![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
39 Cards in this Set
- Front
- Back
|
functions of colon 3
|
Storage, concentration of undigested material
Electrolyte & water transport Propulsion of content |
|
|
regulation of reflexes of GI tract mechanism 3
|
1. Neural regulation
a. Short neural reflex b. Long neural reflex 2. Chemical regulation Endocrine Paracrine |
|
|
difference between the short and long neural reflexes 2
|
1. Short reflexes (from GI receptors through enteric nerve plexuses to effector cells)
2. Long reflexes (from GI receptors to CNS by afferent nerves & back to enteric nerve plexuses and effector cells by way of ANS) (Parasympathetic: excitatory; Sympathetic: inhibitory) |
|
|
list the major GI hormones and paracrines 5+2
|
Major GI hormones - Gastrin, cholecytokinin, secretin, GIP, motilin
Paracrines - Histamine, Somatostatin |
|
|
what is the function of D cell and G cell and ECL cell
|
enterochromaffin-like (ECL) cells – histamine
D-Cells – somatostatin G-cells – gastrin |
|
|
gastric juice components
|
NaCl KCl and HCl
|
|
|
mechanism of HCl secretion 2+2
|
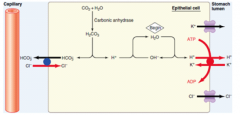
breakdown of water to form H+ and excrete to lumen by H+/K+ antitransport (requice ATP).
there is K+ pump outflux for replacing K+ bicarbonate is produced and excrete into Blood via bicarbonate/Cl- antitransport CFTR Cl - channel: Cl - outflux for recycling CFTR = Cystic fibrosis transmembrane conductance regulator |
|
|
regulation of HCl secretion
|
1. gastrin - by G cell (hormonal)
functions: promote ECL cells secretion (no. and size) and act on the CCK-beta receptor to activate increase Ca level 2. ECL cell secrete histamine (paracrine)- histamine act one he H2 receptor to activate adenylate cyclase to form cAMP 3. neural control: Ach act on muscarinic receptor => IP3 to increase Ca level; also increase gastrin and histamine 4. somatostatin : inhibition of HCl secretion |
|
|
stimulation and inhibition of HCl secretion three phases and their specific action 3+3
|
1. cephalic phase (chewing, sight) promote the Ach released by vagus nerve
2. gastric phase 2.1 distension of stomach - vasovagal reflex 2.2 proteins product in stomach - gastrin secretion 3. intestinal phase - distension, acidity, nutrients conc. => inhibition by decrease secretin and release somatostatin. distension of duodenum =>vagovagal reflex Enterogastrone (CCK and secretin) - secreted by intestines. |
|
|
regulation of secretion of pepsinogen (from chief cell)
|
simulation:
neural: ACh from vagus & enteric nerve plexuses; high acidity: acid in stomach through local nerve reflex inhibition excess acidity (ph <3) => increase somatostatin => decease acid & gastrin secretion |
|
|
mucous and bicarbonate functions and production sites 2
|
produced in mucous neck cell and columnar epithelial cells -
a physical and alkaline barrier to protect against pepsin and acid. almost neutral at the base |
|
|
drugs/factors that inhibit mucous and bicarbonate secretion 2
|
adrenergic agonist => decrease carbonate
NSAID => decrease bicarbonate and mucus secretion predispose to ulcer and gastritis |
|
|
intrinsic factor production site and functions
|
produced in parietal cells - intrinsic factor is important for the absorption of vit B12.
|
|
|
consequence of insufficient / no Vit B12
|
1. megaloblastic anemia - inhibit DNA syn, growth of cell without cell division
2. pernicious anemia - due to autoimmune destruction of parietal cells => no intrinsic factor => NO RBC maturation |
|
|
carbohydrate digestion
different sites, their enzymes, and reaction involved 4 sites, |
mouth cavity:
salivary amylase: starch → α-dextrins endoglucosidase, cleave α-1,4 glycosidic bonds optimal pH ~ 6-7.9, maintained by bicarbonate ion in saliva Duodenum pancreatic amylase starch, α-dextrins → disaccharide DO NOT cleave α-1,6 glycosidic bonds Small Intestinal brush border maltase, isomaltase, lactase, sucrase Fermentation in colon when high amylase, less well hydragrated dietary fibres and undigested sugars fermentation by colonic bacteria: saccharides → gases, FA, lactate |
|
|
pathology of carbohydrate digestion 3
and clinical presentation 3 |
primary deficiency of carbohydrase
- low synthesis rates / mutated genes → deficiency secondary to malabsorption - accumulation of undigested saccharide in large bowl secondary to intestinal injury - brush border epithelium damage clinical presentation 1. copious flatus and hyperactive bowel sounds (gas) 2. explosive diarrhea (partially digested saccharides, retain of water, osmotic effect => water retention 3. abdomen distention and cramps (water and gas) |
|
|
protein digestion sites and reactions
three phrases |
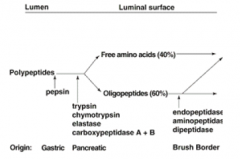
gastric
pepsin secretion excite CCK and secretin => intestinal and pancreatic secretion of trypsin and inhibit HCl production protein → polypeptides pancreatic enteropeptidase: trypsinogen → trypsin - chymotrypsinogen → chymotrypsin - proelastase → elastase - procarboxypeptidase → carboxypeptidase small intestinal brush border - aminopeptidases - intracellular peptidases (Dipeptidase, Tripeptidase, endopeptidase) - peptides → a.a. |
|
|
Pancreatitis pathology 2pts
|
inflam. of the pancreas due to activation of pancreatic enzymes (esp. trypsin)
within the pancreas → autodigestion - usually involve malfunction in genes coding for trypsin inhibitor / regulator (eg. SPINK1, CTRC) |
|
|
lipid digestion phrases and reactions involve
|
1. lingual and gastric lipase for short chain FA
2. Duodenum 2.1 bile salts - emulsification 2.2 pancreatic lipase: TG/DG → FA + 2-MG inhibited by bile salts colipase: bind FA and lipase tgt; overcome the bile salts 2.3 lipid esterase: vit A esterase, chol. esterase (need bile salts) 2.4 phospholipase A2 (need bile salts) |
|
|
Regulation of pancreatic exocrine secretion 3
|
1. Cephalic phase (minor)
sight, smell, taste, chewing of food → ACh release by vagus nerve 2. Gastric phase (negligible) - nervous stimulation 3. Intestinal phase (major) (hormonal and neural) 3.1 acid chyme → S-cells → secretin secretion of large amount of water & bicarbonate 3.2 partially digested protein & fat → I-cells → CCK secretion of pancreatic enzymes 3.3 CCK also stimulates the contraction of gallbladder relaxation of sphincter of Oddi 3.4 vagus nerve - ACh as neurotransmitter to promote acinar cells secretion |
|
|
content of bile 6
|
water + electrolytes + organic compounds (bile acids, chol, phospholipids, bilirubin)
|
|
|
synthesis of bile salt 4
|
1. syn. by hepatocytes from chol.
2. primary bile acid (major): cholic acid, chenodeoxycholic acid 3. secondary bile acid (intestinal bacteria): deoxycholic acid, lithocholic acid conjugated bile acid (=bile salt): glycine & taurine – conjugation of 1° & 2° bile acids |
|
|
secretion of bile salts 4
|
First stage: Hepatocytes secrete fluid rich in bile salts, chol and other organic
compounds → canaliculi → bile duct Second stage: Ductal epithelial cells add water and bicarbonate (← secretin) Storage & conc: Bile enters gall bladder between meals → concentrated by reabsorption of water & electrolytes Release: During meals → CCK → gall bladder contracts and release bile (CCK under neural and hormonal control) |
|
|
digestive Functions of biliary secretion 3
another biliary secretion function 1 |
bile acid: aid fat digestion & absorption, promote absorption of fat-soluble Vit
bicarbonate: neutralizes acid chyme excretory function (bile pigments, excess chol, drugs) |
|
|
movement of food during swallowing (3 phrases)
|
1. Oral phase: Voluntary transfer of food or drink to pharynx by tongue
2. Pharyngeal Phase: Elevation of soft palate to prevent food from entering nasal cavity; larynx raised; glottis closed; respiration inhibited; Epiglottis cover glottis to prevent food from entering trachea (aspiration) 3. Esophageal phase: relaxation of upper esophageal sphincter; closure of sphincter after passage of food; glottis opens; breathing resumes; peristaltic waves move food down esophagus towards stomach; relaxation of lower esophageal sphincter; receptive relaxation of stomach; then closure of lower esophageal sphincter. |
|
|
movement of food through esophagus
|
from higher intraluminal pressure to lower pressure
|
|
|
swallowing reflex
|
afferent and efferent nerve supply
control swallowing center |
|
|
assistance in movement of food through esophagus 4
|
primary peristaltic contractions
secondary peristaltic contractions Upper sphincter lower sphincter |
|
|
causes of dysphagia 4
|
1. Painful disease of mouth & pharynx
e.g. Stomatitis, ulcers 2. Paralysis of mechanisms of swallowing (Neural causes e.g. damage of swallowing centre e.g. poliomyelities; damage in nerves involved in swallowing; Neuromuscular transmission e.g. myasthenia gravis; Muscular e.g. muscle dystrophy; Motility e.g. achalasia) 3. External compression on esophagus e.g. goitre, enlarged lymph nodes 4. Intrinsic disease of esophagus e.g. stricture, cancer of esophagus |
|
|
Motor Functions of Stomach 3 functions in fed state
|
1. storage of food - receptive relaxation
mediated by vagovagal reflex and coordinated by swallowing centre 2. mixing and grinding contractions mix ingested food with gastric juice, digestion and solubilize food substances, reduce particle size 3. controlled emptying: optimal time for intestinal digestion and absorption |
|
|
mixing two types
|
slow waves:
regular depolarization => 3-5 waves per minute => weak contraction => weak mixing effect contraction in natrum: retropulsion => propel the chyme back break down and mix food |
|
|
coordination / control of gastric emptying
reason structure mechanism control |
structure: phyloric sphincter
emptying process: antral peristaltic contraction Regulation by both neural & hormonal: - weak gastric factors promote emptying (stretch teh wall) - duodenal factors inhibit emptying (distension of duodenum & presence of hypertonic solutions, low pH, fatty acids or monoglycerides in the duodenum) - hormonal factors include: secretin, CCK, GIP, gastrin reason? Rate of gastric emptying is regulated to ensure that gastric contents are not emptied into the duodenum at a rate faster than the small intestine can neutralize gastric acid and process the chyme |
|
|
function of stomach in fasted state
|
hunger contractions to increase drive to acquire food
MMC migrating myoelectric complex) => clear of any debris |
|
|
vomiting reflex neural pathway 4
|
Emetic stimuli
Afferent pathway:vagal and sympathetic chemoreceptor trigger zone: flood of 4th ventricle near area postrema (no blood brain barrier here, triggering drugs: morphine and apomorphine esp after general anesthesia) Vomiting centre in medulla, near tractus solitarius at level of dorsal motor nucleus of the vagus nerve Efferent pathway: V, VII, IX, X, XII to upper GIT and spinal nerve to diaphragm and abdominal mus |
|
|
what are the stimuli for vomiting 5
|
-irritation of GI mucosa
-tactile stimuli (gag reflex) CNX -activation of chemoreceptor @ postrema which is outside BBB, sensitive to toxin - rotating movement of head (motion sickness) by vestibular system (CN VIII vestibulocochlear nerve) - high brain centers: psychiatric disorders and stress |
|
|
complications of vomiting 4
|
dehydration
electrolyte imbalance - hypochloremic metabolic alkalosis & hypokalemia acid base imbalance aspiration and pneumonia |
|
|
two mixing of small intestine
|
1. peristaltic contractions
progressive contractions of curcularr smoooth muscle => long transit time 2. Mixing (segmentation) contractions by slow depolarization, back and forth, help mix te content (reflex: gastroileal reflex, intestino-intestinal reflex) |
|
|
motility of large intestine (control)
|
inactive in most of the time
segmentation contraction of circular mus, longitudinal mus strips => form haustrations mass movement (perisatltic wave) Distension of rectum => rectosphincter reflex initiation of mass movement: gastrocolic & duodenal reflex |
|
|
Dysphagia
causes 4 x 2 |
Painful disease of mouth & pharynx
Paralysis of swallowing mechanisms External compression on esophagus Intrinsic disease of esophagus |

