![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
67 Cards in this Set
- Front
- Back
|
Most commonly missed injuries associated with ankle fractures
|
Achilles tendon rupture
lateral process of the talus fractures metatarsal fractures anterior process of the calcaneus fractures |
|
|
physical exam for ankle
|
skin (edema, blisters, tenting, open wounds)
pulses (DP/PT) sensation (superficial peroneal = dorsum except 1st web space, saphenous = medial ankle) ROM |
|
|
squeeze test
|
squeeze fibula and tibia in proximal calf
pain = syndesmotic disruption diagnostic for syndesmosis injury |
|
|
Thompson test
|
compression of gastrocnemius muscle and assess for plantar flexion of foot, failure = ruptured Achilles
|
|
|
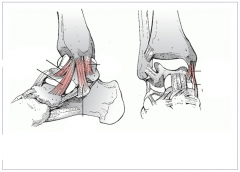
anterior drawer test of the ankle
|
stabilize tibia while cupping posterior calcaneus and imparting anterior translational force
laxity = ant talofibular lig injury |
|
|
ankle ROM
|
dorsiflexion = 15-18
plantarflexion = 39-48 inversion = 27-33 eversion = 18-27 |
|
|
Ottawa ankle rules
|
determines when should obtain xrays to eval ankle injury
- age >55 yr - inability to bear weight - bone tenderness over post edge or tip of either mal |
|
|
initial evaluation of ankle films
|
tibiotalar articulation
assess for fibular shortening widening of joint space malrotation of fibula talar tilt |
|
|
parameters that suggest unstable fracture patterns
|
lat mal displacement >2mm with talar shift on AP or lat
significant med mal displacement deltoid lig disruption (>5 mm clear space) syndesmotic injury (>5 mm tib-fib clear space, <10 mm tib-fib overlap AP or <1 mm on mort) |
|
|
talocrural angle
|
measured between a line perpendicular to tibial plafond and a line connecting the tips of the med and lat mals
|
|
|
accurate stress test
|
stress in dorsiflexion and external rotation
|
|
|
theory of Lauge Hansen classification
|
first part describes position of foot at time of injury
second part describes direction of force applied to foot |
|
|
medial mal shear fracture
|
SA2 - lateral side may be purely ligamentous
|
|
|
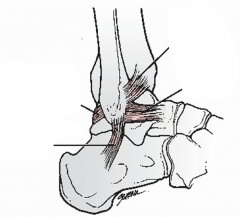
ATFL origin and insertion
|
fib origin = Wagstaffe tubercle
tib insertion = Chaput tubercle |
|
|
ways to distinguish SER2 from SER4
|
stress view
ant/post subluxation of talus >2mm shortening of fibula mild lateral subluxation without stress |
|
|
why is it important to distinguish SER2 from SER4
|
SER2 have shown to have good outcome with nonoperative treatment despite mild talar subluxation on stress views
|
|
|
ankle fracture most commonly associated with syndesmotic injury
|
PER
|
|
|
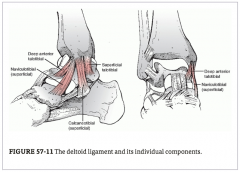
MMOLC
|
medial malleolus osteoligamentous complex:
medial mal (ant/post colliculli, intercollicular groove) superficial/deep deltoid lig insertions of deltoid |
|
|
origin of superficial deltoid
|
anterior colliculus of medial mal
|
|
|
origin of deep deltoid
|
posterior colliculus of medial mal
|
|
|
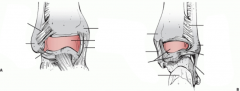
insertions of deltoid lig
|
medial tubercle of the talus
navicular tuberosity sustentaculum tali |
|
|
three components of superficial deltoid
|
ant: naviculotibial (inserts dorsomedial navicular)
mid: calcaneotibial (inserts sustentaculum tali) post: superficial talotibial (inserts medial talar tubercle) |
|
|
strongest portion of superficial deltoid
|
calcaneotibial
|
|
|
two structures of deep deltoid
|
deep anterior talotibial ligament
deep posterior talotibial ligament |
|
|
origin and insertion of deep anterior talotibial ligament
|
origin = intercollicular groove (deep to calcaneotibial)
insert = medial talus |
|
|
origin and insertion of deep posterior talotibial ligament
|
origin = intraarticular aspect of posterior colliculus
insert = medial talus |
|
|
strongest and thickest ligament of deltoid complex
|
deep posterior talotibial
|
|
|
responsible for indirect reduction of posterior mal
|
posterior tibiofibular ligament
pulls back to position when fibula brought back out to length |
|
|
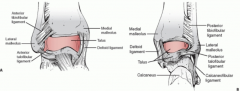
4 components of syndesmosis
|
AITFL (Chaput --> Wagstaffe)
PITFL (Volkman --> post/lat fibula) inferior transverse tib-fib lig (ITL) tib-fib IO membrane |
|
|
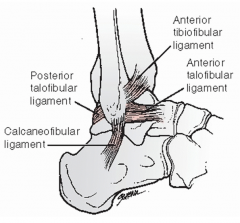
3 LCLs of ankle
|
ATFL (ant tib-fib lig)
PTFL (post talofib lig) CFL (calcaneofib lig) |
|
|
strongest of ankle LCL
|
PTFL
|
|
|
four tendon groups that cross the ankle joint
|
posterior
medial anterior lateral |
|
|
medial ankle tendon group
|
tibialis posterior
flexor digitorum longus flexor hallucis longus |
|
|
path of medial ankle tendon group
|
under lacinate lig (roof of tarsal tunnel)
|
|
|
lateral ankle tendon group
|
peroneus longus
peroneus brevis |
|
|
path of lateral ankle tendon group
|
under the superior peroneal retinaculum posterior to the fibula
|
|
|
path of anterior ankle tendon group
|
under extensor retinaculum proximal to ankle and under Y-shaped inferior extensor retinaculum just distal to ankle joint
|
|
|
location of saphenous vein and nerve
|
medial - superior to medial mal and lacinate lig
|
|
|
path of posterior tibial artery and tibial nerve
|
medial in tarsal tunnel under lacinate lig
|
|
|
location of sural nerve
|
lateral - halfway between lateral border of Achilles and posterior border of lateral mal
|
|
|
anterior ankle tendon group
|
extensor hallucis longus
extensor digitorum longus |
|
|
contents of anterior ankle
|
deep peroneal nerve
anterior tibial arteries |
|
|
pilon fractures
|
ankle fractures that involve the weight-bearing portion of the distal tibial articular surface
|
|
|
cause of substantial swelling and blistering in pilon fractures
|
bone is viscoelastic so more energy is absorbed prior to failure - which is then released and imparted to soft tissue envelope
|
|
|
methods to treat fracture blisters
|
sterile unroofing with silvadene and nonadherents
sterile aspiration with maintenance of roof leaving blister intact |
|
|
hemorrhagic fracture blister
|
dermis is free of epidermal cells --> deeper injury
|
|
|
Reudi-Allgower system for pilon fractures
|
I: intraarticular without displacement
II: displaced articular frags without comminution III: displacement and comminution |
|
|
AO/OTA pilon classification
|
A: extra-articular
B: partial articular C: complete articular (subdivisions for increasing amounts of comminution) |
|
|
Tscherne and Goetzne soft tissue injury classification system
|
0 = closed, no appreciable soft tissue injury, indirect simple fracture
1 = superficial abrasion or skin contusion, displaced fracture frags exerting pressure on skin 2 = deep abrasions and local contused skin, imminent compartment syndrome 3 = extensive contusions or crushing, significant muscle destruction and subq tissue degloving, comp syn, vasc injuries, severe fx comminution |
|
|
anterior tibial compartment (med to lat)
|
tibialis anterior
extensor hallucis longus extensor digitorum longus peroneus tertius (innervated by deep peroneal) |
|
|
lateral tibial compartment
|
peroneus longus
peroneus brevis (innervated by superficial peroneal) |
|
|
superficial posterior tibial compartment
|
gastrocnemius
soleus plantaris (innervated by tibial) |
|
|
deep posterior tibial compartment
|
posterior tibial
flexor digitorum longus flexor hallucis longus (innervated by tibial) |
|
|
contents of tarsal tunnel
|
tibialis posterior
flexor digitorum longus posterior tibial artery tibial nerve flexor hallucis longus |
|
|
three commonly observed pilon fracture segments
|
medial malleolar fragment
anterolateral (Chaput) fragment posterolateral (Volkmann) fragment |
|
|
AP radiographic eval
|
tib-fib overlap <10 mm = syndesmotic injury
tib-fib clear space >5 mm = syndesmotic injury talar tilt (diff in med/lat aspects of superior joint space >2 mm) = medial or lateral disruption |
|
|
mortise radiographic eval
|
medial clear space >4-5 mm = lateral talar tilt
talocrural angle within 2-3 degrees of uninjured tib-fib overlap <1 mm = syndesmotic injury talar shift >1 mm is abnormal |
|
|
Maisonneuve fracture
|
proximal third fibular fracture, PER variant
|
|
|
curbstone fracture
|
avulsion fracture off posterior tibia - produced by tripping
|
|
|
LeForte-Wagstaffe fracture
|
anterior fibular tubercle avulsion fracture
assoc with SER type |
|
|
Tillaux-Chaput fracture
|
avulsion of ant tib margin by ant tib-fib lig
tib counterpart of LeForte-Wagstaffe |
|
|
Mast classification of pilon fractures
|
A: malleolar fractures with sig post lip involvement
B: spiral fx of distal tib with extension into articular surface C: central impaction injuries |
|
|
Ruedi and Allgower classification of pilon fractures
|
1: nondisplaced cleavage fracture of ankle joint
2: displaced fracture with minimal impaction or comminution 3: displaced fracture with significant articular comminution and metaphyseal impaction |
|
|
|
|

|

|
|
|
|
|
|
|

