![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
55 Cards in this Set
- Front
- Back
|
What is the function of acetylcholinesterase?
|
The enzyme acetylcholinesterase converts acetylcholine into the inactive metabolites choline and acetate. This enzyme is abundant in the synaptic cleft, and its role in rapidly clearing free acetylcholine from the synapse is essential for proper muscle function.
|
|
|
EPSPs are graded, what does that mean?
|
They have an additive effect. When multiple EPSPs occur on a single patch of postsynaptic membrane, their combined effect is the sum of the individual EPSPs. Larger EPSPs result in greater membrane depolarization and thus increase the likelihood that the postsynaptic cell reaches the threshold for firing an action potential.
|
|
|
Describe electrical synapse.
|
An electrical synapse is a mechanical and electrically conductive link between two abutting neurons that is formed at a narrow gap between the pre- and postsynaptic neurons known as a gap junction.Compared to chemical synapses, electrical synapses conduct nerve impulses faster, but unlike chemical synapses they do not have gain (the signal in the postsynaptic neuron is the same or smaller than that of the originating neuron).
|
|
|
What is a connexon?
|
In biology, a connexon is an assembly of six proteins called connexins that can be a part of a gap junction channel between the cytoplasm of two adjacent cells. They can be opened or closed, which is regulated by intracellular signalling (phosphorylation).
|
|
|
What is a neurotransmitter?
|
Neurotransmitters are endogenous chemicals which transmit signals from a neuron to a target cell across a synapse.
|
|
|
What is an inhibitory postsynaptic potential (IPSP)?
|
IPSP is a graded hyperpolarisation that moves the membrane potential further from the threshold for firing an action potential.
|
|
|
What is the ionotropic transmembrane receptor for glutamate that mediates fast synaptic transmission in the central nervous system (CNS).
|
The ionotropic glutamate receptor (AMPA-type).
|
|
|
Name receptors for synaptic excitation and inhibition.
|
Synaptic excitation: the ionotropic Glutamate receptor.
Synaptic inhibition: GABAa receptor. |
|
|
Name which receptor is:
- the major central inhibitory receptor type; - is a ligand-gated ion channel composed of 5 subunits; - is permeable to Cl- and HCO3- ions. |
GABAa receptor.
|
|
|
Which receptor is:
-one of the most abundant central receptors; - is a ligand-gated ion channel composed of 4 subunits; - is permeable to Na, K, and sometimes Ca ions. |
Ionotropic glutamate receptor (AMPA-type).
|
|
|
IPSP and EPSP are unable to do what in comparison to AP?
|
To travel along the axons.
|
|
|
What do sensory receptors respond to?
|
Light, heat, mechanical, chemical, etc.
|
|
|
What type of neurones are sensory receptors?
|
Sensory receptors are either specialised endings of afferent neurons or separate cells that signal to the afferent neurone.
|
|
|
Sensory receptors are transducers. What does that mean?
|
Sensory receptors convert one form of energy (e.g. heat, pressure, chemical) into another form, e.g. electrical energy or depolarisation.
|
|
|
The depolarisation occurring at the sensory terminal is called ... .
|
Receptor potential (RP)
|
|
|
Is the depolarisation occurring at the sensory terminal propagating or non-propagating?
|
Non-propagated, it is confined to terminal, it is graded.
|
|
|
What relationship is there between the number of action potentials generated by a pressure-sensitive sensory afferent neurone and stimulus intensity?
|
Directly proportional.
|
|
|
What is the mechanisms that prevents sensory information overload?
|
Adaptation to stimuli of receptors.
|
|
|
There are slow adaptations to the stimuli and fast, and there are stimuli that receptors are not able to adapt to. What are they?
|
Pain receptors are nonadapting receptors.
|
|
|
What function do sensory receptors in internal organs have?
|
They are essential for homeostasis and also alert the body in case of some anomaly.
|
|
|
How is intensity of the stimulus encoded?
|
By the frequency of action potentials.
|
|
|
What is the name of information sent to the CNS from the sensory receptors?
|
Afferent information.
|
|
|
What is the reason for referred pain?
|
In the CNS it is usual that several afferent neurones contact the same postsynaptic cell. This is convergence.
|
|
Label the axis and fill in blanks about which channels close or open in a specific moment.
|
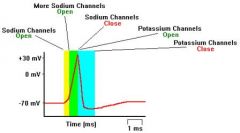
|
|

Label.
|
|
|
|
What is threshold stimulus?
|
The minimum stimulus needed to achieve an action potential is called the threshold stimulus. The threshold stimulus causes the membrane potential to become less negative (because a stimulus, no matter how small, causes a few sodium channels to open and allows some positively-charged sodium ions to diffuse in).
|
|
|
What is a propagation of the AP?
|
It is repeating of AP down the axon.
|
|
|
Name three types of neurone.
|
Multipolar, unipolar, bipolar.
|
|
|
What is multipolar neurone?
|
Multipolar neurons are so-named because they have many (multi-) processes that extend from the cell body: lots of dendrites plus a single axon. Functionally, these neurons are either motor (conducting impulses that will cause activity such as the contraction of muscles) or association (conducting impulses and permitting 'communication' between neurons within the central nervous system).
|
|
|
What is unipolar neurone?
|
Unipolar neurons have but one process from the cell body. However, that single, very short, process splits into longer processes (a dendrite plus an axon). Unipolar neurons are sensory neurons - conducting impulses into the central nervous system.
|
|
|
What is bipolar neurone?
|
Bipolar neurons have two processes - one axon & one dendrite. These neurons are also sensory. For example, biopolar neurons can be found in the retina of the eye.
|
|
|
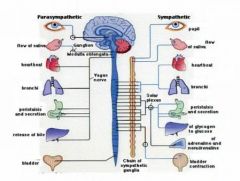
Name subdivisions of ANS - autonomic nervous system.
|
Sympathetic, parasympathetic, enteric.
|
|
|
What is the difference between preganglionic fibre lengths of sympathetic and parasympathetic NS?
|
In Sympathetic NS preganglionic fibres are shorter than in parasympathetic NS.
|
|
|
What are the major transmitters in the autonomic synapses?
|
Noradrenaline (NA) and acetylcholine (ACh).
|
|
|
In which part of the ANS neurotransmitter noradrenaline is used?
|
In the synapses of sympathetic NS between the postganglionic fibre and effector organ.
|
|
|
Describe alpha receptors.
|
Alpha receptors are located postsynaptically at sympathetic neuroeffector junctions of many organs. In general, alpha receptors mediate excitation or increased activity of the effector cells. Vascular smooth muscle is an important site of alpha receptors. SNS activity maintains vascular tone, and thus blood pressure, by maintaining a tone of neurotransmitter on vascular alpha receptors.
|
|
|
Describe beta receptors.
|
Beta receptors are also located postsynaptically at sympathetic neuroeffector junctions of many organs. In general, beta receptors mediate relaxation or decreased activity of the effector cells. Thus, blood vessels dilate and uterine smooth muscle relaxes in response to activation of beta receptors. Heart muscle is an important exception to this rule. Activation of beta adrenoceptors in heart increases the automaticity and contractility of all parts of the heart.
|
|
|
Describe adrenergic receptors (α and β).
|
The adrenergic receptors (or adrenoceptors) are a class of metabotropic G protein-coupled receptors that are targets of the catecholamines, especially noradrenaline (norepinephrine) and adrenaline (epinephrine). Many cells possess these receptors, and the binding of an agonist will generally cause a sympathetic (or sympathomimetic) response (e.g. the fight-or-flight response). For instance, the heart rate will increase and the pupils will dilate, energy will be mobilized, and blood flow diverted from other non-essential organs to skeletal muscle.
|
|
|
Shortly, what selected action
of agonist do alpha and beta receptors have? |
α - Smooth muscle contraction and neurotransmitter inhibition & Cardiac muscle relaxation;
β - Smooth muscle relaxation, Heart muscle contraction, Enhance lipolysis. |
|
|
Name some of the effects of SNS.
|
- Increase in heart rate, increase force of contraction;
- Pupil dilatation; - Glycogenolysis (release of glucose from the storage form) and gluconeogenesis (new glucose made) - Increase in blood glucose. |
|
|
When does the parasympathetic NS dominate?
|
During sleep and rest.
|
|
|
Name some of the effects of parasympathetic nervous system.
|
- Eye pupil constriction (accommodation for near objects);
- Motility of stomach and intestine increases; - Trachea and bronchi constriction; - Decrease in heart rate and force of contraction. |
|
|
How is sensory transduction mediated?
|
Through opening or closing specific ion channels.
|
|
|
What are nociceptors activated by?
|
By extremes of pressure, temperature, or noxious chemicals.
|
|
|
Name five types of sensory receptors.
|
Mechanoreceptors
Thermoreceptors Nociceptors Photoreceptors Chemoreceptors |
|
|
In sensory transduction what is called receptor potential?
|
It is the change in membrane potential, which increases or decreases the likelihood that action potentials will occur.
|
|
|
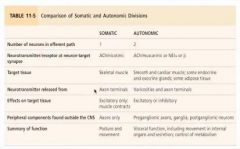
What is the number of neurons in the efferent part in somatic NS and autonomic NS?
|
Somatic - 1, autonomic - 2.
|
|
|
Name target tissues for somatic and autonomic NS?
|
Somatic - only skeletal muscle;
Autonomic - smooth and cardiac muscle, some endocrine and exocrine glands, some adipose tissue. |
|
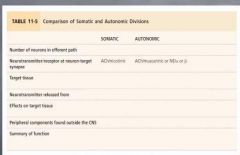
Fill in the table.
|
|
|

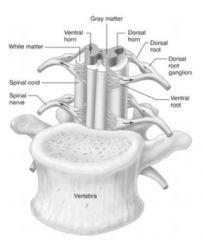
Label.
|

|
|
|
What is the number of neurons in the efferent part in somatic NS and autonomic NS?
|
Somatic - 1, autonomic - 2.
|
|
|
Name target tissues for somatic and autonomic NS?
|
Somatic - only skeletal muscle;
Autonomic - smooth and cardiac muscle, some endocrine and exocrine glands, some adipose tissue. |
|
Label.
|
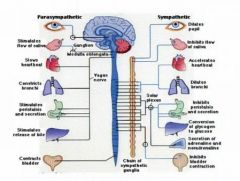
|
|
|
What is the purpose of Enteric NS?
|
Regulates work of the GI tract.
|
|
|
What do motor neurones of the ENS control?
|
- Contraction of the GI tract smooth muscle which push food through the GI tract;
- Secretion of the GI tract organs; - Activity of the GI tract endocrine cells, which secrete hormones. |

