![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
111 Cards in this Set
- Front
- Back
Label.
|
|
|

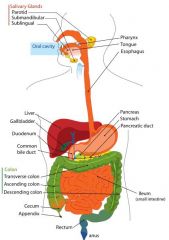
Label.
|
|
|

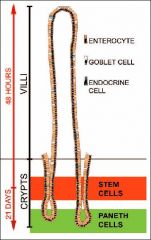
Label.
|

|
|

Put labels on right places.
|
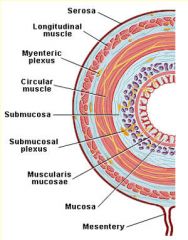
|
|
|
What does Musoca consist of? (3)
|
Epithelium, Lamina propria, Muscalaris mucosae (thin specialised muscle).
|
|
|
What does muscalaris externa consist of (2)?
|
Circular muscle and Longitudinal muscle.
|
|
|
Which part of the gastrointestinal system does not have villi in its structure?
|
Stomach.
|
|
|
What is the name of network of neurons that run in the structures of GT?
|
Submucosal plexus (Meissner's plexus - in small and large intestine);
Myentric plexus (Auerbach's plexus - extends from mouth to anus). |
|
|
Name cells that are laying in large intestine epithelia of the GT (5).
|
1. Absorptive cell
2. Goblet cell (mucous cell) 3.Microvacuolated columnar cell 4. Stem/progenitor cell 5. Enteric endocrine cell. |
|
|
Which membrane of cells is open to lumen of the intestine, apical or basolateral?
|
Apical.
|
|
|
Which membrane of cells has villi in it: apical or basolateral?
|
Apical.
|
|
|
Does water usually move across the intestinal epithelium using transcellular or paracellular pathway?
|
Paracellular.
|
|
|
If Cl- moves from interstitium to lumem of intestine, what fallows it?
|
Na+ follow negative charge of Cl- and water follows because of osmotic imbalance.
|
|
|
Name five major secretory tissues.
|
Salivary glands,
Gastric glands, Exocrine pancreas, Liver-biliary system, Intestin. |
|
|
Describe endocrine regulatory mechanism.
|
Release of a transmitter (e.g. hormones: gastrin, CCK, secretin) into blood for delivery to distant target cell.
|
|
|
Describe paracrine regulatory mechanism.
|
Release of a transmitter (e.g.somatostatin) from a sensor cell to affect adjacent target cells without entering blood or activating neurons. Short distance affect of paracrines, they act locally, within the same tissue that secretes them.
|
|
|
Describe neuronal regulatory mechanism.
|
Electrical signalling via neurons. Via extrinsic and intrinsic regulation.
|
|
|
What are neurocrines?
|
Peptides that are synthesised in neurones of the GT and released following AP (e.g. ACh, GRP, norepineohrine, VIP, substance P).
|
|
|
What is the site of secretion of the following hormones: Gastrin, CCK, Secretin, GIP?
|
Gastrin - G cells of the stomach;
CCK - I cells of the duodenum and jejunum; Secretin - S cells of the duodenum; GIP - K cells in duodenum and jejunum. |
|
|
What are stimuli for secretion of the following hormones: Gastrin, CCK, Secretin, GIP?
|
Gastrin - small peptides and amino acids, distention of the stomach, vagal stimulation (GRP);
CCK - Small peptides and amino acids, fatty acids; Secretin - H+ in the duodenum, fatty acids in the duodenum; GIP - fatty acids, amino acids, oral glucose. |
|
|
What are actions of Gastrin? (2)
|
Increase H+ secretion, stimulating growth of gastric mucosa.
|
|
|
What are actions of CCK? (5)
|
Increase in pancreatic enzyme secretion;
Increase in pancreatic HCO3- secretion; Stimulating contraction of gallbladder and relaxation of the spincter of Oddi; Stimulating growth of exocrine pancreas and gallbladder; Inhibition of gastric emptying. |
|
|
What are actions of Secretin? (4)
|
Increase in pancreatic HCO3- secretion;
Increase in biliary HCO- secretion; Decrease in gastric H+ secretion; Inhibition of trophic effect of gastrin on gastric mucosa. |
|
|
What are actions of GIP? (2)
|
Increase in insulin secretion from pancreatic beta cells;
Decrease in H+ secretion. |
|

Fill in the table using offered answers.
|

|
|
|
Which hormone inhibits gastric secretion and stimulates insulin release?
|
GIP
|
|
|
Which hormone stimulates growth of mucosa (of enterochromaffin-like cells)?
|
Gastrin.
|
|
|
Which hormone stimulates gallbladder contraction, pancreatic secretion?
|
CCK.
|
|
|
Which plexus lies between submucosa and the circular muscle?
|
Submucosal plexus (Meissner's plexus).
|
|
|
Which plexus lies between the circular muscle and the longitudinal muscle?
|
Myenteric plexus.
|
|
|
Innervation of GT is regulated by which two NS, which are part of ANS?
|
Extrinsic NS (long reflexes) - sympathetic and parasympathetic innervation;
Intrinsic NS (short reflexes) - enteric NS. |
|

Put in names of transmitters.
|

|
|
|
Name two inhibitory transmitters of intrinsic NS.
|
VIP and NO.
|
|
|
Name two excitatory transmitters of intrinsic NS.
|
ACh and substance P.
|
|
|
Name three phases of gastrointestinal control.
|
1. Cephalic phase -sight, smell, taste and chewing;
2. Gastric phase - distension, acidity, etc.; 3. Intestinal phase - distension, acidity, osmolarity, etc. |
|
|
Name three functions of motor activity of GI tract.
|
Non-propulsive movements (Effectively mixes chyme and brings fresh chyme into contact with the mucosal surface);
Peristaltic movements (Propels chyme for a short distance); Reservoir function. |
|
|
Name Two types of muscle contractions.
|
Phasic and tonic.
|
|
|
What are slow waves?
|
Slow waves are not action potentials, but rather oscillating (колеблющийся) depolarization and repolarization of membrane potential of the smooth muscle cells.
|
|
|
Fill in blanks about the electric activity in the smooth muscle in the GI tract:
The frequency of ___ ___ sets the frequency of ___ ___ and, therefore, sets the frequency of ____. ___ ___ cannot occur unless the ___ ___ brings the membrane potential to threshold. |
The frequency of slow waves sets the frequency of action potentials and, therefore, sets the frequency of contractions. Action potential cannot occur unless the slow wave brings the membrane potential to threshold.
|
|
|
Where do slow waves originate?
|
In interstitial cells of Cajal.
|
|
|
What causes the depolarization of membrane potential of slow wave in GI tract cells?
|
Cyclic opening of Ca++ channels.
|
|
|
What causes the repolarization of membrane potential of slow wave in GI tract cells?
|
Opening of Potassium channels.
|
|
|
Name three components of gastric motility.
|
1. Relaxation of the orad region of the stomach to receive the food bolus from the esophagus;
2. contractions that reduce the size of the bolus and mix it with gastric secretions to initiate digestion; 3. Gastric emptying that propels chyme into the small intestine. |
|
|
Name three anatomic divisions of the stomach.
|
The fundus, the body and the antrum.
|
|
|
Name two pats of the stomach, based on differences in motility.
|
Orad and caudad.
|
|
|
What are migrating motor complexes?
|
During fasting, there are periodic contractions, that occur at 90-min intervals and function to clear the stomach of any residue remaining from the previous meal.
|
|
|
What are spincters?
|
Specialised circular muscles that separate two adjacent compartments of the GI tract. They effectively serve as one-way valves.
|
|

Label.
|

|
|
|
What are the components of saliva?
|
Mucin glycoproteins, lysozyme,
lipase, proline-rich proteins, alpha-amylase. |
|
|
Name three functions of saliva.
|
1. Lubricate the food to make swallowing easier - mucin glycoproteins, water;
2. Clean and protect the cavity of the mouth - lysozyme, proline-rich proteins; 3. Reduce starch to oligosaccharide molecules - alpha-amylase. |
|
|
Name three major salivary glands.
|
Parotid glands, submandibular glands and the sublingual glands.
|
|
|
What does acinus of salivary gland soncist of?
|
It is lined with acinar cells and in the middle of it there is intercalated duct.
|
|
|
What do acinar cells produce?
|
They produce initial saliva composed of water, ions (Na, K, Cl, HCO3), enzymes and mucus, which is isotonic to plasma.
|
|
|
What do ductal cells of salivary glands do?
|
They modify the initial saliva to produce the final saliva by altering the concentrations of various electrolytes. Secretion of K+ and HCO3- and reabsorbing Na+ and CL-. So saliva is hypotonic to plasma after going through ductal cells, it has less Na+ and CL-.
|
|
|
Compare saliva and plasma osmolarity.
|
Saliva is hypotonic to plasma, has lower osmolarity. It has higher K+ and HCO3- concentrations, but lower Na+ and Cl-.
|
|
|
Acinar cells of salivary glands are often called leaky epithelia, and duct-lining epithelial cells are called tight epithelia. Why?
|
Because acinar cells allows Na and water to move between them, but in duct cells secretion and reabsorption happens only through individual epithelial cells, nothing can move between the cells.
|
|
|
Describe effect of flow rate on composition of saliva.
|
The ionic composition of saliva changes with flow rate. Faster is flow rate, more closely is the composition of saliva to plasma or initial saliva. Low flow rates - low concentrations of Na and Cl, high flow rates - duct cells are not able to reabsorb these ions and their concentration remains high. Concentration of HCO3 and K do not change.
|
|
|
Which hormones regulate saliva secretion in the mouth?
|
There is no control by peptide hormones of excretion of saliva.
|
|
|
Which NS increases salivary secretions - SNS or PNS?
|
Both, but PNS has stronger effect and long-lasting.
|
|
|
What is the effect of ACh in salivary glands?
|
It decreases NaCl reabsorption.
|
|
|
What is the effect of Noradrenaline in salivary glands?
|
It stimulates HCO3- secretion.
|
|
|
What is the effect of aldosterone in work of salivary glands?
|
Aldosterone stimulates NaCl reabsorption and K+ secretion.
|
|
|
How much of saliva is secreted every day?
|
About 1 - 1.5 L per day.
|
|
|
Name three phases of swallowing.
|
1. Oral phase. Voluntarily.
2. Pharyngeal phase 3. Oesophageal phase (start of peristalsis). |
|
|
What is peristalsis?
|
Sequential contraction of ring of muscle.
|
|
|
What is receptive relaxation?
|
Part of swallowing process - relaxation of the fundus of the stomach when food enters it.
|
|
|
When does secondary peristalis occur?
|
It occurs if after primary peristalis there is still food left in the oesophagus after lower oesophageal spincter is closed.
|
|
|
Describe coordination of spincter activity during swallowing.
|
When UES is open, LES is closed. And when LES opens, UES is closed.
|
|
|
What coordinates vomiting reflex?
|
Vomiting center in the medulla.
|
|
|
Name 6 events of vomiting reflex in temporal sequence.
|
1. Reverse peristalisthat begins in the small intestine
2. relaxation of the stomach and pyrolus 3. Forced inspiration to increase abdominal pressure 4. relaxation of the lower esophageal spincter 5. forceful expulsion of gastric contents 6. reflex relaxation of the upper oesophagus spincter and vomiting. |
|

Fill in which substances and where are being secreted in the stomach.
|

|
|
|
What secretes gastric juice?
|
Gastric mucosa.
|
|
|
What are four major components of gastric juice?
|
HCl, pepsinogen, mucus, intrinsic factor.
|
|
|
Which substances of gastric juice initiate the process of protein digestion?
|
HCl and pepsinogen.
|
|
|
What is the major role of intrinsic factor?
|
It is required for absorption of vitamin B12.
|
|
|
What is the only essential component of gastric juice?
|
Intrinsic factor.
|
|
|
The body of stomach contains two types of glands. Which ones?
|
Oxyntic and Pyloric.
|
|
|
Which cells secrete HCl and intrinsic factor?
|
Pariental cells.
|
|
|
What do pariental cells secrete?
|
HCl and intrinsic factor.
|
|
|
Which cells in stomach secrete pepsinogen?
|
Chief cells.
|
|
|
Which stomach cells secrete Gastrin to circulation?
|
G cells.
|
|
|
Where to do G cells secrete gastrin?
|
Into the circulation.
|
|
|
To what level of pH does HCl acidifies gastric contents?
|
pH between 1 and 2.
|
|
|
What is the function of HCl in the stomach?
|
It acidifies gastric contents. This is to convert inactive pepsinogen to its active form, pepsin, a protease that begins the process of protein digestion.
|
|
|
Name 4 functions of HCl.
|
1. Promotes the activation of pepsins; provides optimal environment for the action of pepsins;
2. Kills or inhibits microorganisms; 3. Stimulates secretions in the small intestine; 4. Helps iron and calcium absorption in the small intestine. |
|
|
What enzyme catalyzes in formation of H2CO3 from CO2 and water inside gastric pariental cells?
|
Carbonic anhydrase.
|
|
|
After dissociation of H2CO3 to H+ and HCO3- in the gastric pariental cells what happens with end products?
|
H+ is secreted to lumen of the stomach and HCO3- is absorbed into the blood.
|
|
|
In the pariental cells, how is H+ transported to the lumen of the stomach?
|
Via H+-K+ATPase.
|
|
|
In pariental cells of the stomach, how is Cl- transported to the lumen of the stomach?
|
Diffusing through Cl- channels. Passive process.
|
|
|
How do Cl- ions get to pariental cell of the stomach?
|
The Cl- ions enter the cell across the basolateral membrane via the Cl-/HCO3- exchanger. No energy of ATP required.
|
|
|
Which channels for ion transport do apical membrane of pariental cell in the stomach has?
|
Cl- gated ion channel;
H+/K+ ATPase; K+ gated ion channel. |
|
|
Which ion channels does basolateral membrane of pariental cells of a stomach have?
|
Na+/K+ ATPase;
Cl-/HCO3- exchanger; K+ gated ion channel. |
|
|
In pariental cells of the stomach how does HCO3- is absorbed from the cell to the blood?
|
Through Cl-/HCO3- exchanger in basolateral membrane.
|
|
|
What effect does HCO3- absorbed from pariental cells of a stomach has on blood?
|
The effect is called 'alkaline tide', means high pH of the blood.
|
|
|
What will happen with HCO3- absorbed by blood from pariental cells of the stomach?
|
Eventually, it will be secreted back into the gastrointestinal tract in pancreatic secretions.
|
|
|
In summary, what happens in apical and basolateral membrane of pariental cells in the stomach?
|
Net secretion of HCl and net reabsorbtion of HCO3-.
|
|
|
What is the function of intrinsic factor?
|
It combines with vitamin B12 to resist digestion by pancreatic proteases (digestive enzymes secreted by the pancreas to break down proteins), it facilitates absorption of vitamin B12 in the ileum.
|
|
|
What is the function of pepsins?
|
They digest proteins.
|
|
|
What environment is needed for pepsinogens to activate to pepsins?
|
Very acidic (< or = 3 pH).
|
|
|
Is the HCl needed for activity of pepsins (apart from activation of pepsinogen)?
|
Yes.
|
|
|
Why don’t HCl and pepsins damage the gastric mucosa?
|
Because walls of a stomach are covered with gastric mucosal barrier.
|
|
|
What are three protective components of gastric mucosal barrier?
|
1. A compact epithelial cell lining, with very tight junctions that do not let the acid go through.
2. A special mucus covering, that holds HCO3 close to the epithelial cells. 3. Secretion of bicarbonate ions that in the lumen act to neutralize harsh acids. It combines with H+ and becomes H2CO3 and Water and CO2 later on. |
|
|
Which substances inhibit HCO3- secretion by epithelial cells of stomach?
|
Aspirin, Adrenaline, noradrenaline.
|
|
|
Name three phases of Gastrointestinal control.
|
1.Cephalic phase (smell, sight, taste and chewing);
2. Gastric phase (distension, acidity); 3. Intestinal phase (distension, acidity, osmolarity). |
|
|
Describe control of gastric secretion in gastrointestinal Cephalic phase (1).
|
The control is entirely dependent on vagal nerve. Stimulation via:
- direct effect on pariental cells - indirect effect on ECL cell - indirect effect on G cells. Stimulation is also effected by inhibiting the secretion of somatostatin by D cells. |
|
|
Describe control of gastric secretion in gastric (2) phase of gastrointestinal control.
|
Controlled by local and vagovagal reflexes and hormones.
The stimuli for secretion are distension of the stomach, presence of break-down products of protein, amino acids and small peptides. - Distension causes direct vagal stimulation of periental cells and - indirect stimulation of the pariental cells via gastrin release from G cells. - Distension of antum results in local reflexes and stimulates gastrin release. - Alcohol and caffeine also stimulate gastric secretion. |
|
|
What effect do tonic contractions of the stomach have?
|
It controls the emptying of food into the duodenum.
|
|
|
What does tonic contraction of pyloric spincter control?
|
The speed of stomach emptying.
|
|
|
What is the driving force of gastric emptying?
|
Pressure difference between the lumen of stomach and duodenum.
|
|
|
Which of the following would have the fastest rate of emptying from the stomach: liver/glucose?
|
Glucose --> liver.
|
|
|
What is the amplitude of slow waves of smooth muscle?
|
5 to 15 mV
|

