![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
29 Cards in this Set
- Front
- Back
|
What two major things does [Na] regulate?
|
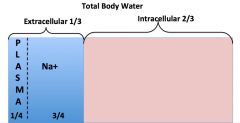
*Na+ is the major extracellular cation.
*Na+ determines extracellular volume and plasma volume. |
|
|
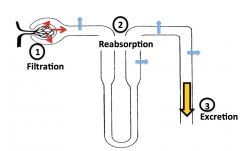
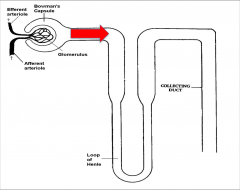
Simplified schematic of filtration, reabsorption, and excretion in the nephron:
|
|
|
|
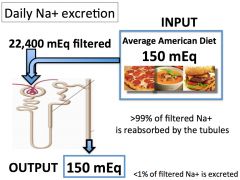
How much Na is filtered every day?
|
[Serum Na+] X Glomerular Filtration Rate =
140 mEq/L X 160 L/day = 22, 400 mEq/day |
|
|
How much Na gets excreted every day?
|
|
|
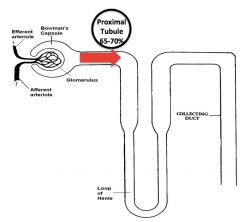
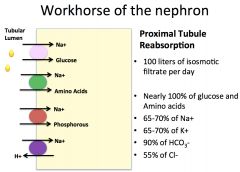
Discuss the actions of the proximal tubule:
Why is it so important? |
|
|
What's the Pathway of Reabsorption in the proximal tubule?
|
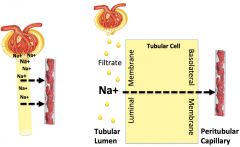
*Na goes from lumen to the peritubular capillary. It must cross two membranes to get there.
|
|
How is Na transported across the luminal and basolateral membranes?
|

*Concentration gradient enables it to come in passively on luminal side. It brings some other good stuff with it by co-transport. It also comes in via the H+/Na anti-porter.
*Na/K pump pumps it back out on the basolateral side. |
|

With all the Na+ coming into the proximal tubule cell, how is charge maintained?
|
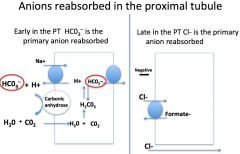
*It must stay electroneutral, so anions get reabsorbed, too.
*Early = Bicarbonate. Note the passive diffusion and rxns that allow this to occur. *Late = Chloride. |
|
With all the reabsorption happening in the proximal tubule, how is osmolality maintained?
|
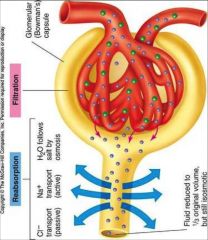
*Isosmotic filtrate is reabsorbed.
*As solute is removed from the tubular lumen, the osmolality in the lumen falls and water is reabsorbed. *Water follows sodium! |
|
Summary of actions that occur in the proximal tubule:
|
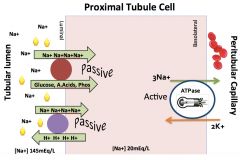
*65%-75% of Na is reclaimed here.
*Glucose, AAs, P by co-transport. *Na+/H+ by antiport. *Powered by 2° active transport: Na/K pump. *Reabsorption across luminal membrane down an electrochemical gradient. *Na/K pump in basolateral membrane returns reabsorbed Na to blood & provides energy. *Early in the PT BICARB is the primary anion reabsorbed. *Late in the PT Cl- is the primary anion reabsorbed. *H2O is reabsorbed along with Na; filtrate isosmotic to blood is reabsorbed. |
|
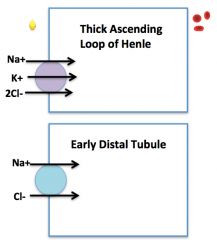
What actions occur in the Thick ascending loop of Henle?
|
![*Powered by 2° active transport (Na/K pump).
*Less Na is reabsorbed (20-30%).
*Along the [gradient], Na brings in K and 2Cl for every Na.
*Clinical correlation: This is where LOOP diuretics work, blocking the Na/K/Cl pump (furosemide/Lasix).](https://images.cram.com/images/upload-flashcards/67/10/06/2671006_m.jpg)
*Powered by 2° active transport (Na/K pump).
*Less Na is reabsorbed (20-30%). *Along the [gradient], Na brings in K and 2Cl for every Na. *Clinical correlation: This is where LOOP diuretics work, blocking the Na/K/Cl pump (furosemide/Lasix). |
|
What actions occur in the Early Distal Tubule?
|
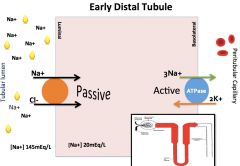
*5-7% of Na+ is reclaimed here (Na/Cl cotransporter).
*Powered by 2° active transport (Na/K pump). *Thiazide diuretics act here. |
|
What actions occur in the Collecting Duct?
|
*<5% of Na is reclaimed here.
*Epithelial sodium channels (ENaCs) in principal cells have an important regulatory role; they fine-tune Na excretion. |
|
|
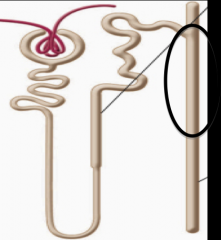
What all occurs in the Cortical Collecting Duct?
|
*The number of ENACs determines amount of Na reabsorption. This is the fine-tuning!
|
|
|
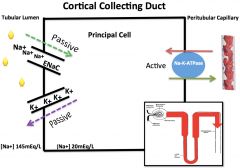
Sometimes the GFR will increase slightly with random vasoconstriction of the efferent arteriole. How is Glomerulotubular Balance maintained?
|
*If the tubules did not respond by increasing Na reabsorption, Na excretion would increase significantly.
*Let’s say the filtered load of Na is 25,200 mEq/day. A 1% increase in filtration would mean an additional 252 mEq would be filtered. *Total amount of Na in the ECF is 1960 mEq, making a loss of an extra 252 mEq of Na significant. *Compensation by the tubules prevents this loss. *Higher π from plasma proteins upstream encourages compensatory reabsorption downstream. |
|
|
How does the kidney know when to increase or decrease sodium reabsorption (how does it know when you are volume depleted or have volume overload)? 5
|
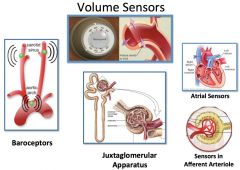
1) Aortic arch baroreceptors.
2) Carotid sinus baroreceptors. 3) Atrial sensors. 4) JGA's macula densa senses NaCl delivery. 5) Afferent arteriole sensors. |
|
|
So, if the sensory systems detect that there is too much volume or too little volume, how does the body respond? 4 ways.
|
1) Sympathetic Nervous System.
2) Renin-Angiotensin-Aldosterone. 3) Atriopeptin (ANP). 4) Starling Forces. |
|
|
Describe the sympathetic response to a decrease in volume:
|
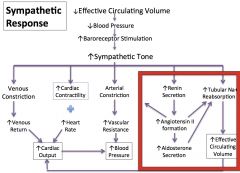
*The kidney's role is with the renin system to increase reabsorption and increase volume.
|
|
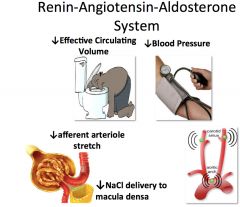
How does the renin system sense and respond to a decrease in volume?
|

*Sense: Receptors (baroreceptors or macula densa).
*Response: Renin cascade! *Renin comes from afferent arteriole cells (JGA)--> you know the downstream effects. |
|
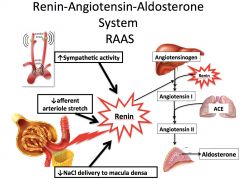
What are the effects of Angiotensin II?
What are the effects of Aldosterone? |
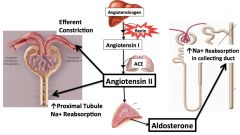
*Angiotensin II:
1) Vasoconstriction of Efferent Arteriole. 2) Increases proximal tubule Na reabsorption by stimulating Na/H anti-porters. 3) Increases aldosterone levels. *Aldosterone: 1) Increases Na reabsorption in Collecting Duct by increasing the number of ENAC channels. |
|
|
What are the actions of ANP?
|
1) Dilates blood vessels.
2) Increases Na excretion some by increasing GFR (constricts efferent arteriole, dilates afferent arteriole). 3) Prevents tubular reabsorption some (antagonizes aldosterone and Angiotensin II; not well understood). |
|
|
Describe the role of Starling Forces in the setting of decreased plasma volume:
|
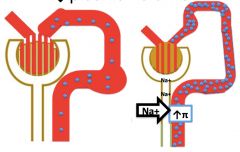
↓ Plasma volume results in higher π (oncotic pressure) in peritubular capillary blood which ↑ Na+ reabsorption.
|
|
|
Summarize the proximal tubules's work if you get volume depleted:
|
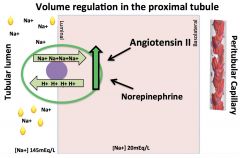
*BOTH Angiotensin II and NE act to increase the actions of the Na/H anti-porter, which raises Na reabsorption.
|
|
|
Summarize Volume regulation in the Loop of Henle and the Early Distal Tubule in the setting of volume depletion:
|
*NOT RESPONSIVE TO NE OR ANGIOTENSIN II.
*Na reabsorption is FLOW-dependent in the loop of Henle and early distal tubule. *Maintains glomerular tubular balance but DOES NOT provide an effective response to changes in ECF. |
|
|
Summarize Volume regulation in the Cortical Collecting Duct in the setting of volume depletion:
|
![*Occurs in Principal Cells (not Intercalated cells).
1) Aldosterone increases Na/K pump activity, which increases the [gradient] into the cell.
2) Aldosterone also increases the number of ENACs.](https://images.cram.com/images/upload-flashcards/67/14/41/2671441_m.jpg)
*Occurs in Principal Cells (not Intercalated cells).
1) Aldosterone increases Na/K pump activity, which increases the [gradient] into the cell. 2) Aldosterone also increases the number of ENACs. |
|
|
Take home points from this lecture:
|
*Na regulation is one of the kidney’s most important functions. Na determines extracellular volume and plasma volume. Under normal circumstances, daily Na intake = daily Na excretion.
*Since Na is freely filtered in the glomerulus, the majority of filtered Na must be reclaimed by the tubules. Na is reabsorbed across the luminal membrane of tubular cells and returned to the blood via Na/K pumps in the basolateral membrane. These Na/K pumps create an electrochemical gradient that drives reabsorption. *>95% of the filtered Na has been reabsorbed by the time the filtrate reaches the cortical collecting duct. Nonetheless, the cortical collecting duct plays an important role in Na regulation. Fine adjustments in Na excretion are made in the cortical collecting duct. *The ability to defend against threats to circulating volume (by moderating Na excretion) is vital to survival. Multiple responses occur to changes in effective circulating volume: 1) Sympathetic nervous system 2) Renin-angiotensin-aldosterone system *Baroceptors sense a decrease in effective circulating volume and a sympathetic response stimulates proximal tubule Na reabsorption in 2 ways: 1) Direct stimulation of Na/H antiporters. 2) Renin release leading to an increase in angiotensin II which stimulates Na/H antiporters. *The cells of the macula densa sense a decrease in NaCl delivery when effective circulating volume decreases. Juxtaglomerular cells increase renin release and the renin-angiotensin-aldosterone cascade is activated. Angiotensin II increases Na reabsorption in the proximal tubule. Aldosterone increases Na reabsorption in the cortical collecting duct. |
|
|
A 20-year-old student presents to student health services with NVD X 3 days after eating her roommate’s left over sushi. She complains of weakness and dizziness. Physical exam is notable for Low BP (80/60) and dry mucous membranes.
The patient’s effective circulating volume has: Increased Decreased Not changed |
Decreased
|
|
|
In order to defend circulating volume and maintain organ perfusion which of the following responses will occur?
Vasodilation in the extremities Bradycardia The kidney will increase Na+ excretion The kidney will avidly conserve Na+ |
The kidney will avidly conserve Na+
|
|
|
In order to defend circulating volume and maintain organ perfusion which of the following responses will occur?
A-Aldosterone will increase Na+ reabsorption in the cortical collecting duct B-Angiotensin II will increase Na+ reabsorption in the proximal tubule C-Renin will increase Na+ secretion throughout the nephron D-Epinephrine will increase proximal Na+ secretion E-A and B F-All of the above |
E-A and B
Aldosterone will increase Na+ reabsorption in the cortical collecting duct. Angiotensin II will increase Na+ reabsorption in the proximal tubule. |

