![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
151 Cards in this Set
- Front
- Back
|
APTT stands for?
measures ? normal APTT time? |
- Activated Partial Thromboplastin Time (name doesn't make a whole lot of sense, b/c thromboplastin is TF of extrinsic system)
- measures INTRINSIC and common pathway expected time 60-120 sec AI |
|
|
Total Blood Volume (TBV)/ ADULTS:
as a R.o.T. = ??? |
TOTAL BLOOD VOLUME (TBV)/ ADULTS:
~6-8% of body weight OR 60-80 ml / Kg BW |
|
|
FLUID REPLACEMENT THERAPY
how much fluid is needed (without over-infusing)? How long before blood (fluids) reach tissues? |
R.o.T: severely dehydrated patients can be given up to the equivalent of
their total blood volume within 1. hour using crystalloids = ~7% of body weight (or 70ml/kg) Note: 1hr later, 75% of infused fluid will have moved out of vessels into tissues re-hydrates ECF and ICF For Maintenance: ~same volume over 24 hours (variable) |
|
|
What layers are visible after blood is centrifuged?
Approx. % by volume? |
plasma 59%
BUFFY COAT = top layer of white blood cells and platelets, ≈ 1 % HEMATOCRIT (=PCV) = % of total blood volume occupied by RED BLOOD CELLS, ≈ 40 % (±15% sp. dpd *formed elements are represent by bottom two layers |
|
|
PCV
|
hematocrit
OR packed cell volume = volume occupied by RBC |
|
|
plasma is made up of?
|
7% proteins (albumin, fibrinogen, globulin,etc)
91.5% water 1.5% other solutes (electrolytes,etc) |
|
|
Plasma Proteins are derived from ?
|
- are derived from liver (albumin, some globulins, fibrinogen) & WBC
|
|
|
All formed blood elements
originate from _____; it replenishes itself and differentiates into ________. |
All formed blood elements
originate from same pluri-potent stem cell pool ; it replenishes itself and differentiates into 2 stem cell lines: Myeloid & Lymphoid |
|
|
Hemopoiesis occurs in _____.
Hemopoiesis is controlled by ______? |
Hemopoiesis occurs in red bone marrow + lymphoid tissue
(before birth also in spleen, liver, thymus, yolk sac, lymph nodes) Hemopoiesis is controlled via CSFs (colony stimulating factors), interleukins, cytokines, thrombopoietin, erythropoietin |
|
|
Which have largest RBC: salamander, camel, ostrich, snake? Smallest?
which are nucleated? what else of nucleus? |
salamander is largest; camel has smallest
which are nucleated? amphibians, reptiles, birds <- but RBC nucleus not functional |
|
|
examples of plasma proteins not produced in liver?
|
antibodies and protein hormones
|
|
|
how does protein concentration in plasma compare to interstitial fluid?
where in body are caps more permeable to protein? |
higher than interstitial fluid
(capillary wall not permeable to protein, except in liver) |
|
|
approximate proportion of body weight occupied by blood in cat and dog? also volume per kg BW?
TBV: (just to get idea of range) In 20kg Dog? In 5kg Cat? |
5kg cats 5%
(50ml/kg x 20kg = 1000ml = 1L) 20kg dog is ~9% or 90ml/kg body weight (90ml/kg x 20kg = 1.8L) |
|
|
approximate proportion of body weight occupied by blood:
in 700kg cold-blood horse? in bird? |
c/b horses with 700 kg BW, 7% or 70kg/ml:
~so TBV 49,000 ml or 49L birds: higher 10% *cold blooded horse is lightly muscled, and have lower hematocrit than warm/hot blooded horse b/c fewer RBC |
|
|
proportion of blood cells that are RBC?
approx. proportion of blood volume occupied by RBC's? |
90%
40% |
|
|
If goat has twice as many erythrocytes as dog, why is hematocrit so much lower?
|
RBC of dog more than x2 size
|
|
|
compare blood volume between active and inactive animals
|
active animal has larger blood volume e.g. warm blooded horse
|
|
|
OSPT stands for?
measures ? normal OSPT time? |
OSPT = One Stage Prothrombin Time
-> measures EXTRINSIC and common pathways (expected time < 10 sec!) OE |
|
|
Plasma Protein (PP) conc in plasma ?
|
rel. stable: 7g / 100ml
|
|
|
P.P. increase during ?
what are acute phase proteins? |
can increase in inflammations (e.g. globulins + fibrinogen, also ferritin <- binds iron, inhibiting microbe iron uptake)
called "acute phase proteins" (> in large animals) = absolute increase Lab report: PCV normal & PP increased P.P. can look increased in haemo-concentration / dehydration = relative increase (all proteins) Lab report: PCV & PP increased |
|
|
P.P. can be decreased during?
|
can be decreased e.g. in end-stage liver disease (lack of production)
OR after blood loss |
|
|
How many O2 bind to Hb molecule?
How many Fe bind to Hb? |
Each of four heme groups bind an Fe, the four irons bind an O2 molecule
->so 4 oxygens |
|
|
What blood parameters used to monitor deyhydration?
(give a standard value for each in %) |
PP (around 7%)
PCV (hemacrit)(around 40%) |
|
|
Approx. life span of RBC in domestic animals?
cat? pig? bird? |
survival of RBCs is limited to: in most spp. is 4-5 months
cat, pig: 2 months; birds 5 weeks - short life span b/c lack DNA, RNA to make new protein |
|
|
Blood cell production in fetus?
Blood cell production in adult? |
fetus - liver, spleen
adult - bone marrow...particularly flat bones (sternum, ribs, pelvis) ! - if challenged, liver and spleen contribute |
|
|
Mature RBC are approx. ____% hemoglobin
|
Mature RBC are ~33% hemoglobin
|
|
|
Name stages of erythropoiesis?
|
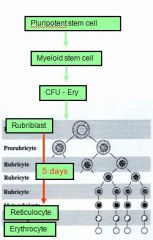
(1) Pluripotent stem cell
Erythropoietin stimulates commitment from (2) Myeloid stem cell into (3) CFU/erythrocyte (4) rubriblast (5) reticulocytes. (6) erythrocyte |
|
|
Originate from Myeloid stem cells:
|
* RBCs
* Platelets * Monocytes * Granulocytes |
|
|
- takes ___ days from stem cell to reticulocyte
during this time: (3) What comes before reticulocyte? What change signifies the formation of a reticulocyte? |
- takes 4-5 days from stem cell to reticulocyte
during this time: - cells become smaller - Hb content increases - nucleus condenses and extruded |
|
|
extrusion of nucleus correspond with what precursor?
where are found? what changes do they undergo in addition to loss of nucleus? time frame? |
extrusion of nucleus = reticulocyte
RETICULOCYTES migrate from b.marrow into CIRCULATION. & mature within 1-2 days to mature RBCs = loss of remaining RNA material which means loss of HB synthesis ability |
|
|
normal Reticulocyte count/blood: ____% ?
Exception? |
normal Reticulocyte count/blood: 1-2%
Exception: healthy horses and ruminants only release mature RBCs -> NO reticulocytes circulate in healthy ones |
|
|
Erythropoiesis requires adequate supplies of ? (5)
|
Erythropoiesis requires adequate supplies of: iron, folic acid and Vit B(2,6,12)
|
|
|
RETICULOCYTOSIS
(give time frame, etc) when highest? how long to see affect? example of max proportion compared to mature RBC? |
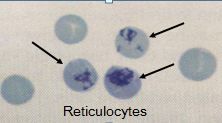
- elevated lvl of reticulocytes appear in circulation (e.g. up to 25 % in dogs) if blood loss has occurred
- usually change apparent 3-5 days after challange, w/peak after 7 days |
|
|
Can immature RBC in circulation contribute to oxygen carrying capacity?
|
Although immature, these cells contribute to O2 carrying capacity while still increasing their Hb content
|
|
|
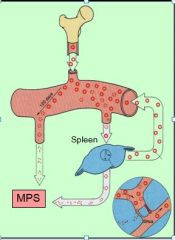
Removal of aged RBCs occurs where?
|
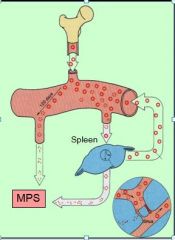
- rupture during SPLEEN passage
(tight traberculae) and are absorbed by macrophages - or are selectively removed by Mononuclear – Phagocytic System (Macrophages in spleen, liver, bone marrow!) ~ so three potential places |
|
|
What parts of RBC do the macroph. recycle?
|
Globin (amino acids)
Protoporphyrin (heme after iron removed) Iron note: Protoporphyrin then becomes billirubin |
|
|
Fate of heme group?
|

- Fe removal to become Protoporphyrin
- converted to Bilirubin - released into circulation, and excreted by liver in bile juice |
|
|
Iron re-cycling: ?
hint: what is name of plasma protein for transport of iron? for storage? |

- iron is removed from Heme, released into circulation and binds to plasma protein to form TRANSFERRIN = Fe-transport form; iron can either go to liver for storage OR bone marrow where transferrin binds strongly with erythroblastic receptors, Fe is released into myeloblast cells for Hb synthesis
- Transferrin can also release Fe into any other tissue, i.p. liver; Fe then binds to intracellular protein to form FERRITIN = Fe-storage form; is released from storage when needed |
|
|
ferritin
|

protein-iron complex (plasma protein) of macrophages from liver, spleen, and b.marrow
|
|
|
transferrin?
|

in blood, iron released (from heme) is transported in the protein-iron complex "transferrin"
to liver for storage OR b.marrow to be reused in hemoglobin synthesis |
|
|
If ferritin stores are full, any excess iron is stored as nearly insoluble _____?
(liver, pancreas, heart) -> can lead to toxic cell damage |

excess iron is stored as nearly insoluble HEMOSIDERIN
can lead to toxic cell damage (Hemosiderosis / Iron-Storage-Disease) |
|
|
ERYTHROPOIETIN (EPO)
what does it do? where made? where does it go? |
- controls rate of RBC production
- made in kidney - when low O2 sensed by RENAL tubular receptors , production of EPO increases - EPO then goes to b.marrow |
|
|
Name three lab parameters for evaluating erythron and anemia
|
MCV
MCHC MCH~Mean Corpuscular Hb |
|
|
Anemia
|
Anemia = deficiency in oxygen carrying capacity
|
|
|
hemolytic anemia
causes? regenerative? |
hemolytic anemia is when RBC destroyed so rapidly that bone marrow is unable to replace them
can be caused fragile RBC due to inherited diseases, etc. macrocytic-hypochromic, regenerative |
|
|
Characterize dyshemopoietic anemias caused by nutritional deficiencies:
Where is this common? |
Dyshemopoietic anemia = non-regenerative
Nutritional deficiencies,e.g. LACK of IRON: cells cannot produce sufficient Hb (hypochromic = pale color) and become nonregenerative, MICROCYTIC (small) Commonly in piglets, b/c milk is low in iron and grow quickly |
|
|
MCHC
what are units? |
1 of 3 RBC PARAMETERS
MCHC = Mean Corpuscular HEMOGLOBIN Concentration in % ~ describes the Hb content in a deciliter of RBCs - MCHC = Hb x 100 / Hct = g hemoglobin / dL blood normochromic = normal conc. of Hb within RBC = 33% hypochromic = low conc.of Hb, pale in color e.g iron deficiency;immature RBCs hyperchromic = beyond satur. point, artifact due to hemolytic sample |
|
|
hemorrhagic anemia?
causes? regenerative? reticulocyte %? |
- hemorrhagic anemia is due to blood loss and blood cell loss.
- it is regenerative, so reticulocytes up and blood cells present tend to be macrocytic-hypochromic |
|
|
MCV
|
MCV = Mean Corpuscular Volume (of RBC) in femtoliter
~describes size of 1 RBC!! MCV (femtoliter per CELL) = Hct (%) x 10 / RBC (cells/liter) = Hct% x 10 x 1L / cell <- dividing by fraction so units flip |
|
|
If antibodies not present, the recepient of blood (with different antigen),...
|
If antibodies not present, the recepient slowly develops antibodies after 1st transfusion; initially only mild delayed reaction.
2nd transfusion? gloves are off... |
|
|
What happens to RBC numbers at high altitude?
|
- each RBC transports less O2
- therefore more EPO made, but take couple days RBC to be made |
|
|
5 steps of hEmostasis?
What is primary hemostasis? What is secondary hemostasis? |
Hemostasis = sequence of responses that stop bleeding
1. vascular spasm 2. platelet plug formation = primary hemostasis 3. blood clot formation = coagulation = secondary hemostasis 4. healing 5. clot removal = fibrinolysis |
|
|
another word for platelets?
|
thrombocytes
|
|
|
BLOOD TYPING
|
= determination of the RBC antigens present in an individual;
done to determine universal donor animals |
|
|
universal donor in dog should be?
|
e.g. DOG: should be negative for DEA 1.1; 1.2 and 7
(because these are the strongly antigenic groups) |
|
|
CROSS MATCHING
Major? Minor? |
MAJOR: expose Donor’s RBCs to Recipient’s plasma and observe for agglutination
MINOR: expose Recipient’s RBCs to Donor’s plasma and observe for agglutination |
|
|
platelets derived from ?
|
Origin: derived from bone marrow megacaryocytes
(pluripotent stem cell – myeloid stem cell – CFU/Meg – megakaryoblast – megakaryocyte – fragmentation into hundreds of platelets); controlled by hepatic thrombopoietin |
|
|
platelets contain?
|

- contractile proteins (actin, myosin, thrombosthenin)
- ADP, ATP - Prostaglandins, serotonin, clotting factors, endothelial growth factors, etc - Calcium |
|
|
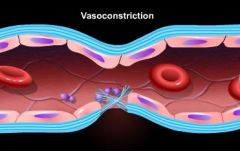
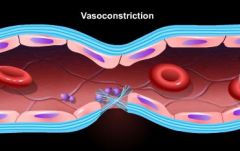
STEP 1 of hemostasis: Vasospasm is caused by?
What is main point of this? |
is caused by
- Immediate release of ENDOTHELIN from damaged cells - later: release of THROMBOXANE A2 (= prosta- glandin derivative important in next step) and serotonin (vasocontrictor) from platelets - myogenic contraction of damaged smooth muscle cells -initial step of vasoconstriction to minimize additional blood loss |
|
|
How long can vasospasm last?
|
minutes to hours
|
|
|
What releases von Willebrand Factor (vWF)?
|
Damaged endothelial cells!
|
|
|
___ promote vasospasm )?
hint: (step 1 of hemostasis) they are released from? |
Serotonin and Thromboxane A2
platelets prior to plug form. |
|
|
difference between hemorrhagic and hemalytic anemia?
|
- hemalytic disorders arise when RBC are lysed prematurely
- in hemarrhagic anemia, the RBC are not being lysed, but are lost along with plasma/fluids.. - in both cases, cells being replaced but low hb and increased # of immature RBC lead to anemia |
|
|
Types of dyshemopoietic anemia and examples:
|
All are non-regenerative.
1. Nutr.deficiencies e.g. lack of iron - weird b/c microcytic 2. Anemia of chronic (imflammatory) disorders = ACD or AID e.g. FeLV, Ehrilichia, cancer, tissue necrosis 3. Chronic renal disease leading to lack of EPO 4. Drug-related suppression, e.g. by estrogene |
|
|
STEP 2: Platelet plug formation
started when...? ~describe the course of events: |

Endothelial Damage / Exposure of Collagen:
- Damaged endothelial cells release von Willebrand Factor - vMF binds to exposed collagen fibers and cell membrane (conf. change), serves as receptor for platelets, which degranulate, releasing ADP, serotine, thromboxane A2 |
|
|
Characterize dyshemopoietic anemias caused by ACD:
Where is this common? |
- anemia of CHRONIC (inflammatory) disorders = ACD or AID
- seen in chronic infections, FeLV, Ehlic., inflammations, cancer, tissue necrosis -release of toxins, e.g. CYTOKINES or Tumor Necrosis Factor, which suppress EPO - fewer RBCs are released (but remaining are normal) - typically normocytic/ normo- chromic |
|
|
____ attract more platelets?
they are released from? |

ADP and Thromboxane A2 released from platelets
(part of positive feedback during form. of plug) |
|
|
When do hemorrhagic (and hemolytic) anemias can become chronic disorders?
|
exhaustion of iron stores after long stimulation
eventually become non-regenerative anemias eg. GI ulcers, parasites |
|
|
What are consequences of anemia?
|
- REDUCED TISSUE OXYGENATION
- anaerobic metabolism, low ATP, so Na/K pump down, cell function down - increased lactic acid, metab. acidosis, cardiotoxic |
|
|
How does body compensate for anemia?
|
- increased EPO
- hyperventilation - vasodilation to vital organs, vasoconstriction to periphery - HR up, etc |
|
|
What happens when Na/K pump down?
|
intracellular Na - up
extracellular potassium up because repolarization not occurring properly |
|
|
How does inflammation affect the size of the buffy coat?
|
incr. in WBC, so size of buffer coat increases
|
|
|
1 L of blood = ?
|
1 kg
|
|
|
A huge increase in the buffy coat can be a sign of what?
|
leukemia
|
|
|
If ferritin stores are full, an excess Fe is stored as nearly insoluble ___. This can lead to toxic cell damage.
|
Hemosiderin
|
|
|
sequence of responses that stop bleeding called?
|
Hemostasis
~it is fast, localized, and carefully controlled |
|
|
Erythropoisis is controlled by...
|
tissue oxygenation
|
|
|
Clinical signs of dehydration: (not asking about blood tests, but rather physical characteristics one might find examining dehydrated animal)
|
* Turgid mucous membranes
* Increased Capillary Refill Time * Eyes sunken in * Slow recoil to skin test |
|
|
When Transferrin releases Fe into a tissue, Fe binds to an intracellular protein to form...
|
Ferritin
|
|
|
Main function of Erythrocytes (RBCs)
|
exchange of gases, regulation of blood pH
|
|
|
Why does erythropoesis shift from all bones to only the marrow of flat bones?
|
B/c as the animal matures, the marrow of long bones fill with fat.
|
|
|
Plasma proteins are derived from...
|
liver and WBC
|
|
|
Carries fat soluble substances since most of plasma is H2O.
|
Albumin
|
|
|
Plasma proteins are essential in maintaining...
|
osmotic pressure
|
|
|
Average diameter of a capillary
|
3um
|
|
|
Size of RBC
|
7um in diameter
|
|
|
ERYTHROPOIESIS is controlled by TISSUE OXYGENATION:
where is low level detected? Where EPO made? |
Withdrawal of RBCs -> HYPOXIA -> RENAL tubular receptors -> ERYTHROPOIETIN (EPO) release -> Bone Marrow -> stimulation of Erythropoiesis -> release of new RBCs
|
|
|
Part of RBC that is converted to bilirubin, released into circulation, and excreted by the liver in bile juice.
|
Protoporphyrin
|
|
|
Part of RBC reused for protein synthesis?
|
Globin
|
|
|
RBCs in fish
where made in bony fish? in cartilaginous fish? |
* nucleated
* produced in spleen and liver (bony fish) * produced in circulation in cartilaginous fish |
|
|
what is responsible for recycling most RBC parts?
|
macrophages
|
|
|
In healthy animal, every day approx. what % of all RBCs die / are removed and have to be replaced ?
|
1% everyday
|
|
|
NSAIDs
|
Non-steroidal anti-inflammatory drug
e.g. ibuprofen and aspirin prostaglandin synthesis inhibitors, prostaglandins cause vasospasms and attract platelets used for anticoagulation to prevent excessive clotting |
|
|
increase in RBC numbers
|
Polycythemia
|
|
|
Primary Polycythemia
|
Primary Polycythemia = P. vera (rare)
lack of feedback control -> uncontrolled RBC production (myeloproliferative disorder) -> hematocrit can increase upto 60-70% -> high viscosity -> reduced blood flow but: sight hounds have naturally high PCV values |
|
|
Secondary Polycythemia
how common? where/when does it occur? what changes? |
2^ polycythemia (common)
= physiological response to oxygen deficiency due to e.g. high altitudes, cardiac failure, lung diseases -> Hct increases by a few %; plasma unchanged |
|
|
Transient Polycythemia
|
Splenic contraction due to excitement & exercise seen in horses, cats, sight hounds:
-> elevated PCV, but normal plasma proteins) NOT pathological! |
|
|
type polythemia that is very common?
|
"Relative Polycythemia” (very common)
is not a true polycythemia, but is caused by: - dehydration = fluid loss -> all blood components become more concentrated = hemoconcentration -> typically shows as elevated PCV and elevated plasma protein levels |
|
|
Lassie, an elderly *****, suffering from uterine cancer and has become anemic.
What type anemia? Likely cause? ~characterize and describe RBC's: |
Dyshemopoietic anemia (non-regenerative): specifically of chronic disorders -> release of toxins e.g. tumor necrosis factor (or cytokines) which suppress EPO -> fewer RBCs released but remaining normocytic/ normochromic
|
|
|
Concentratoin of RBCs
|
5 million / ul
|
|
|
Originate from Lymphoid stem cells:
|
* B-lymphocytes
* T-lymphocytes |
|
|
Conc. of platelets in blood?
Half-life? |
150.000 – 300.000 / ul
ca 10 days |
|
|
explain how RBC could be hyperchromic?
|
can't be; just artifact when blood is analyzed, elevated b/c of residual hemoglobin floating (from dead cells)
|
|
|
Femtolitre
|
unit volume equal to 10^(−15) liter
|
|
|
during platelet plug, this glue-like substance to promotes adhesion
|

4. platelets release ADP and Fibronectin -> glue-like substance to promote adhesion
|
|
|
Platelet plug: loose plug is formed within _____ to seal off the injury site
|
1-2 minutes
|
|
|
Name 3 platelets factors release by platelets that involved in clotting:
|
(III, V and VIII)
|
|
|
Why does calcium help with clotting?
|
Most clotting factors negatively charged, so Ca+2 helps bring in.
|
|
|
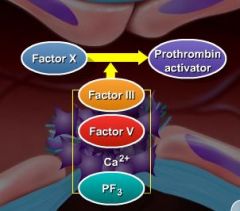
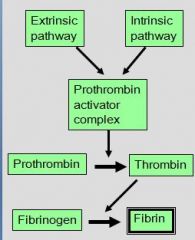
______ lead to formation of a Prothrombin-Activator Complex?
COMMON pathway begins _____? |
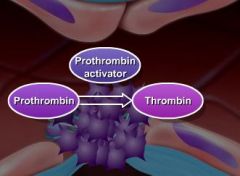
EXTRINSIC and/or INTRINSIC pathway, each produces unique factors important in activating PAC.
COMMON pathway begins activation of Prothrombin to Thrombin via Prothrombin-Activator Complex (represent merger of ext/intrinsic pathways) |
|
|
factors found in both intrinsic and extrinsic pathways?
|
X, V, Ca
|
|
|
Factor XII activates what?
leads to? which factors involved in cascade? |
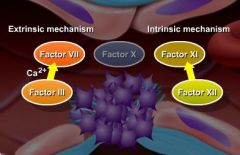
activates an enzymatic cascade of INTRINSIC (inside blood vessel or plasma based) system (kallekrein, factors XI, IX, VIII, X, V, Ca) leading to P.A.C.
note: X, V, Ca found in both |
|
|
which is plasma-based pathway during stage 1 of clot formation?
what happens during this? |
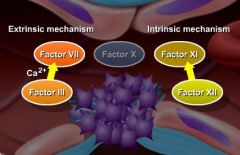
INTRINSIC SYSTEM (inside blood vessel)
Change in surface charge of endothelial membranes (neg. charge in cell released) binds and activates Plasma Factor XII, e.g. caused by inflammatory reactions (endotoxins); activated platelets; contact with glass surface (bleeding not necessary!) |
|
|
which is tissue-based pathway during stage 1 of clot formation?
|
EXTRINSIC SYSTEM: comes from outside blood vessel, membrane disrupted
Injured tissue expresses Tissue Factor |
|
|
What is Tissue Factor?
What is it part of? What does it activate? |
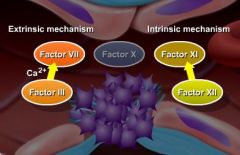
Injured tissue Factor (Thromboplastin), of extrinsic pathway, activates an enzymatic cascade (factors VII, X, V, Ca) leading to P.A.C
note: extrinsic comes from outside blood vessel, membrane disrupted |
|
|
Which pathway (intrinsic or extrinsic) of clot form. is faster and more powerful?
|
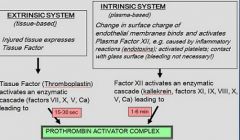
EXTRINSIC SYSTEM (tissue-based)
is only 15-30 second long. ~in contrast, Intrinsic system (plasma-based) takes 1-6 min |
|
|
Which enzyme of clot formation depends relies of vitamin K?
Name Vit K antagonist..what does it cause? |
Prothrombin
Coumarin = Vit K antagonist -> impairs liver synthesis of several clotting factors incl. Prothrombin |
|
|
Prothrombin
|
- proenzyme or inactive enzyme precursor, converted by P.A.C. to active thrombin
- is a hepatic alpha globulin - its liver synthesis is Vit K dependent - attaches itself to activated platelets |
|
|
Is factor XII a plasma or platelet factor?
|
Plasma Factor, of plasma-based INTRINSIC SYSTEM
activates an enzymatic cascade (kallekrein, factors XI, IX, VIII, X, V, Ca) leading to PAC |
|
|
What kind of factor is Thromboplastin?
identify any related related factors.. |
Tissue Factor, expressed by injured tissue
activates enzymatic cascade of extr.sys. (factors VII, X, V, Ca) leading to PAC |
|
|
What polymerize into long fibers and X-link into meshwork w/i and around the platelet plug?
Bonus: what is time frame? |
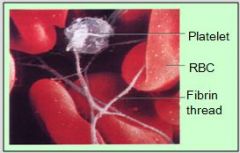
FIBRIN, this meshwork = STABLE CLOT
-> bleeding stops (within 3-6 min after injury) |
|
|
How is FIBRIN formed?
|
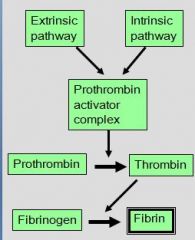
Thrombin hydrolyses FIBRINOGEN (=hepatic soluble protein; already bound to activated platelets) into FIBRIN monomers
|
|
|
CLOT RETRACTION
|
W/i the next 30 minutes after stable clot (fibrin meshwork around plug), platelets contract more and pull fibrin threads together
-> clot tightens and pulls edges of injured blood vessel together |
|
|
SERUM vs plasma?
|
SERUM = Plasma minus clotting factors
~blood fluid that remains after hemostasis has occurred is serum |
|
|
Hemostasis: Healing
|
Hemostasis: Step 4
- fibrin meshwork serves as scaffolding for fibroblasts, stim. by platelet derived endothelial GF. - wound healing / scar formation begins |
|
|
Fibrinolysis
what is it? time rame? enzymes involved? |
Hemostasis: Fibrinolysis = removal of clot (1-2 days after clot formation)
tissue-Plasminogen Activator = tPA activates hepatic plasma factor Plasminogen to PLASMIN = proteolytic enzyme - plasmin nibbles at fibrin fibers |
|
|
PLASMIN
|
PLASMIN = proteolytic enzyme
- plasmin hydrolyses fibrin fibers + clotting factors! into FDPs (Fibrin Degradation Products); |
|
|
FDPs are removed by
|
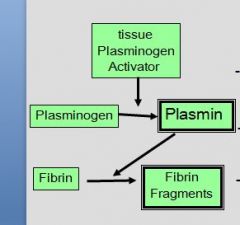
Fibrin Degradation Products are removed by macrophages
|
|
|
- _____ inhibit platelets adhesion
- secreted by ?? |
PROSTACYCLIN and Nitric Oxide -> inhibit platelets adhesion
secreted by intact endothelial cells and WBC |
|
|
What limits fibrin formation and positive feedback?
|
Fibrin binds Thrombin -> limits fibrin formation and positive feedback
(remember normally thrombin hydrolyzes fibronogen to form fibrin monomers, as well as +f/b of int/ext.systems) |
|
|
* ANTI-THROMBIN III
* ______from ____ combines with Anti-thrombin III and greatly augments its effectiveness |
ANTI-THROMBIN III (α globulin) deactivates Thrombin and other clotting factors
Heparin from Mast Cells / Basophils increases A-TIII's effectiveness |
|
|
In vitro anticoagulation
|
Calcium binding agents (e.g. citrate, oxalate, EDTA), heparin
|
|
|
In vivo anticoagulation
|
Heparin, Vit K antagonists, prostaglandin synthesis inhibitors (NSAIDs)
|
|
|
4 parameters for testing Hemostasis
|
1. Platelets counts
2. (Mucosal) Bleeding Time / in vivo 3. OSPT = 1 Stage Prothrombin Time 4. APTT = Activated Partial Thromboplastin Time |
|
|
(Mucosal) Bleeding Time
what does it test? |
TESTS PLATELET PLUG FORMATION (not clotting)
*stop time until bleeding stops after standardized small incision into skin or mucosa (expected time 1-5 min) -> measures functional ability of platelets and vMF to plug minute injuries |
|
|
OSPT
expected time? what is added? |
1 Stage Prothrombin Time:
-> measures EXTRINSIC and COMMON pathways (expected time < 10 sec) - measures clot formation in citrated plasma after addition of Tissue Factor, Platelet Factors and calcium |
|
|
APTT
|
APTT = Activated Partial Thrombo- plastin Time
- measures INTRINSIC and common pathway <- measures clot formation after clean venipuncture in citrated plasma and addition of contact activator (diatomaceous earth), Platelets Factors and Calcium (expected time 60-120 sec) |
|
|
heparin
|
anticoagulant; decrease clotting ability of blood and help prevent harmful clots from forming.
heparin will not dissolve blood clots already formed, but may prevent clots from becoming larger and causing more serious problems. (heparin is strong acid and - charged, but physiology processes it involves are unclear) |
|
|
Thrombocytopenia
|
decreased production (bone marrow; drugs; FeLV) or increased destruction (immune-mediated) or consumption
|
|
|
von Willebrand’s Disease (Form I,II,III)
|
= most common bleeding disorder in animals due to genetic lack / insufficiency of vWF -> platelets fail to adhere to injury sites -> spontaneous bleeding (or ); clinical signs can be mild / severe / fatal; described in ca 60 breeds of dogs with highest
prevalence in Dobermans |
|
|
Vit K deficiency / Rodenticide poisoning
|
Coumarin = Vit K antagonist -> impairs liver synthesis of several clotting factors incl. Prothrombin
Causes hemorrhagic anemia, regenerative so macrocytic, hypochromic, reticulocytes up, PP down, APTT prolonged, OSPT prolonged |
|
|
How much blood can you take from an animal
without endangering it? |
1% of Body Weight
(or 10 ml/kg) max (and i'm going out a limb here guys) 2% in healthy donor animals (or 20ml/kg) |
|
|
where do RBC get energy?
|
GLUCOSE dependent
energy gain depends on anaerobic glycolysis (no mitochondria = no Krebs cycle, no beta oxidation, no ETC) |
|
|
Thrombosis
|
clotting in an unbroken blood vessel, e.g. due to stasis, atherosclerosis (cholestoral build up), trauma, parasites, tumors if thrombus dislodges -> embolisms = blocking of blood vessels -> ischemia
|
|
|
give example of Thrombosis
|
Aortic Thromboembolism /cats (aka Saddle Thrombus) due to myocardial diseases -> thrombus formation in left atrium -> embolism into aorta -> often lodges at caudal trifurcation, blocking blood supply into iliac arteries
|
|
|
petechial
|
purple spot on the body, caused by a minor hemorrhage
|
|
|
Ecchymosis
|
subcutaneous purpura larger than 1 centimeter or HEMATOME, commonly called a bruise. It's pretty much same as a "petechia". It can be located both in skin as well as in mucous membrane.
|
|
|
Thrombopoietin
|
Hormone produced mainly by liver and kidney that regulates production of platelets by bone marrow; stimulates production and differentiation of megakaryocytes, the bone marrow cells that fragment into large numbers of platelets
|
|
|
Are Fibrinogen, prothrombin, factor VIII,
von Willebrand factor acute phase proteins? |
Yes b/c increase during inflammation; these are coagulation factors, trapping invading microbes in blood clots.
There are many others like Plasminogen, various globulins, complement factors, ferritin, etc. |
|
|
If O2 dissociation curve shift to right?
|
If shifts to right, O2 more likely to dissociate e.g. if pH down
|
|
|
Physio I Review:
CO2 transported in blood mostly as ? *skip this question until know everything else* |
Bicarbonate HCO3- , 70% of time
w/Hb, 23% of time |
|
|
Physio I Review:
Describe path of CO2 *skip this question until know everything else |
-Leaves tissues to ECF, thru capillary wall where enters RBC still as CO2
-CA in RBC, converts W + CO2 --> HCO3- and H+. - H+ binds to Hb and Cl- uptake drives HCO3- release into plasma |

