![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
128 Cards in this Set
- Front
- Back
|
Hematoxylin
|
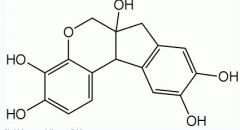
*basic
*blue/purple-colored *molecules carry positive charge-->selectively bind to negatively-charged structures in a cell *so stains blue/purple: dna, nuclei, ribosomes, chief cells, any cell with a high concentration of ribosomes or RER |
|
|
basophilic
|
a structure which has a net negative charge so as to interact with a basic stain
|
|
|
Eosin
|
stain
*acidic *red-colored *carries negative charge *bind to positively charged structures: proteins, mitochondria, parietal cells |
|
|
Eosin
|
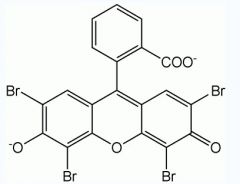
stain
*acidic *red-colored *carries negative charge *bind to positively charged structures: proteins, mitochondria, parietal cells |
|
|
acidophilic
|
structures which bind acidic stains such as eosin
|
|
|
euchromatic
|
(eu- "true") stained lightly, unwound DNA (probably active making proteins)
|
|
|
heterocromatic
|
stains dark, wound DNA inside nucleus (not making active proteins)
|
|
|
nissl body
|
basophilic structures that fill the soma and extend into the dendrites; clumps of ribosomes
|
|
|
how do you identify an axon histologically
|
* lack nissl substance
* common diameter * don't branch |
|
|
alpha motor neurons innervate...
|
extrafusal muscle fibers
|
|
|
gamma motor neurons innervate...
|
innervate intrafusal muscle fibers
|
|
|
isozyme
|
enzymes that differ in amino acid sequence but catalyze the same chemical reaction
|
|
|
functions of auaporins
|
REGULATE CELL VOLUME
secretion/absorption of CSF generation of aqueous humor in the eyes secretion of tears saliva sweat and bile renal concentratiion in urine gastointestinal absorption of water/secretion of water into the gi tract |
|
|
Normal body fluids are about ___ mOsm
|
300 milli0osmoles/liter (mOsm)
|
|
|
In the equation for osmotic pressure pi = RT Delta(C), pi =
|
pi = 19.3 mmHg/mOsm x Delta(C)
|
|
|
oncotic pressure
|
a form of osmotic pressure exerted by proteins in blood plasma that usually tends to pull water into the circulatory system.
|
|
|
1 torr = ___ mm hg = ___ Pa
|
1 torr = 1 mm Hg = 133Pa
|
|
|
nerve fibers that release acetylcholine (ach) as their NT are referred to as
|
cholinergic
|
|
|
nerve fibers that release noreinephrine are called
|
adrenergic
|
|
|
The inside of the adrenal gland is called
|
the medulla
|
|
|
parasympathetic stimulation of GI exocrine gland secretion controls
|
volume/enzyme content of secretion
|
|
|
sympathetic stimulation of GI exocrine gland secretion controls
|
mucus content
|
|
|
which structures receive only sympathetic innervation
|
smooth muscle and glands of the skin/parasympathetic nerves do not distribute to the body wall ALSO most blood vessels
|
|
|
preganglionic sympathetic motor neurons occur between which spinal cord levels
|
T1-L2 (although they can be found as high as C8 and as low as L3)
|
|
|
preganglionic cells are clustered in which spinal cord segment..
|
intermediolateral cell column and is largely organized ipsilaterally
|
|
|
a negative resting potential means..
|
the inside of the cell is negatively charged wrt the outside
|
|
|
cations have more _____ charge and are attracted towards the ____
|
cations have more positive charge and are attracted towards the negative electrode
|
|
|
anions have more _____ charge and are attracted towards the ____
|
anions have more positive charge and are attracted towards the positive electrode
|
|
|
The exchange of the K/NA pump is ___ K for every ___ Na
|
2 K for every 3 Na
|
|
|
(If you can) explain the apparent contradiction between electroneutrality and membrane potential
|
A potential depends on a charge asymmetry, but electroneutrality asummes that the charge outside is bulk neutral and inside bulk neutral. Ion exchange preserves electroneutrality, but a difference in relative permibabilties set up a potential in the MEMBRANE that keeps the ion exchange electroneutral
|
|
|
hyperosmotic
|
bath osmolarity > initial cell osmolarity --> cell shirnks
|
|
|
isomotic
|
bath osmolarity = cell osmolarity --> nothing happens
|
|
|
hypoosmotic
|
bath osmolarity < intitial cell osmolarity (cell expands)
|
|
|
Equation for osmolarity
|
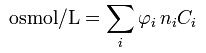
φ is the osmotic coefficient, which accounts for the degree of non-ideality of the solution. In the simplest case it is the degree of dissociation of the solute. Then, φ is between 0 and 1 where 1 indicates 100% dissociation. However, φ can also be larger than 1 (e.g. for sucrose). For salts, electrostatic effects cause φ to be smaller than 1 even if 100% dissociation occurs (see Debye-Hückel equation);
n is the number of particles (e.g. ions) into which a molecule dissociates. For example: glucose has n of 1, while NaCl has n of 2; C is the molar concentration of the solute; the index i represents the identity of a particular solute. |
|
|
Which formula should you use to determine how much a cell will shrink/grow when placed into a bath?
|
Ci/Cf = Vf/Vi
derived from Mi = Mf and M = CV M = amount of solute C concentration V volume |
|
|
What is the difference between tonicity and osmolarity
|
tonicity depends on solute permeabilites and what the cell eventually does, osmorality depends on current concentrations
|
|
|
isotonic saline is used to..
|
boost extracellular volume without effecting intracellular volume (because Na/Cl has very low permabilities)
|
|
|
D5W IV is used to
|
boost both extracellular and intracellular volumes (because is both isomotic and hypotonic)
|
|
|
hypertonic solution causes the cell
|
to shrink
|
|
|
hypotonic solution causes..
|
the cell to swell
|
|
|
Tonicity depends on ...
|
which side has the greater amount of impermeant solutes
|
|
|
What are the three modes of permeable solute exchange across a membrane
|
1) non-electrolyte equalizes concentration
2) a negative and positive ion moving in the same direction simultaneously 3) a 1-for-1 exchange of a cation (or anion) |
|
|
radius of hydration is...
|
the radius of the ion with the water molecules surrounding it
|
|
|
What is the Nerst Equation
|
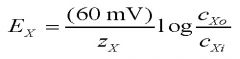
Calculates the equilibrium potential for a single species of ion
z_x: valence of the ion c_x0: concentration of teh ion ouside c_xi: concentration of the ion inside |
|
|
extracellular fluid contains ____(ions) and intracellular contains ___(ions)
|
K inside, Na/Cl outside
|
|
|
The only ion that has significant changes in concentration when crossing the membrane
|
Ca++ because most cells already have a very LOW [Ca++]
|
|
|
Typical equilibrium potentials for K, Na, Cl?
|
E_K = -100, E_Na = +50, E_Cl = -70 mV
|
|
|
What is the equation for the resting membrane potential.
|
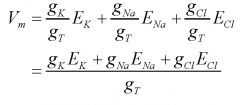
resting membrane potential is the weighted average of the individual equilibrium potentials
|
|
|
How can you calculate the flux of charges entering/exiting a cell membrane from the current
|
divide current by columb's constant e = 1.602X10^-19
|
|
|
How do you determine the moles of a ion from the charge
|
divide the charge by faraday's constant 965000 coul/mol
|
|
|
What is the sign convention of the flow of ions across the membrane
|
inward flow of positive -> neg
outward flow of + -> positive inward flow of - --> pos outward flow of + --> neg This is from the definition of real current (not conventional): negative charges (positive current) flows toward the lower potential, so if neg charges flow out of the cell this is positive current |
|
|
hyperkalemia is...
|
high extracellular levels of K+ that prevent the normal efflux pressure of K+ from its concentration gradient, which in turn depolarizes the cell just enough to keep the sodium inactivation gates closed and brings the cell closer to depolarization, the membrane potential becomes depolarized so more cl- enters the cell and the cell continually fires and can lead to cell death
|
|
|
_______ channels are even open at rest
|
K+ channels
|
|
|
Na+ channels have ___ gate(s) and is (are named)... K+ have...
|
Na+ has 2 gates m(activation) on the extracellular side and h(inactivation) on the intercellular side, K+ has one n (activaiton) gate
|
|

When are the h m gates open for the sodium channel
|
m gate is closed at resting potenatil, h gate is closed during repolarizing phase, and both are closed during undershoot
|
|
|
Why is there a resting potential at all
|
1) the Na/K pump creates a concentration gradient, 2) K+ leaks out of the cell more than Na+ leaks in (through leak channels and more open K+ channels)
|
|
|
what does adding ouabain do to an action potential
|
it selectively inhibits the na/K pump (but DOES NOT abolish action potential)
has no immediate effect on nerve AP, over time there is an effect |
|
|
Tetraethylammonium anion (TEA)...
|
*bocks K+ channels
* does not prevent APs because Na channels still work *abolishes hyperpolarization * prolongs duration of the AP |
|
|
Tetodotoxin (TTX)
|
* blocks Na channes irreversibly and blocks AP's altogether
*attenuates spike or blocks AP altogether *coms from puffer fish (Fugu) |
|
|
novocaine, lidocaine
|
* blocks Na channels reversibly
* locally blocks conduction in nerve(s) * returns when is diluted into extracellular volume and is metabolized or excreted |
|
|
How many mph in a m/s (also: How many pounds in a kilogram)
|
2.2
|
|
|
as r_internal/r_membrane/diameter increases conduction velocity...
|
r_internal: decreases
r_membrane: increases diameter: increases |
|
|
nerve conduction towards the nerve terminal is called...
|
orthodromic
|
|
|
nerve conduction towards the soma is called
|
antidromic
|
|
|
for unmyelinated axons conduction velocity goes as _____ and for mylenated fibers it goes ____
|
square root of the diameter, linerally
|
|
|
log 1
|
0
|
|
|
log 2
|
~0.3
|
|
|
log 3
|
~0.48
|
|
|
log 4
|
~0.6
|
|
|
log 5
|
~0.70
|
|
|
log 6
|
~0.78
|
|
|
log 7
|
~0.85
|
|
|
log 8
|
~0.90
|
|
|
log 9
|
~0.96
|
|
|
How does the membrane depend on ca++
|
the plasma membrane is compused of a negatively charged phosphatidyl serine which is "screend" by ca++. If ca++ is too low na+ will replace ca++, incrase E_na and the driving force of na+ into the cell, decrease the threshold potential and lead to hyperexcitability
|
|
|
Curare is..
|
a drug which blocks nicotinic Ach receptors.. causes completel paralysis because NMJ is blocked, used to induse paralysis during surgery
|
|
|
Atropine is
|
a drug which blocks muscarininc Ach receptors Used as an "antidote" for ach inhibiting agents
|
|
|
hemicholinium is..
|
a drug which blocks choline upake in presynaptic terminal. Ach in vesicle
|
|
|
How does black widow spider venom affect the synapse
|
uncouples ca++ dependent synaptic release. results in incontrollable release of all transmitter at a synapse
|
|
|
how does botulinium toxin affect the synapse
|
irreversibly blocks synaptic release of vesicles at cholinergic synapes including the NMJ
|
|
|
Cholinesterase inhibitors do what to the synaptic terminal..
|
block hydrolysis of ach at cholinergic synapes.. cause hugh-amplitude EPSPs with long duration, paralyzing muscle.. used as a treatment for myasthenia gravis.. allows ach to stay in the cleft longer so their fewer nAChRs can give a biggers respons to the Ach they have
|
|
|
the muscle "thin filament" is composed of...
|
actin (G-actin monomers which form an F-actin polymer) associated with tropomyosin which covers the binding sites bound to actin with troponin
|
|
|
troponin consists of ...(the three subunits)
|
TnT subunit that binds tropomyosin
TnC subunit that binds Ca++ TnI that links the three subunits together |
|
|
Describe the sliding filament theory "cross bridge cycle"
|

|
|
|
Explain rigor mortis at the molecular muscle level...
|
myosin must bind ATP to disassociate from actin.. without ATP muscles will be stiff
|
|
|
Describe how Ca++ enters the cytoplasm of the myofibril
|

The T-tubules carry action potentials from the motor end plate deep into SR, opening the SR’s
Ca++ releasing channel. This is done through the actions of the dihydropyridine (DHP) receptor. When the DHP conformation changes due to the AP, it “unplugs” the ryanodine receptor (aka calcium channel) of the SR, thereby releasing Ca++ necessary to initiate contraction |
|
|
General Somatic Efferent (GSE) is a ____ neuron system involving _____, General Visceral Efferent (GVE) is a ____ neuron system involving ______
|
GSE- a 1-neuron system involving alpha- and gamma-motoneurons
GVE- a 2-neuron system associated with the autonomic system, which can be classified as either sympathetic or parasympathetic |
|
|
I bands are called "I" because? and are ____ colored
|
isotropic because it reflects polarized light "I" for L*I*ght
|
|
|
Abands are called "A" because? and are ____ colored
|
anisotropic because it doesn't reflect polarized light "A" for dArk
|
|
|
Describe the relation among.. fibre, muscle, myofibril, filaments
|
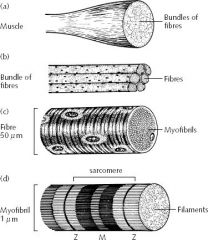
|
|
|
What are the three stages of an isometric twitch and how would you measure the time it takes to generate enough force
|
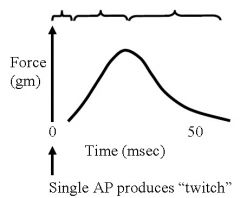
1)Latency period (time for AP to propagate, t-tubles, activate receptors, ca rlease from SR)
2Contraction time 3)Relaxation time Think F = ma --> no acceleration unless you can overcome the weight of an object, so the time for an object to move is latency + contraction time up to necessary force |
|
|
Given the filament lengths thin: 2.1 um, thick 1.5 um, bare zone 0.2 um make a rough plot of force v.s. sarcomere length
|
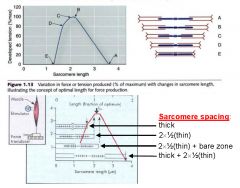
|
|
|
connexon is...
|
a hexameric protein that forms a gap junction
|
|
|
Second messengers bind to which protein to induce fusing of vesicles in the presynaptic terminal
|
synaptotagmin
|
|
|
hypocalcemia results in...
|
decreased neurotransmission
|
|
|
hypermagnesemia results in..
|
decrease3d neurotransmission because Mg competes with Ca++ influx
|
|
|
how is ca++ removed presynaptically?
|
ca++ atpase and sodium/calcium exchanger
|
|
|
The three muscle fiber types are:
|
slow oxidative (type I) - don't fatigue
fast oxidative (type IIa) - intermediate characteristics Fast glycolitic (type IIx) - most powerful, white in appearance, b/c no myoglobin for oxygen binding, fatigue easily |
|
|
invaginated villi are called
|
canaliculus
|
|
|
LIS is...
|
lateral intercellular space... space between epithealial cells
|
|
|
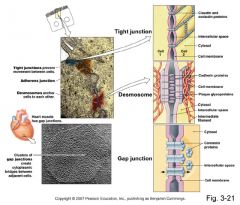
What are the major types of cellular junctions
|
|
|
|
K+ selective leak channels are blocked by... Na/K atpase are blocked by...Na leak channels are blocked by ...
|
barium/ouabain/TTX and amiloride
|
|
|
describe what happens to the fluid in the loop of Henle
|
In other words, as fluids go down the loop of henle, the extracellular solute concentrations pull H2O out to make it hypertonic. Then, when ascending, NaCl is given the chance to leave and is pulled out progressively by decreasing concentrations of solute in the extracellular matrix. This helps to create the gradient that pulled the H2O out in the first place.
|
|
|
how does cholera cause diarrhea..
|
affects the Cl- secretory cells: cholera toxin binds to cell membrane receptor activates adenylate cyclase which creates sustained increase of cAMP and secretion
|
|
|
WHO-ORS is?
|
world health organization oral rehydration solution: 90mM na+, 20 mM K+ 80mM Cl-, 20mM citrate 111mM glucose.. WORKS BECAUSE OF GLUCOSE (glucose/Na COtransporter)
|
|
|
preganglionic parasympathetic fibers release ____ onto the postganglionic cell which acivates _____ receptors
|
ach/nicotinic
|
|
|
postaganglionic parasympathetic release ____ to ____ receptors
|
ach/muscarinic
|
|
|
pregangalonic sympathetic fiber release ___ onto ____ receptors
|
ach/nicotinic
|
|
|
postganglionic cell releases _____ and activates ____ receptors
|
noreepinephrine/alpha- beta- receptors
|
|
|
pre-g sympathetics go to adreneal medulla where they synapse onto ____ via ___ ___ receptors
|
chromaffin cells/cholinergic nicotinic recptors
|
|
|
dopamine is degraded by
|
Monoamine oxidase, AKA MAO
|
|
|
the affect of MAO inhibitors is
|
to raise dopamine levels and produce a sympathetic effect
|
|
|
what does reserpine do...
|
reduces norepinephrine release... controls hypertension by controlling the amount of norepinephrine in the vesicle and therefore its release into the cell-> decrease in sympathetics, hence, decrease in blood pressure
|
|
|
What are the two methods of uptake of norepinephrine..
|
uptake 1: NR goes back into the presynaptic cell
uptake 2: NR going into another cell (the effector cell) NOT important unless uptake 1 is blocked, and uptake 2 is slow |
|
|
what enzyme degrades norepinphrine
|
Catecholo-methyltransferase (COMT)
|
|
|
alpha adrenergic receptors make mucles ____ alpha 1 are usually work on _____ terminal, alpha 2 usually work on ____ terminal
|
contract, presynaptic (though there are alpha 2 postsnyaptically) , postsynaptic
|
|
|
compare epinephrine, norepinephrine, isoproterenol as alpha agonist/antagonists
|
epinephrine > norepinephrine >>isoproterenol (stimulates beta) as alpha agonist
|
|
|
Beta-1 receptors reside _____ wherease Beta-2 reside _____
Beta-1 are stimulated by _____ Beta-2 are stimulated by ____ |
in the heart, everywhere else, norepinephrine/epinephrine, epinephrine (NR doesn't affect Beta-2)
|
|
|
isoproterenol is a _____ agonist/antagonist.. propranolol is a...
|
non-specific agonist, non-specific beta antagonist
|
|
|
What is the path of the heart's conducting system:
|
SA notde->atria->AV node->ventricular conducting sytem (bundle of His and peripheral Purkinje fibers)->inside heart->outside of heart->apex of heart->base of heart
|
|
|
A gap junction is formed by __(#)__ _____ which is composed of _(#)_ ____
|
A gap junction is formed by 2 connexons (also called hemichannels) which is composed 6 connexins
|
|
|
In addition to Na+ current in cardiac muscle there is...
|
and L type Ca current that activates at potential positive to about -40mV and provides an net inward current
|
|
|
describe calcium induced calcium release in the heart
|
1. ca ions come along through the inward L-type Ca current
2. Ca inos flow into the cell and bind to receptors on the SR 3. The binding of Ca on the SR opens Ca channels on the SR that rlease Ca into the cytosol 4. Large incrase in cytosolic Ca leads to muscle contraction |
|
|
why can't you tetanize the heart
|
the action potential is effectively just a long as the contraction.. to tetanize the AP must be shorter than the contraction time
|
|
|
How is Ca from L-type channel pumped out fo the cell
|
*Na/Ca low-affinity, high-capacity exchanger removes MOST of ca that comes in
* Ca ATP pump - balances small deviations of Ca from resting levels |
|
|
describe therapeutic na/k pump blocking
|
1. drugs block 10% of Na/K pumps
2. na rises in the cell 3. na gradient decreases 4. na/ca pump decreases 5. ca rises in the cell 6. more ca pumped into sr 6. more ca releases from sr during subsequent ap's 8 greater strength of contraction |
|
|
which autonomic nerves control the heart
|
Parasympathetic input from vagus
Sympathetic input from thoracic sympathetic efferents from ganglion on esophagus |
|
|
myocytes have which type of receptors
|
beta receptors for sympathetic input
cholinergic M2 receptors for vegal, muscharinic parasympathetic input |

