![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
137 Cards in this Set
- Front
- Back
|
What makes the canine estrus cycle different from any other species?
|
1. follicle produces progesterone just prior to ovulation 2. ovulated oocyte must mature before fertilization 3. no pregnancy recognition needed, both pregnant and non-pregnant ******* will go through the same diestrus period
|
|
|
How long are estrus and diestrus in dog?
|
both 7-10 days
|
|
|
estrogen levels highest and progesterone lowest during ?
|
estrogen levels highest and progesterone lowest during ESTRUS
|
|
|
follicular phase consists of ?
|
proestrus and estrus
|
|
|
ovarian artery provides ovary with
|
blood
|
|
|
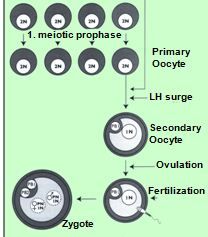
At sexual maturity there are 200,000 primary oocytes (immature eggs) in woman's ovary, what stage of meiosis are these primary oocytes arrested in?
Haploid or diploid? |
Diploid, arrested in prophase I of meiosis
|
|
|
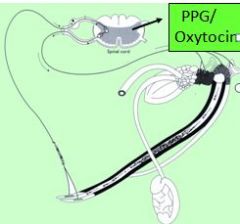
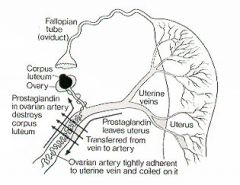
prostaglandin (for ovary) is produced in?
how does it get to artery? |
uterine mucosal lining
from uterine vein -> ovarian artery (counter-current system) -> ovary and luteal tissues |
|
|
What does estrogen come from?
|
Ovary
|
|
|
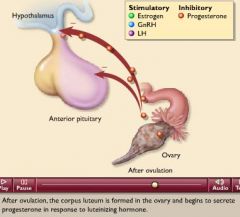
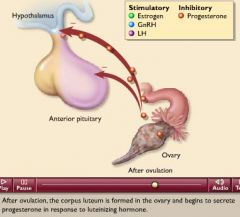
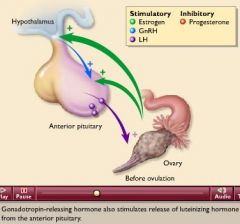
Estrogen triggers release of?
|
* triggers release of GnRH from ovary and LH from anterior pituitary
|
|
|
2 hormones that stimulate release of LH?
|
GnRH and estrogen from ovary
|
|
|
Production of prost. incr. during ?
|
luteal phase
|
|
|
are any new oocytes formed after birth?
|
NO
|
|
|
lifespan of mature oocytes (female)?
|

brief, ~24 hrs.
|
|
|
when is next estrus postponed?
|
if mating is successful
to provide embyro time to develop |
|
|
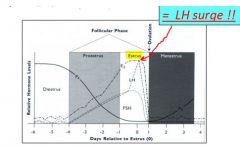
Estrous Cycle Summary
The estrous cycle involves periodic ovarian changes with 2 major phases: |
1. FOLLICULAR PHASE (ca 1/3 of cycle)
2. LUTEAL PHASE (ca 2/3 of cycle) |
|
|
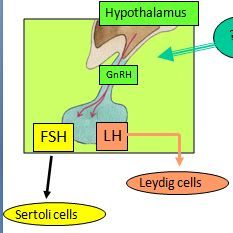
What stimulates Ant.Pit. gland to release (FSH & LH)?
|
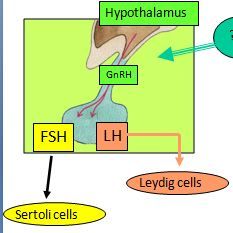
Hypothalamic (GnRH)
|
|
|
What stim. release of gonadal testosterone?
|
pituitary (FSH & LH)
|
|
|
HYPOTHALMUS contains what two centers:?
|
Hypothalamus contains:
Tonic center Surge center (only in female) |
|
|
Fetal testosterone inhibits ______ - males only have _______?
|
Fetal testosterone inhibits surge center; males only have tonic center
|
|
|
Tonic center of hypothalmus Produces?
|
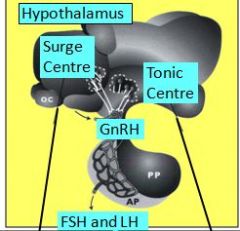
Produces GnRH (gonadotropin releasing hormone) → enters the portal system and stimulates anterior pituitary gland to produce and release the gonadotropins
|
|
|
What are the gonadotropins?
|
FSH - follicle stimulating hormone
LH - luteinizing hormone |
|
|
What type of breeders coordinate time of birth with favorable climatic conditions, and its main influences are photoperiod and ambient temperature? Examples?
Hint: these animals that have one or more estrous cycles during certain periods of year |
seasonal breeders
animals that have one or more estrous cycles during certain periods of year (not continuous) examples: sheep, goat (add more) |
|
|
What type of breeders breed during the spring/summer, the pineal gland responds to increased light which decreases melatonin and increases GnRH release?
|
long day breeders (horses, cats)
|
|
|
What are animals called that breed during AUTUMN/early WINTER?,
|

short day breeders (goats, sheep, deer)
|
|
|
In short day breeders (sheep, etc), pineal gland responds to decreasing light, by?
|
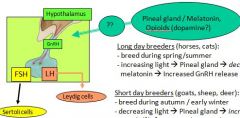
decreasing light --> increased opioids release from pineal & incr. GnRH release which stimulates spermatogenesis in male and female cycles?
|
|
|
What center shows spontaneous basal GnRH secretion in pulses of 1.5-2 hours, stimulates release of gonadotrophins FSH and LH from anterior pituitary gland?
|
Tonic Center
|
|
|
What produces low basal GnRH pulses until estrogen reaches critical threshold, responds with massive release of GnRH= surge?
|
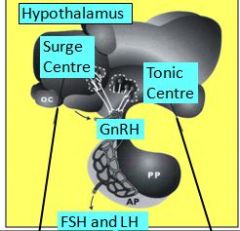
Surge Center
|
|
|
What is it called when progesterone lowers pulse frequency / amplitude of both centers (tonic and surge), and inhibits GnRH surge?
|
Negative feedback control
|
|
|
When reaching puberty, females enter a period of cyclical reproductive activity characterized by series of predictable events, involving the ovaries, uterus, and behavior, what is this called?
|
Estrous cycles
|
|
|
What is the process of acquiring reproductive competence (being able to support pregnancy)?
When does formation of graafian follicles begin? |
puberty in females
puberty, b/c it is hormone dependent (gr.follicle formation begins at puberty when tonic levels of LH and FSH begin to rise and fall with each oestrous cycle) |
|
|
What is the onset of puberty in females influenced by?
|
threshold body weight (fat tissue is powerful endocrine producer and main determinant in onset of puberty);
also genetic factors e.g. age (this is main factor in males), external factors or social factors |
|
|
What are polyestrus species?
|
cow, pig, human, have continuous cycles throughout the year
|
|
|
What are seasonal polyestrus species?
|
horse, cat, sheep, wild ruminants, continuous cycles during a certain season only, followed by silent period
|
|
|
What are monoestrous species?
|
dog, one cycle occurs, followed by silent period
|
|
|
What is a period without estrus cycles, caused by pregnancy, photoperiod, lactation, "stress"?
|
anestrus
|
|
|
What is luteolysis?
What causes luteolysis ? |
Regression of CL
PGF2 alpha |
|
|
What phase of the estrous cycle consists of and proestrus and estrus, is dominated by folliculogenesis with estrogen production, estrogen leads to sexual receptivity, and peak estrogen levels initiate ovulation via GnRH/LH surge?
|
follicular phase
|
|
|
What phase of the estrous cycle consists of Metestrus and Diestrus, conversion of ovulated follicle into corpus luteum with production of progesterone, progesterone prepares endometrium (inner membrane of the mammalian uterus) for pregnancy, ends with regression of corpus luteum?
|
luteal phase
|
|
|
What is the purpose of the estrous cycle?
|
release ova ready to be fertilized, coordinate time of ovulation with copulation, prepare uterus for attachment, switch over to pregnancy state or induce new cycle
|
|
|
During what phase for the hypothalamic tonic and surge center release basal pulses of GnRH, which stimulate corresponding FSH and LH?
|
proestrus
|
|
|
What is it called in proestrus, when FSH stimulated growth of a group of primary follicles to secondary and tertiary follicles?
|
folliculogenesis
|
|
|
In proestrus are FSH and LH both necessary to induce production of _____?
|
estrogen
|
|
|
In proestrus, what stimulates the theca cells to produce testosterone, which diffuses into granulosa cells?
|
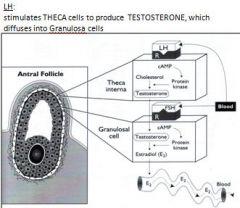
LH
|
|
|
In proestrus, WHAT stimulates granulosa cells to convert testosterone to estrogen, which is secreted with fluid into blood and forms the antrum?
|
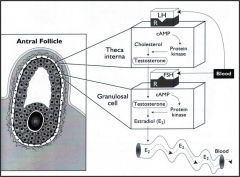
FSH
|
|
|
Upon gonadotropin stimulation, granulosa cells express more _____ receptors, and theca cells express more ____ receptors
|
FSH, LH
|
|
|
What is it called when cells become more sensitized to gonadotropins, leading to fast increase in estrogen concentration and proestrus behavior?
|
up-regulation
|
|
|
Exponential increase in estrogen induces what three events in sequence?
|
1. estrus begins
2. inhibin release 3. LH surge |
|
|
What happens when estrus begins?
|
standing heat, first sign of estrus is day 1 of cycle
|
|
|
What happens during inhibin release?
|
granulosa cells express LH receptors, producing inhibin, which inhibits FSH release, FSH decreases, leaving only 1 to few fully up-regulated follicles remaining active
|
|
|
What happens during the LH surge?
|
final increase in estrogen by fully up-regulated follicles, estrogen reaches critical threshold to activate surge center to release GnRH, leads to massive release of LH
|
|
|
Luteinization begins when?
|
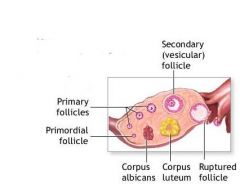
Luteinization, beginning after rupture of the ovarian follicle in ovulation (A) and progressing through vascularization and hypertrophy of the maturing corpus luteum (B, C) ; it is followed by regression (D) to the corpus albicans (E) .
_______________ process taking place in luteal cells of graafian follicles that have matured and discharged their eggs: cells become hypertrophied and there is vascularization and lipid accumulation (latter in some species giving a yellow color), the follicles then become corpora lutea. |
|
|
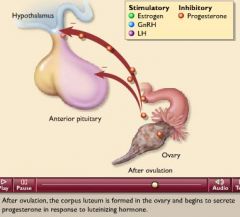
The LH surge initiates lutenization of granulosa and theca cells,
both begin to produce progesterone instead of testosterone/estrogen/inhibin which leads to what? |
estrogen decreases rapidly, estrus behavior declines, progesterone increases slowly
|
|
|
The LH surge blocks the ______ inhibiting factor.
|
meiosis
|
|
|
LH surge stimulates local production / release of histamine, proteolytic enzymes and prostaglandins E2 and F2a (vasodilation, proteolysis, transudation, myoid cell contraction) this leads to what?
|
follicular swelling, pressure increase, breakdown of connective tissue, rupture of mature follicle with release of oocyte into abdominal cavity
|
|
|
The most important event that the LH surge leads to is?
|
spontaneous ovulation
|
|
|
Some species do not ovulate spontaneously as part of cycle, but ovulation occurs only during or after copulation, coitus induces neuroendocrine reflex via vaginal and cervial receptors that leads to GnRH/LH surge, these kind of ovulators are?
|
induced ovulators e.g. cat
|
|
|
In induced ovulators, without copulation, there is no LH surge, no ovulation, what would happen?
|
tertiary follicles become atrophic
|
|
|
What species are induced ovulators?
|
cats, camel, ferrets, minks, rabbits
|
|
|
after ovulation, the follicular walls collapse & some bleeding occurs, antrum fills with blood clot called?
|
corpus hemorrhagicum
|
|
|
LH surge has induced lutenization in granulosa and theca cells; production of estrogen declines rapidly and progesterone increases slowly, what phase is this?
|
luteal phase
|
|
|
lack of estrogen abolishes estrus behavior, which means the end of estrus and the start of?
|
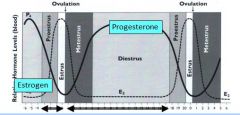
metestrus
|
|
|
Metestrus: corpus hemorrhagicum gradually luteinizes into the corpus luteum, which means?
|
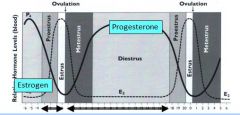
diestrus begins
|
|
|
Diestrus: what does the corpus luteum contain?
|
mature lutein cells
|
|
|
What do LUTEIN cells produce?
|
produce PROGESTERONE, which prepares the endometrium for potential pregnancy
|
|
|
What do small lutein cells develop from?
|
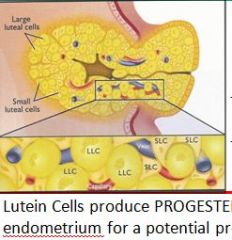
theca cells during early corpus luteum phase
|
|
|
What do large lutein cells develop from?
|
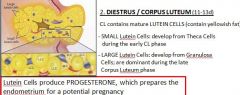
Granulosa cells, dominant during late corpus luteum phase
* following ovulation, granulosa cells divide rapidly forming CL |
|
|
Diestrus: the increasing progesterone levels suppress, but do not inhibit tonic and surge centers, which means?
|
GnRH is released in low frequency/low amplitude pulses, followed by low pulses of FSH and LH
|
|
|
What is necessary to keep corpus luteum viable?
|
LH pulses
|
|
|
FSH and LH pulses are sufficient to initiate folliculogenesis during diestrus called?
|
follicular waves
|
|
|
As long as progesterone is high (diestrus), the surge center cannot respond to elevated estrogen which means?
|
no LH surge, no ovulation, atresia (passage closed!)
|
|
|
Non-pregnant uterus starts to produce _______ towards the end of lutein phase.
|
prostaglandin F2a
|
|
|
PGF 2a reaches ipilateral ovary directly via a what?
|
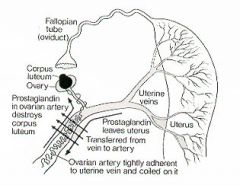
countercurrent blood system between uterine vein and ovarian artery
|
|
|
PGF2a leads to apoptosis of luteal cells, the CL regresses and progesterone production stops, means?
|
end of diestrus
|
|
|
In what species is PGF2a produced by the CL, and the uterus is not needed to induce luteolysis?
|
primates, probably carnivores
|
|
|
When progesterone decrease lifts suppression on ?
which means? |
no more suppression on hypothalamic GnRH release,
|
|
|
After progesterone decr and GnRH pulse increase again in frequency/amplitude, which increases FSH and LH, this means?
|
new cycle can begin with proestrus
|
|
|
In luteolysis, oxytocin is released from large luteal cells which initates?
(Where is oxytocin released from in dogs and primates?) |
In luteolysis, oxytocin released initiates PGF2a release from the endometrium
(however oxytocin is released from posterior pituitary gland in primates, dogs) |
|
|
What species are oxytocin and PGF2a released in pulses?
|
sheep
|
|
|
*PGF2a* is produced by ___ when stimulated by ____?
acts on ____ to cause ____? |
Produced by uterus when stimulated by oxytocin, if NO implantation during follicular phase.
Acts on corpus luteum to cause luteolysis, forming corpus albicans and stopping production of progesterone. Action of PGF2α is dependent on number of receptors on corpus luteum membrane. |
|
|
PGF2a receptor numbers are high only in what cells?
|
large lutein cells, during mid to late diestrus, PGF2a can induce luteolysis only during this time
|
|
|
What can be used to induce luteolysis in all species?
|
exogenous PGF2a
|
|
|
What can inhibit PGF2a synthesis (in ruminants and pigs, but not in the mare)?
|
acute/chronic endometritis, no luteolysis, persistant corpus luteum, persistant progesterone release, cycle locked in diestrus
|
|
|
The PGF2α isoform 8-iso-PGF2α is significantly increased endometriosis, being a potential causative links in endometriosis-associated oxidative stress.[1
|
The PGF2α isoform 8-iso-PGF2α is significantly increased endometriosis, being a potential causative links in endometriosis-associated oxidative stress.
|
|
|
What phase is under estrogen: proliferation of endometrium, increasing thickness, hyperemia & swelling of vulva, endometrial and cervical glands secrete thin, string-forming mucous?
|
proliferative phase
|
|
|
What phase is under progesterone: growth of spiral arteries, increased blood supply, swelling of endometrium with increased secretory activity, accumulation of nutrients= ready for implantation/attachment?
|
secretory phase
|
|
|
What phase is it when blood vessels become vasospastic, necrosis of endometrium, desquamation, external bleeding= menstration?
|
luteolytic phase
|
|
|
What is the effect of estrogen on the uterus?
|
proliferation of endometrium, mucus
|
|
|
What is the effect of estrogen on the oviducts?
|
proliferation of glandular tissue and ciliated cells; increase of cilia activity
|
|
|
What is the effect of estrogen on the vulva/vagina?
|
hyperemia, swelling, mucous
|
|
|
What is the effect of estrogen on the mammary gland?
|
deposition of fat, proliferation of stroma and duct system
|
|
|
What is the effect of estrogen on the skeleton?
|
increased osteoblastic activity and mineralization
|
|
|
What is the effect of estrogen on metabolism?
|
slight increase in protein synthesis, increased fat deposition / subcutaneous tissue
|
|
|
What is the effect of estrogen on sexual behavior?
|
initiates sexual receptiveness
|
|
|
What is the effect of progesterone on the uterus?
|
stimulates secretory activity of endometrial glands, decreases myometrial activity = progesterone block
one of roles of progesterone is to suppress contraction on uterine smooth muscle; eventually this is antagonized by rising estrogen lvl. @ end of gestation |
|
|
What is progesterone block?
|
Suppression of contractility in uterine smooth muscle, which, often called the "progesterone block" on the myometrium. Toward the end of gestation, this myometrial-quieting effect is antagonized by rising levels of estrogens, thereby facilitating parturition.
|
|
|
What is the effect of progesterone on mammary gland?
|
development of mammary lobules and alveoli
|
|
|
What contols the female reproductive center, including search for partner, courtship display, and sexual receptivity, and is sitmulated by high levels sof estrogen (during estrous phase)
|
hypothalamic sex center
|
|
|
In what species does sex center require priming by low levels of progesterone?
|
cattle, pigs, sheep
|
|
|
What are volatile / non-volatile chemicals produced by genitals, urinary tissue, or sebacous glands as 'olfactory communicators' which can influence the estrous cycle and mating behavior?
|
phermones and estrous cycle
|
|
|
What adaption found in female small ruminants induces cycling after males join herd?
Purpose of this? |
whitten effect (sin heep, goat)
synchronizes females and advance breeding season? |
|
|
Give 2 examples pheromone effects used in animal production systems
|
Whitten effect:
Vandenbergh effect: |
|
|
Vandenbergh effect:
|
when gilts (female pig) reach puberty earlier when exposed to a boar -> used to advance onset of puberty in this species
|
|
|
for the establishment of pregnancy, maintenance of corpus luteum / progesterone is imperative, what must be avoided?
|
luteolysis
|
|
|
To avoid luteolysis (in most sp.) the conceptus has to interfere with what?
|
endometrial PGF2a release
|
|
|
What is the most important hormone to maintain pregnancy in all species?
|
progesterone
|
|
|
Where is progesterone produced?
|
corpus luteum / corpora lutea
|
|
|
At a later stage, what takes over progesterone production while the CL regresses?
Except in what species? |
placenta
not in pigs |
|
|
What are the functions of progesterone during pregnancy?
|
1. support of endometrium - to provide environment condusive to survival of preggers (maintains secretory activity / perfusion of endometrium)
2. decreases uterus tone, increases cervix tone (progesterone block) 3. prepares mammary gland during late pregnancy (also app. inhibit secretion of LH/FSH/GnRH -> prevent ovulation during pregnancy) |
|
|
What is the most important event initiating parturition, at end of pregnancy?
|
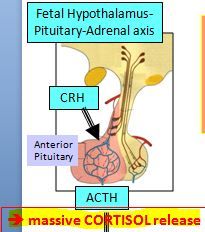
an INCREASE in fetal CORTISOL production, leading to progesterone withdrawal
|
|
|
What is cortisols target organ?
During parturition, cortisol stimulates 2 steroid hormone enzymes to convert what to what? |
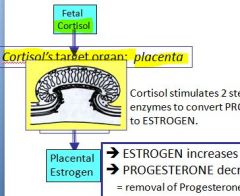
What is cortisols target organ? PLACENTA
During parturition stim. -> progesterone to estrogen |
|
|
What does conversion of estrogen to progesterone cause?
|
estrogen increases, progesterone decreases -> REMOVAL of the progesterone block
(remember this is occurring during parturition) |
|
|
Which of following is NOT a consequence of the estrogen increase after removal of the progesterone block (decr.progesterone)?
A. Number of gap junctions / myometrium increases -> single unit type smooth muscle (facilitates co-ordination of contractions) B. Stimulates synthesis of contractile proteins (actomyosin) C. Decreases number of oxytocin receptors D. Stimulates mucous secretions, stimulates synthesis of placental prostaglandin F2a/ E2 |
C. Not Decrease, there is INCREASE in oxytocin receptors
_______ Estrogen increase -> removal of block has what effects 1. Myometrium - Number of gap junctions / myometrium increases -> single unit type smooth muscle (facilitates co-ordination of contractions) - Induces an increase in oxytocin receptor numbers - stimulates synthesis of contractile proteins (actomyosin) --> prepares MYOMETRIUM (smooth muscle of uterus) to become CONTRACTILE stimulates mucous secretions, stimulates synthesis of placental prostaglandin F2a/ E2 |
|
|
What initiates regression of CL, leads to complete withdrawl of progesterone, assists in relaxing/dilating cervix, initiates intracellular contractions?
|
prostaglandin F2a/ E2
|
|
|
What is produced in some species by the CL, increases with PGF2a induced finala luteolysis ca. 10-14 hrs prior to birth, relaxes pelvic ligaments and muscles, separation of pelvic synthesis, facilitates expansion of birth canal?
|
relaxin
|
|
|
Are LH receptors on theca interna only? OR on granulosa cells also?
|
Don't know, but think both..at first only on Theca internal but read that FSH stimulates formation of LH receptors on Gr. cells too
(like maybe ahead of big surge) |
|
|
After regression of the CL, do FSH and LH increase OR decr.?
|
After luteolysis, FSH and LH secretion increases b/c of decrease in concentration of progesterone (made of by CL)
|
|
|
What effect does progesterone have on FSH, LH release?
|
decrease their release
|
|
|
Which hormone converts Testosterone to Estrogen?
|
neither, but FSH stimulates granulosa cells to do conversion :P
|
|
|
T/F Many of the follicles that undergo growth and maturation with each cycle never ovulate.
|
True
|
|
|
In large species, Stage 1 parturition, the fetus aquires the correct 'diving position' for delivery, what is this positioning?
|
anterior presentation
|
|
|
Stage II parturition: fetal membranes, legs, head, or buttocks push against and finally enter the cerivx, pressure receptors are stimulated to initiate what?
|
fergusson relflex / oxytocin release
|
|
|
Receptors initiated rhythmic myometrial contractions, and simultaneously abdominal muscles contract causing?
|
expulsion of the fetus
|
|
|
What is stage III parturition?
|
delivery of fetal membranes through sustained surges of PGF2a
|
|
|
What is the period of uterus involution and regeneration, attachment points of fetala membranes slough off, new epithelium forms = healing of endometrium, myometrium retracts = size reduction?
|
puerperium
|
|
|
During last days before parturition, prolactin is released to do what?
|
induce lactogenesis, induce maternal behavior
|
|
|
What are paired cutaneous gland, which provides nutrients to the newborn and consists of a secretory system and a duct system?
|
mammary gland
|
|
|
What is the milk secreting unit of the mammary gland, lined with a single layer of epithelial cells and surrounded by dense capillary network and myoepithelial cells
|
alveolus
|
|
|
Describe the mammary gland at birth.
|
gland present at birth, rudimentary duct system, parenchyma consistas of adipocytes and fibroblasts
|
|
|
During puberty, there is exponential growth during first estrous cycles of the mammary gland, what are the functions of estrogen and progesterone?
|
estrogen: lengthening and branching of ducts, progesterone: lobulo-alveolar development
|
|
|
The mammary gland becomes functional only during gestation, stroma is replaces with alveolar tissue b/o long standing what?
|
high estrogen/progesterone levels
|
|
|
The actual production of milk is lactogenesis, and only begins a few days befor parturition, called the what?
|
induction phase
|
|
|
Lactogenesis has what 2 distinct phases?
|
induction phase (before birth) and maintenance phase (p.p.)
|
|
|
Induction phase is coordinated with parturition, meaning it is induced by the same hormonal changes, such as:
|
withdrawl of progesterone prior to birth, increase in cortisol to induce prolactin receptors, increase in prolactin
|
|
|
The increase in prolactin a few days prior to birth is stimulated by prolactin RH and suppression of prolactin IH which is what?
|
dopamine
|
|
|
What does C.E.P.R.O. stand for?
|
The order of hormones in parturition: cortisol, estrogen, prostaglandin F2a, relaxin, oxytocin
|
|
|
T/F Fat tissue is a powerful endocrine/hormone producer.
|
True, e.g. leptin role in determining onset of puberty in female
|
|
|
zona pellucida forms first in what follicle/phase?
why is the z.p. important? |
zona pellucida 1st appears on secondary follicle
it has sperm binding sites (w/o sperm can't bind to ovum) |

