![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
8 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
A. Describe regulation of the heart? and define:
1. chronotropic 2. inotropic 3. dromotropic B. Describe the effect of parasympathetic innervation to the heart by using the terms above? C. Describe the effect of sympathetic innervation to the heart by using the terms above? |
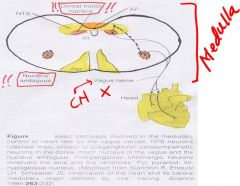
A. Cardiac centers in the medulla and pons influence heart activity via sympathetic and parasympathetic nerves
Regulation of: 1. Heart rate (beat)= chronotropic action 2. Systolic contractile force: inotropic action 3. Atrioventricular conduction velocity: dromotropic action B. Parasympathetic innervation: -vagus (CN 10) sends preganglionic fibers from the right side to right atrium - mainly SA node, and from Left vagus to AV node. -stimulation of right vagus or ACh application decreases heart rate (negative chronotropy) -stimulation of left vagus retards atrioventricular conduction and in extreme cases an AV block occurs (negative dromotropic action) -vagus may reduce strength of contraction of myocardium (negative inotropic action) C. Arises from the preganglionic fibers in the upper thoracic cord -Sympathetic stimulation or norepinephrine application increases heart rate,(positive chronotropic action) force of atrial and ventricular myocardial contraction - Sympathetic inhibition or removal results in decreased tone of heart. |
LoVe
|
|
|
Describe regulation of circulation?
|
-ANS regulation of vasomotor tone is via sympathetic fibers with few exceptions
such as vessels of the external genitalia and small pial arteries. -Both epinephrine and norepinephrine are continuously released in small amounts into the blood by the adrenal medulla. |
|
|
|
Describe cardiovascular regulation?
|

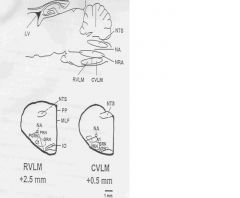
Cardiovascular regulation is monitored by strategically placed receptors throughout the body, which send afferent impulses centrally to the vasomotor center (VMC) located in the medulla oblongata. The ventrolateral medulla (VLM) is involved in the regulation of cardiovascular activity. VLM neurons are involved in the maintenance of blood pressure, vasomotor tone, baroreceptor, chemoreceptor, and cardiorespiratory reflex mechanisms.
The VLM may be subdivided into two functional regions: 1. Rostral Ventrolateral Medulla (RVLM) Which comprises the: -C-1 Area [Adrenergic; Epi]. -RVLM nervous system contain phenyl ethanolamine – N methyltransferase (PNMT), a cytoplasmic enzyme that catalyzes the conversion of NE to EPI. -The excitatory transmitter is however GLUTAMATE. 2. Caudal Ventrolateral Medulla (CVLM) -A-1 Area [Adrenergic; -Nor-Epi] (Best Known) NOTES: -RVLM and CVLM are the “VASOMOTOR CENTER”. -Stimulation of the RVLM elicits a pressor response, e.g., increase in heart rate and sympathetic activity. Thus the RVLM may be referred to as the “PRESSOR AREA”. -Stimulation of the CVLM neurons elicits a decrease in blood pressure, decreased sympathetic activity and bradycardia. This area is referred to as the “DEPRESSOR AREA”. |
|
|
|
Describe the nucleus tractus solitarus (NTS) and relate it to other organs in the medulla?
|
Your decreased oxygen deals with lactic acid and hydrogen ion being produced
Intermittent hypoxia Low O2 is a peripheral chemoreceptor event The receptor for respiration are in the medulla oblongata The dorsal group is your nucleus tractus solitarus!!!!!! The ventral respiratory group is your nucleus ambiguus and nucleus retro ambigualiis!!! NTS is a respiratory center and your chemoreceptor structures are not the respiratory centers, the The chemistry of the blood..Ph and the CSF..PH, O2 of the blood, and CSF, and then C02 of the blood CSF is infuenced by the chemistry of the blood This determines what activates the receptors |
|
|
|
Illustrate the carotid sinus reflex and differentiate btw:
-Carotid sinus -Carotid body |

1. Carotid sinus = a slight dilation of the common carotid artery at the bifurcation. It contains baroreceptors which, when stimulated, cause bradycardia and a decrease in blood pressure.
2. Carotid body : is a small structure located just above the bifurcation of the common carotod artery; it contains chemoreceptors that respond to carbon dioxide, oxygen, and pH levels CAROTID SINUS REFLEX Baroreceptors are located in the walls of the heart and blood vessels. The carotid sinus and aortic baroreceptors are stretch receptors. A brief overview of the carotid sinus baroreceptors is described. The carotid sinus is located at the bifurcation of the common carotid arteries. They are small swellings which contain mechanoreceptors or stretch receptors. Innervation is via the carotid sinus nerve, abranch of the glossopharyngeal (Nerve IX). Another pressoreceptor is located in the arch of the aorta and is innervated by vagal afferents. When the vessel wall is stretched by maintained pressure these receptors respond by increasing their impulse discharge rate. Afferent impulses from these receptors are conducted to the cardioinhibitory and vasomotor centers in the medulla oblongata, where they cause inhibition of sympathetic activity and excitation of parasympathetic activity. As a result vasomotor tone is reduced while heart rate and myocardial contractile force are decreased. This feedback mechanism operates to stabilize blood pressure and heart rate. A drop in systemic arterial blood pressure results in a rise in blood pressure and cardiac output. Thus external pressure applied to the neck such that carotid sinus pressure is augmented produces bradycardia and a drop in blood pressure. In older people who have developed arteriosclerosis, the blood pressure may fall drastically with transient cardiac arrest and loss of consciousness (carotid sinus syndrome). |
|
|
|
1. Describe GASTROINTESTINAL REFLEXES?
2. Describe MICTURITION REFLEX? |
1. The gastrointestinal (GI) tract has an intrinsic nervous system throughout its extent which controls both gastrointestinal motility and secretion. This system is composed of an outer myenteric or Auerbach’s plexus and an inner submucosal or Meissner’s plexus. Auerbach’s plexus controls mainly GI motility while Meissner’s plexus controls mainly secretion and some sensory functions. In general, stimulation of the myenteric (Auerbach’s) plexus increases GI motility by increasing tonic contraction and rate of rhythmic contraction.
2. MICTURITION REFLEX The wall of the bladder is composed of 3 layers of smooth muscle. This smooth outermost muscle is called the detrusor muscle and is responsible for bladder emptying. Bladder contractions may be recorded on the cystometrogram as stretch of the detrusor begins to occur. The greater the stretch the greater the activity of the stretch receptors within the bladder walls. Regulation of micturition is a reflex process but it is subject to modulation by higher centers in the brainstem and cerebral cortex Higher center modulation is primarily inhibitory though some output are excitatory |
|
|
|
Describe the 3 mechanisms of cardiovascular regulation (CVS)?
|
1. a. Posterior and lateral hypothalamic stimulation causes blood pressure and heart rate increase. Stimulation of this region evokes increased catecholamine secretion from the adrenal medulla.
2. Stimulation of the Peoptic area in the anterior hypothalamus causes a decrease in blood pressure and heart rate. 3. c. Sympathetic Cholinergic Vasodilation System. Sympathetic nerves to skeletal muscles include vasodilator fibers which release acetylcholine at their endings which at on the smooth muscles of the blood vessels. This system is controlled by the anterior hypothalamus. It is believed that at the onset of exercise, the sympathetic vasodilator system causes the initial vasodilation in skeletal muscles associated with anticipatory increase in blood flow, thus, providing the necessary oxygen. NOTES The impulses get to the vasomotor center, means connection by vasomotor fibers that go to the blood vessels intermediolateral horn, then to yiu SYMPATHETHIC CHOLINERGIC OUTFLOW SYSTEM!!! |
|
|
|
Describe TEMPERATURE REGULATION?
|

ADDITIONAL NOTES
1. Anterior Hypothalamus – Thermostatic Regulator a. Increased temperature of blood flowing through the anterior hypothalamus increases its activity. Decreased temperature depresses its activity. Increased activity of anterior hypothalamus triggers heat loss mechanisms. i. By stimulation of sweat glands ii. By inhibition of sympathetic activity in posterior hypothalamus. (There is then dilation of blood vessels to the skin and heat loss). HEAT CONSERVATION MECHANISM 1. Abolition of Sweating – evaporate cooling ceases 2. Vasoconstriction of skin blood vessels 3. Pilorection of skin blood vessels HEAT PRODUCTION – also may be necessary, if the hypothalamic thermostatic temperature remains below 37°C. This may be accomplished. 1. Shivering. The dorsomedical portion of the posterior hypothalamus contains an area called the primary motor center for shivering. There is a general increase in muscle tone resulting in increased metabolism; thus, increased heat production. 2. Sympathetic excitation may occur with increases in circulating norepinephrine and epinephrine in the blood causing increase in the rate of cellular metabolism. 3. Increased thyroxine output may occur due to the increased production of thyrotropin releasing factor by the hypothalamus. Thyrotropin releasing factor is carried by the blood via the hypothalamic portal veins to the adenohypohysis where it stimulates secretion of thyrotropin. |
|

