![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
46 Cards in this Set
- Front
- Back
|
What are plasma proteins?
|
-macromolecules = amino acids linked by peptide bonds
-made in the liver (mostly) + plasma cells (globulins) -catabolized in GI tract, kidneys (should filter out protein tho), and liver (broken down) |
|
|
What are the fns of the plasma protein?
|
-Transport (transferrin - transports iron)
-Colloid osmotic pressure -Immune defense (c-reactive proteins - marker) -Inflammatory response -Blood clotting (coag factors are protein - fibrinogen) -Signaling |
|
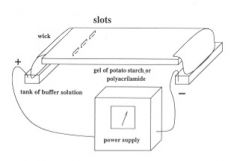
What is serum protein electrophoresis? SPEP
|
separation based on net electrical charges + size of protein molecules, properties of medium + temp
-fractionated serum proteins -patterns characteristic of disease |
|
|
graph check papers
|
52-68% of our protein is albumin. next peak is called the a.1 protein.
beta globulin gamma glublin peak - 10-22% normal distribution! |
|
|
What's the reference range for albumin?
|
3.5-5.0 g/dl (serum)
|
|
|
What are the fn's of albumin?
|
plasma oncotic pressure
transport protein blood product volume expander |
|
|
Causes of Hypoalbuminemia?
|
1) Decreased albumin synthesis
-Liver disease/failure -Decreased dietary protein -Congenital “analbuminemia” People with cystic fibrosis have low albumin if malnousihed do to the enzymes therefore low albumin Albumin tests the fn of the liver! Good for diagnosis and prognosis in those with liver disease |
|
|
Another cause of hypoalbuminemia?
|
2) Increased loss of proteins
-Renal disease with proteinuria (nephrotic syndrome - glomerulus has high permeability t.f. proteins leak out) -Burns and other skin disease (skin - major site of albumin storage!) -GI disease w/protein losing enteropathy (not absorbing) -Orthostatic proteinuria (benign, occurs in adolescent, protein loss through kidneys while standing but not while laying down. collect urine at bedtime - discard it - only get proteinuria after walking upright!) -Hemorrhage (blood has protein!) |
|
|
Another cause of hypoalbuminemia? Examples?
|
Acute/chronic inflammation + infections (vascular permeability - may leak out into ECF like lupus, rheumatoid arthritis)
|
|
|
In what situations would you see decreased albumin levels?
|
-Last trimester of pregnancy
-Oral contraceptive use (increase in plasma volume - dilution effect) -Prolonged bed rest -Overhydration (low level of albumin, fluid will shift to extravacular spaces t.f. edema occurs!) |
|
|
Are low levels of albumin considered an independent risk factor for mortality in the elderly?
|
yes
|
|
|
What is the hallmark finding of hypoalbuminemia?
|
EDEMA!
|
|
Causes of hyperalbuminemia
|
1)Severe dehydration
2) Prolonged tourniquet application before venipuncture 3) Administer too much |
|
|
What's the reference range for prealbumin?
|
10-45 mg/dl (serum)
|
|
|
What does prealbumin reflect?
|
****Reflects current nutritional status
-Short half life of 2 days -Test/follow in all hospitalized patients esp in ICU and surgical floors -Obtain nutrition consult if <15 mg/dL (not affected as much by hydration) |
|
|
What is prealbumin?
|
-transport protein (vit a, thyroid hormone)
-useful to evaluate nasal fluids (test to see if it's CSF which has higher % of albumin) |
|
|
Reference range of alpha 1 antitrypsin?
|
100-300 mg/dl
|
|
|
What is alpha antitrypsin?
|
-Predominant component of Alpha1 globulin fraction
-Inactivates trypsin + other proteolytic enzymes -Inhibits thrombin and plasmin (helps in breaking up the clots and thrombin helps make clots - both in coagulating cascade) -Acute phase reactant (protein in the plasma that increases when there's an acute inflammation!) |
|
|
If you have a congenital deficiency of alpha 1 antitrypsin what can happen?
|
Congenital deficiency syndromes
Premature emphysema Childhood cirrhosis of liver with deficiency you can develop emphysema!! |
|
|
What does the alpha 2 macroglobulin inactivate? ihibit?
|
-Inactivates many proteases
-Inhibits thrombin and plasmin -Large molecular weight - are Retained with proteinuria |
|
|
What's the compensatory increase in alpha 2 all about?
|
Compensatory increase in alpha 2 macroglobulin synthesis in nephrotic syndrome
|
|
|
Reference range of haptoglobin?
|
37-184 mg/dl
|
|
|
what should you be aware about with haptoglobin?
|
get picked up by haptoglobin, you'll have a decrease - it will be bound to hg, but we're testing for haptoglobin and we'll see a depletion IN THE SERUM. must be some intravascular HEMOLYSIS!!
|
|
|
What does haptoglobin bind to?
|
alpha 2 globulin fraction, acute phase reactant
-BINDS free hemoglobin and preserves iron |
|
|
when is haptoglobin depleted?
|
Depleted in severe intravascular hemolysis
Caution- hemolysis may be present although haptoglobin may be within reference range -acute inflammatory episode -steroid therapy |
|
|
What happens to haptoglobin after a blood transfusion?
|
slight decrease
|
|
|
Limitations to the testing of haptoglobin?
|
---**Decreased haptoglobin concentration
like with Oral contraceptives, Strenuous exercise |
|
|
Reference range of transferrin?
|
2.0-3.6 g/l
|
|
|
Describe tranferrin
|
-iron transport protein in serum (increased in iron deficiency anemia!)
-small MW -beta globulin fraction |
|
|
C-reactive protein range:
|
<.8 mg/dl
hsCRP .02 - .8 mg/dl |
|
|
What kind of reactant is c reactive protein? What is it a sensitive marker for?
|
-ACUTE phase reactant
-inflammation (sensitive) (rises within 4-6 hrs and clearly rapidly.) sensitive not specific!! |
|
|
What does c reative protein signal?
|
-signals postoperative infections
-signals transplanation rejection high sensitivity CRP elevation associated w/risk of cardiac event |
|
|
What can give you false results when taking a persons c reactive protein?
|
-lipemia or hemolysis = gives false elevated results
-fat people + women on HRT have higher levels of CRP! |
|
|
What are gamma globulins - immunoglobulins made by?
|
plasma cells!
|
|
|
What are the functions of gammaglobulins - immunoglobulins?
|
-Neutralize toxic substances
-Support phagocytosis -Destroy microorganism function |
|
|
What are the immunoglobulins?
|
IgG (75-80%) dominates in secondary immune response; crosses placenta (most abundant)
IgA (10-15%) serum and secretion protection (colostrum) IgM (5-10%) dominant antibody produced in primary immune response; ABO group Ab; doesn’t cross placenta (largest) IgD (trace) signal B cell function IgE (trace) allergic reactions (parasitic infxns) |
|
|
Describe difference between 1st and 2nd exposure.
|
during the 1st exposure, you'll make igM antibodies. second time, you'll have a faster response, and you'll make igG
|
|
|
What crosses the placenta?
|
IgG!
|
|
|
What happens if you're IgA deficient and I tranfuse you with blood?
|
IgA deficiencies in people - they can MAKE antibodies for it....igA antibodies. this can cause serious transfusion reactions!
|
|
|
If you have a really high level of gamma globulin concentration, WHAT DOES THIS MEAN?
|
-Chronic infections and malignancies
-Liver disease -Monoclonal gammopathies (proteins that are like antibodies, but not. clone of plasma cells - neoplastic - they make immunoglobulins but they're not normal! examples: Waldenstrom’s macroglobulinemia (IgM spike) (can present with anemia, splenomegaly, lymphadenopathy, high SED rate, weakness, bleeding) or Multiple myeloma (Non IgM spike) (has 10% of plasma cells in the bone marrow (too much!), has lytic bone lesions, they have punched out lesions in the bone - renal problems - kidneys do a job on them, high sed rate, anemia . think bone conditions and kidney conditions. (BOTH OF THESE CONDITIONS, will have the spike!) -Autoimmune reactions (lupus or rheumatoid arthritis) |
|
|
What is rouleaux formation related to? (anyone with rouleaux have a high sed rate!)
|
multiple myelocoma - happen with increase serum proteins, particularly fibrinogen and glubulins. this is the mechanism for the sedimentation rate, which increases non-specifically w/inflammation + increased acute phase serum proteins
|
|
|
If you have really low levels of gamma globulin concentrations, what do you have?!?!
|
Decreased levels
-Primary immunodeficiencies (don't make enough gamma globulins) (examples: Agammaglobulinemia and Hypogammaglobulinemia) Nephrotic syndrome (losing a lot of proteins!) |
|
|
What are the acute phase reactants? how do you test if they're elevated?
|
-plasma proteins that incr in response to illness, infection, trauma, and tissue necrosis
-sed RATE Alpha1 antitrypsin Antithrombin III Ceruloplasmin Complement 3 Haptoglobin Fibrinogen C-reactive protein |
|
|
Total protein reference range?
|
6.0-8.3 g/dl
|
|
|
Elevated levels of total protein is seen in what?
|
-dehydration
-excess production of gamma globulin -chronic inflammation or infection |
|
|
Decreased levels of total protein are seen in what?
|
Renal disease
Blood loss Malnutrition Liver disease Severe skin disease or burns Prolonged immobilization |

