
Norovirus
|
|
|
What am I?
Diagnosis is primarly based on clinical signs and history. Some ELIZA, PCR, and nucleic acid hybridization is becoming availible. |
Adenovirus
|
|
|
What am I?
isolation of organism from blood, bone marrow, stool, or urine. Stool and urine cultures are not very sensitive. Serological typing is recomended. |
Salmonella typhi
|
|
|
What am I?
Clinical signs including presence of fecal leukocytes and sometimes blood as well as history are important. Fecal culture with serotyping is needed for diffinitive diagnosis. |
Salmonella typhi
|
|
|
What am I?
presumptive diagnosis is presence of leukocytes, blood, and motile microorganisms in feces on wet mount examination. Definitive diagnosis requires fecal culture. |
Campylobacter jejuni
|
|
|
What am I?
Definitive diagnosis requires stool, blood, and abcess cultures. Labs must be told to suspect organism. |
Yersinia spp.
|
|
|
What am I?
presence of blood in stool and a large number of fecal in a fibrile patient. Bacterial culture and serotyping is necessary for definitive diagnosis. leukocytes |
Shigella
|
|
|
What am I?
Fecal leukocytes and blood in stool. Patient is usually fibrile. Definitive diagnosis involves isolation of organism, serotyping, and tissu culture invasiveness tests (very special testing site required). |
EIEC
|
|
|
What am I?
Blood diarrhea without fecal leukocyte. Definitive diagnosis is isolation of organism and culture is positive on sorbitol MacConkey agar followed by serotyping. Shiga toxin using EIA is positive |
EHEC O:157
|
|
|
What am I?
Cases of bloody diarrhea without fecal leukocyte. No growth on sorbitol MacConkey agar. Shiga toxin is detected with EIA testing. |
non O:157 EHEC
|
|
|
What am I?
Endoscopy reveal punctate hemorrhage areas or small ulcers with exudative centers in colon. Large cyst with 1-4 nuclei or trophozoite can be visible in a fresh wet mount. Trophozoite may have ingested RBCs in it. Optimal sensitivity requires a premanent Trichrome stain. Extraintestinal diagnosis is best made with DFA from an abcess |
Entamoeba histolytica
|
|
|
What am I?
Endoscopy reveals pseudomembranous colitis in severe cases. ELISA or tissue culture can reveal cytotoxin in feces. Rapid diagnosis is crucial! |
Clostridium difficile
|
|
|
What am I?
Usualy and epidemilogic investigation. Diagnosis is dependent on isolation of strains from blood source that match those in food. |
Clostridium perfingens
|
|
|
What am I?
can cause rapid vomitting or lead to watery diarrhea. Up to 10 to the 10th organisms needed for infection to occure. Definitice diagnosis occurs when isolation of the organism from food source occurs. |
Bacillus cereus
|
|
|
What am I?
Usually epidemologic investigation. Dependent on ID of toxin and toxin produing strains |
Staphylococcus aureus
|
|
|
What am I?
laboratory diagnosis is largely dependent on injection of the patient's blood mice (toxin-antitoxin neutralizing tests in mice). Culture and isolate organism from food or wound if possible. |
Clostridium botulinum
|
|
|
What am I?
Considered for any patient with meningitis or meningoencephalitis. Gram stain of CSF reveals negative bacteria. Hard to differentiate from other gram negative causes of meningitis. |
Listeria monocytogenes
|
|
|
Enzyme that is necessary for colonization of the antrum by heliobacter pylori?
|
urease
|
|
|
how is the shape of Vibrio cholerae described?
|
comma-shaped
|
|
|
Incubation period?
Helicobater pylori |
> 7 days
|
|
|
Incubation period?
Giardia lamblia |
7-14 days
|
|
|
Incubation period?
Vibrio cholerae |
24-72 hours
|
|
|
Incubation period?
ETEC |
24-72 hours
|
|
|
Incubation period?
EPEC |
24-72 hours
|
|
|
Incubation period?
Vibrio cholerae |
8-48 hours
|
|
|
Incubation period?
Rotavirus |
24-96 hours
|
|
|
Incubation period?
Caliciviruses |
48-96 hours
|
|
|
Incubation period?
Adenoviruses |
3-10 days
|
|
|
Incubation period?
Salmonella sp. |
8-48 hours
|
|
|
Incubation period?
Campylobacter jejuni |
2-7 days
|
|
|
Incubation period?
Yersinia spp. |
1-10 days
|
|
|
Incubation period?
Shigella |
24-72 hours
|
|
|
Incubation period?
EHEC |
72-96 hours
|
|
|
Incubation period?
EIEC |
24-72 hours
|
|
|
Incubation period?
Entamoeba hystolitica |
1-3 weeks
|
|
|
what are the 2 GI bugs that require only a small inoculum level?
|
1. rotavirus
2. Shigella |
|
|
List all the bugs that infect duodenum?(2)
|
1. Giardia lamblia
2. Cryptosporidium parvum |
|
|
List all the bugs that infect the jejunum? (9)
|
1. Giardia lamblia
2. Cryptosporidium parvum 3. Vibrio cholerae 4. ETEC 5. EPEC 6. Vibrio parahemolyticus 7. rotavirus 8. caliciviruses 9. adenoviruses |
|
|
List all the bugs that infect the illeum? (3)
|
1. Salmonella
2. Campylobacter jejuni 3. Yersinia spp. |
|
|
List all the bugs that infect the colon? (7)
|
1. Campylobacter jejuni
2. Yersinia spp. 3. Shigella spp. 4. EHEC 5. EIEC 6. Entamoeba histolytica 7. Clostridium difficile |
|
|
Which of the GI bugs produce non-cytolytic enterotoxins? (3)
|
1. Vibrio cholerae
2. ETEC 3. Clostridium difficile |
|
|
Which of the GI bugs produce cytolytic enterotoxins? (7)
|
1. Vibrio parahemolyticus
2. Campylobacter jejuni 3. Yersinia spp. 4. Shigella spp. 5. EHEC 6. EIEC 7. Clostridium difficile |
|
|
which GI bugs are associated with osmotic diarrhea?
|
1. Giardia
2. Cryptosporidium parvum |
|
|
what are the 2 most common ways to diagnose helicobacter pylori infection?
|
C14 urease test and H. pylori stool DFA
|
|
|
What am I?
Attaches to algea, shells, and copepods and can enter dormant state when conditions are unfavorable. Epidemics tend ot occure in hot weather. |
Vibrio cholerae
|
|
|
what is the inoculum level for an infection with Vibrio cholerae? (high, medium, low)
|
high
|
|
|
Hypovolemic shock, renal failure, and death might be the result of what GI infection?
|
Vibrio cholerae
|
|
|
Lactated Ringer's solution is given to patients with this GI infection?
|
Vibrio chorlerae
|
|
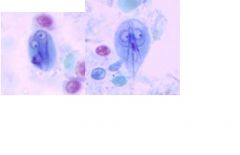
What GI bug is this?
|
Giardia lamblia
|
|

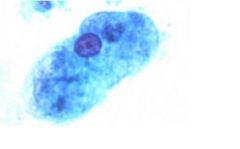
What is this?
|
Enterobius
|
|
What is this?
|
Giardia
|
|
What is this?
|
Strongyloides
|
|

What is this?
|
Taenia
|
|
|
This can grow in undercooked meat if it has at least 12 hours?
|
EHEC
|
|
|
Found in meats that are kept warm for long periods of time like gravy on a buffet and incubation time is 8-12 hours?
|
Clostridium perfringens
|
|
|
Produces preformed toxin in rice and symptoms begin 6-8 hours after ingesting toxins?
|
Bacillus cereus
|
|
|
Leafy vegetables, milk, and tap water all all means by which this GI bug gets spread?
|
ETEC
|
|

What GI bug is this?
|
ETEC
|
|
|
What am I?
Primarily confined to infants and young children, especially in institutional settings. Causes secretory diarrhea. |
EPEC
|
|
|
What am I?
Pleomorphic gram negative rod that produces ST toxin and is locally invasive. You can get it by eating seafood. |
Vibrio parahemolyticus
|
|
|
Jimbo ate jumbo shrimp at a seafood resteraunt. A day later he had watery diarrhea. 2 days later he noticed some blood in his diarrhea and came into see the doctor. How long will his diarrhea continue?
|
another two days or so, he has infection with Vibrio parahemolyticus
|
|
|
what is the kanagawa test used to diagnose?
|
Vibrio parahemolyticus
|
|
|
2 weeks after swimming in a nearby stream a male patient presents with watery diarrhea, cramps, bloating, and flatulence. This is likely an early infection by which GI bug?
|
Giardia lamblia
|
|
|
What would you give to a person infected with Giardia?
|
metronidazole
|
|
|
You become ill after swimming in a river near a water sanitation plant. When you call the plant they claim it is not their fault because the chlorinate there outflow water. You tell them that this treatment does not rid the water of which organism?
|
Cryptosporidium parvum
|
|
|
what is ingested that results in an infection with Cryptosporidium parvum?
|
oocysts from water
|
|
|
what is ingested that results in an infection with Giardia?
|
cysts, only need around 100
|
|
|
Patient presents with diarrhea for 15 days. Endoscopy reveals inflammation of small intesting and tissue histology shows loss of microvilli. What is the GI bug? The patient is HIV positive, what would treatment be?
|
Cryptosporidium parvum, give spiramycin or paromomycin
|
|
|
after swimming in the community pool 4 days ago, patient has watery diarrhea. Acid fast stains are positive for which organism?
|
Cryptosporidium parvum
|
|
|
if you were forced to eat a 2 day old sandwich contaminated with feces from a person with Cryptosporidium parvum or Cyclospora cayetanensis which would you choose?
|
Cyclospora cayetanensis becuase oocysts are only infectious after 5 days post defecation
|
|
|
What GI bug am I?
Oocysts are autofluorescent on a wet mount |
Cyclospora cayetanensis
|
|
|
how can you prevent the spread of Cyclospora cayetanensis?
|
sanitation of fruits and vegetables
|
|
|
anytime you see crazy amounts of watery diarrhea think of which GI bug?
|
Vibrio cholerae
|
|
|
What am I?
I have a double layered capsul, non envelope, and 11 segments of dsRNA coding for Virus-Specific Proteins (VP)? |
Rotaviruses
|
|
|
VP7 and VP4 proteins allow provide for what type of immune response for rotaviruses?
|
providing epitopes for virus neutralization
|
|
|
whats the vaccine for rotavirus?
|
RotaTec
|
|
|
what are the two viral agents that can be associated with sea food?
|
Hepatitis A and Noroviruses
|
|
|
PCR is routinely used to diagnose this virus?
|
Norovirus
|
|
|
what are the two most important serotypes of adenovirus?
|
40 and 41
|
|
|
how can you tell the difference between rotaviruses and adenoviruses
|
longer incubation and clinical course (8-12 days)
|
|
|
what are the Vi antigens of salmonella?
|
capsular antigens
|
|
|
H antigens are associated with which cellular component?
|
flagellar
|
|
|
A patient presents with fever, headache, abdominal pain, bradycardia, splenomegaly, and leucopenia. What does the patient suffer from?
|
Enteric fever cause by Salmonella typhi
|
|
|
how do Salmonella typhi bacteria attach to epithelial cells of ileal microvilli?
|
specific adhesion via mannose-containing receptors
|
|
|
how do Salmonella typhi get into the mesenteric lymphatics?
|
they are ingested by macrophages in Peyers patches and then carried to the lymphatics
|
|
|
describe the pathogenesis of enteric fever starting with mesenteric lymph infiltration via macrophages?
|
from lymph they get to the blood stream via thoracic duct and cause a primary bactermia. Many organs are infected and secondary more severe bactermia occurs. The gallblader becomes seeded. Constant release from gall bladder propagates further infection over time.
|
|
|
what will you find in the ileum with a person infected with Salmonella typhi?
|
necrosis and typhoid ulcerations around Peyers patches
|
|
|
Patient presents with dry cough, epistaxis, anorexia, adbdominal tenderness, and headache. Over next week rise in body temp and development of serious illness occurs. What is the GI bug responsible?
|
Salmonella typhi
|

