![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
59 Cards in this Set
- Front
- Back
|
List the steps of platelet activation following blood vessel injury:
|
Rolling adhesion --> Firm adhesion of platelets to subendothelial matrix proteins eg. collagen & vWF by glycoprotein receptors on platelets
Secretion of platelet granule contents Generation of TXA2 Shape change: Discoid --> spherical --> stellate Expose P-selectin and phosphatidylserine (PS) on platelets Activate fibrinogen receptor, GP IIb/IIIa - platelet-platelet aggregation |
|
|
Name the platelet granule contents that are secreted on activation of the platelets:
|
ADP
Epinephrine Calcium vWF PDGF |
|
|
Name the two categories of hemorrhagic platelet disorders:
|
Thrombocytopenia
Platelet dysfunction |
|
|
Clinical presentation of platelet disorders:
|
+ Mucocutaneous bleeding
+ Petechiae + May have hx of easy bruisability |
|
|
What is the normal range of platelets?
|
150,000 - 440,000 per ul
|
|
|
Define thrombocytopenia:
Mild Moderate Severe |
thrombocytopenia: Platelet count < 150,000/ul
Mild 50,000/ul - 150,000/ul Moderate 20,000/ul - 50,000/ul Severe < 20,000/ul |
|
|
What is the first step in evaluating thrombocytopenia?
|
Complete blood count
Platelet count |
|
|
How does pseudothrombocytopenia arise?
|
When EDTA is used, it may cause platelet clumping and thus produce smaller count. A peripheral blood smear should be analyzed to rule this out.
|
|
|
Name conditions in which isolated thrombocytopenia (ITP) is the only major finding:
|
Immune thrombocytopenic purpura
Drug induced thrombocytopenia |
|
|
What is the cause of thrombocytopenia in ITP?
|
Autoimmune destruction of peripheral platelets.
Most platelets are destroyed in the spleen. Macrophages with Fc receptors for IgG are responsible for this destruction. The autoantigen targeted by the IgG is glycoprotein IIb/ IIIa |
|
|
Name the two major forms of ITP
|
Acute & Chronic
|
|
|
Char of acute ITP:
|
Children,
Usually after viral infection, Self ltd - usually goes away in 6 - 12 months Sx: Petechiae, epistaxis, bruises |
|
|
Char of chronic ITP:
|
In adults
Insidious onset More in females May be seen in patients with SLE |
|
|
Receptor:Glycoprotein Ib/IX/V
Ligand: vWF |

Name the platelet receptor and ligand (on damaged subendothelial matrix) that are called to play in the attachment & rolling of activated platelets
|
|
|
What is the pathophysiology of drug induced thrombocytopenia?
|
Destruction of platelets
|
|
|
These drugs cause thrombocytopenia by suppressing platelet production:
|
Chemotherapeutic agents
Ethanol Thiazides |
|
|
Names drugs that are known to cause thrombocytopenia by the destruction of platelets:
|
Quinine
Quinidine Heparin Sulfonamides Gold salts Antibiotics Sedatives Tranquilizers Anticonvulsants |
|
|
Define pancytopenia
|
A decrease in the concentration of the three major cell types found in blood: RBC, all WBC and platelets
|
|
|
Schistocytes: Fragmented RBC's that appear as helmet cells.
|
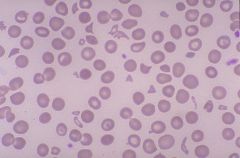
What type of cells are seen in this picture that are indicative of microangipathic hemolytic anemia and seen in peripheral blood smears of patients with DIC and TTP?
|
|
|
Name conditions that cause thrombocytopenia associated with other clinical problems:
|
Aplastic anemia - Bone marrow failure
Bone marrow filled with immature leukemia cells Megaloblastic anemia Hypersplenism - splenomegaly & pancytopenia DIC TTP HIV infection Massive hemorrhages Post-transfusion purpura Antiphospholipid antibody syndrome |
|
|
The pentad clinical manifestations seen in patients with TTP secondary to arterial & capillary occlusion are:
|
Neurological abnormalities
Renal impairment Thrombocytopenia Fever Microangiopathic hemolytic anemia |
|
|
Both DIC and TTP may present with severe thrombocytopenia and microangiopathic hemolytic anemia. How do you tell them apart?
|
COAGULATION TESTS are usually normal in TTP. DIC has abnormal coagulation tests.
|
|
|
In most cases, patient may have isolated TTP. What conditions are found in association with TTP?
|
Infection, pregnancy, immune disorders, ADAMTS13 - vWF cleaving protease that is absent or defective in familial TTP.
ADAMTS13 - absent in sporadic TTP |
|
|
What is the best way to treat familial TTP as compared to sporadic TTP:
|
Familial - plasmapheresis - want to exchange bad for good
Sporadic - Plasma infusion because ADAMTS13 is missing in these patients |
|
|
Describe the pathophysiology of thrombocytopenia in HIV positive individuals:
|
Could be due to:
+ Platelet destruction + Suppression of platelet production + Secondary to anti-retrovirals |
|
|
Pathophysiology of pancytopenia associated with massive hemorrahges:
|
+ Loss of blood - loss of RBC's and WBC's and platelets. Blood transfused does not have viable platelets due to the fact that it was stored at 4C. This and the dilution factor due to the transfusion --> thrombocytopenia. How to take care of this? Platelet transfusion.
|
|
|
Name this condition that causes alloimmune thrombocytopenia due to blood transfusion but is due to HPA-1a positve blood from donor to recepient without this antigen. This needs to be differentiated from dilution of blood due to transfusions:
|
Post-transfusion purpura
|
|
|
The pathophysiology of thrombocytopenia in this condition is sequestration:
|
Hypersplenism
|
|
|
These etiologies cause thrombocytopenia due to decreased production of platelets:
|
Inflitration of bone marrow
Hypoplasia HIV Ineffective production - megaloblastosis |
|
|
These conditions cause thrombocytopenia due to increased destruction of platelets:
|
Immune: ITP, Drug induced thrombocytopenia, HIV
Non-immune:DIC, TTP and sepsis |
|
|
Name conditions that cause alloimmune mediated platelet destruction:
|
Neonatal alloimmune thrombocytopenia
Posttransfusion purpura Platelet transfusion refractoriness |
|
|
Define the term alloimmune:
|
This a condition in which an individual gains immunity againts his/ her own cells from an individual of same species.
|
|
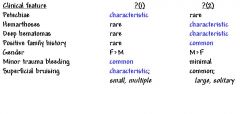
Name the defects (1) and (2)that have the clinical features listed
|
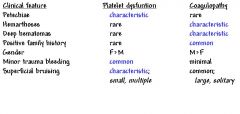
1 - Platelet defects
2 - coagulopathy |
|

Fill in the blanks:
|
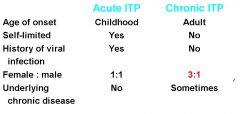
Note that in children, ITP is seen after viral infection whereas that in adults is not and tends to have more of an insiduous onset.
|
|
|
How would you treat ITP?
|
Corticosteroids for max of 6wks. If not normal then -->
IV anti-RH(d) or IV IgG or anti-CD20 ab (Rituximab)--> Splenectomy indicated. If this doesn't work then --> Immunosuppressive therapy - Vincristine Plasmapheresis |
|
|
Which two conditions associated with thrombocytopenia are Dx by exclusion?
|
ITP and Drug induced
|
|
|
What kind of platelet disorder does a patient with prolonged bleeding and normal platelet count have?
|
Qualitative platelet disorder
|
|
|
List hereditary platelet disorders:
|
Bernard Soulier syndrome: abnormal GpIb receptor
Glanzmann thromboasthenia (TSA): GpIIb/IIIa Platelet secretion defects: Storage Pool Disease (SPD):- Deficiency in secretion of ADP or serotonin (dense bodies) Grey platelet syndrome:- alpha granules --> proteins |
|
|
List acquired platelet disorders
|
Uremia - chronic renal failure
Drugs - Aspirin - irreversible block on COX, hence blocked TXA2 production. Platelet disfunction may last 7 days (until new bunch is made). Avoid ASA in hemophiliacs. Cardiopulmonary bypass Myeloproliferative disorders - stem cell Acquired vWF & storage pool disease |
|
|
Pathophysiology in cardiopulmonary bypass surgery induced platelet disorder:
|
During this surgery patient's blood goes through extracorporeal circuit where platelets are activated and fragmented - these platelets are dysfunctional.
|
|
|
Pathophysiology in chronic myeloproliferative and myelodisplastic induced platelet disorder:
|
Intrinsic platelet disorder
|
|
|
Pathophysiology in disprotenemia induced platelet disorder:
|
These platelets are coated with plasma paraprotein (abnormal protein found in urine & blood associated with multiple myeloma) which makes them dysfunctional.
|
|
|
Treatment of platelet disorders in chronic renal failure
|
Dialysis - the problem is not the platelets but the toxic plasma they are in.
Correction of Anemia with EPO has better prognosis Desmopressin - Acopy of a natural hormone that avails vWF, increase platelet aggreg. Cryoprecipitate - a blood product that contains vWF among other factors Estrogens |
|
|
What is Cryoprecipitate
|
Blood product prepared from plasma. Contains factor VIII, Fibrinogen, vWF, Factor XIII and Fibronectin.
|
|
|
Name two myeloproliferative disorders that lead to acquired platelet disorders:
|
Polycethemia vera (Excessive production of RBS and other cells in bone marrow) & essential thrombocythemia (overproduction of platelets and megakaryocytes in bone marrow)
|
|
|
These two drugs block ADP receptors on platelets and interfere with platelet aggregation:
|
Clopidogrel and Ticlopidine.
|
|
|
What is the main mgt for qualitative platelet disorders?
|
platelet transfusions
|
|
|
How do your dx qualitative platelet disorders?
|
Hx - if life long, like hereditary.
CBC - seen in both hereditary & acquired. Bleeding time: ITP may have a shorter bleeding time than normal PT, defect in vWF - the longest bleeding time. Platelet aggregation, can be used to distinguish disorder due to problem with aggregation Cytometry and molecular diagnostic tests. |
|

This chart shows the approach to Dx of thrombocytopenia. Fill in the blanks:
|

You want to rule out thrombocytopenia due to platelet aggregation if EDTA used as an anticoagulant. In addition, realize that the dx of ITP and Drug induced thrombocytopenia is one of exclusion
|
|
|
Antiplatelet drug: Aspirin
MOA t1/2 Where is it absorbed? How long does it take for platelets to be inhibited? |
MOA - Binds and inhibits Cox1 - inhibit formation of TXA2
t1/2 - 30 - 40 minutes Where is it absorbed? stomach and small intestine How long does it take for platelets to be inhibited? 1hr Note: ASA irreversible binds to COX1 - therefore inhibition of platelet lasts the lifetime of the platelet |
|
|
Antiplatelet drug: NSAIDS
MOA |
MOA - reversible binds and inhibits Cox1 - competitive inhibition
|
|
|
Antiplatelet drug: Dipyridamole (persantine)
MOA |
Inhibits cyclic nucleotide phosphodiesterase --> increase CAMP thought to have vasodialator and antiplatelet effects.
NOT A GD FRONTLINE DRUG |
|
|
Antiplatelet drug: CLOPIDOGREL
MOA t1/2 Where is it absorbed? How long does it take for platelets to be inhibited? *** MUI IMPORTANTE *** |
Antiplatelet drug: Clopidogrel
MOA - INHIBIT ADP INDUCED PLATELET AGGREGATION, NO DIRECT EFFECTS ON ARACHIDONIC ACID METABOLISM. Also inhibit platelet aggregation due to collagen & thrombin. t1/2 - 8HRS Where is it absorbed? ORALLY -RAPID ABSORPTION How long does it take for platelets to be inhibited? INHIBITION BEGINS 2HRS AFTER ORAL DOSING OF 400MG. LOWER DOSE 75MG --> STEADY STATE IN 4 -7 DAYS |
|
|
CLOPIDOGREL IS A FIRST LINE DRUG. GIVEN ITS MOA WHEN WOULD YOU GIVE IT?
|
After Heparin and Aspirin, cause would manifest its effects in 4 - 7 days. Usually given with ASA cause they do not cross-react.
|
|
|
Antiplatelet drug: Ticlopidine
MOA t1/2 Where is it absorbed? How long does it take for platelets to be inhibited? Adverse effects? |
MOA: Inhibit ADP induced platelet aggregation with no direct effects on arachidonic acid metabolism. Similar to clopidogrel.
t1/2 - 24 - 36hrs (longer after repeated dosing 96hrs) Where is it absorbed? Orally - rapid How long does it take for platelets to be inhibited? 2 weeks, not indicated for acute conditions such as unstable angina. Adverse effects? Neutropenia & TTP |
|
|
Antiplatelet drug: Abciximab Rheopro)
MOA t1/2 Where is it absorbed? How long does it take for platelets to be inhibited? |
MOA - Abciximab is a monoclonal ab that binds GpIIb/IIIa receptors on platelets and megakaryocytes. Blocks binding of fibrinogen
t1/2 - of unbound abciximab is 10-30 minutes Administered - IV infusion How long does it take for platelets to be inhibited? Decreased platelet aggregation when # of unbound receptors is < 20,000 per platelet |
|
|
Name gpIIb/IIa antagonists that are used to reduce platelet aggregation:
|
Abciximab - mab
Tirofiban - Recombinant drug - may cause severe thrombocytopenia Eptifibatide - synthetic drug |
|
|
Antiplatelet drug: Anagrelide
MOA t1/2 Where is it absorbed? How long does it take for platelets to be inhibited? |
MOA: Reduces megakaryocyte size and ploidy
Where is it absorbed?orally How long does it take for platelets to be inhibited? Reduction in platelet action over time in dose-dependent manner |
|
|
List three clinial conditions where anti-platelet drugs are useful.
|
Acute coronary syndromes
Atrial Fibrillation Transient ischemic attacks |

