![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
76 Cards in this Set
- Front
- Back
|
How many percent of the Cardiomyocytes in the myocardium possess the ability to generate electrical impulses (or action potentials)?
|
One.
|
|
|
What is SA node?
|
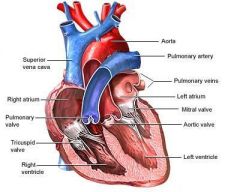
Sinoatrial node is responsible for atrial propagation of action potential. is a group of cells positioned on the wall of the right atrium, near the entrance of the superior vena cava. These cells are modified cardiomyocyte. They possess rudimentary contractile filaments, but contract relatively weakly.
|
|
|
Why SA node is called Primary pacemaker?
|
Because SA node generates AP more often than other pacemakers of the heart and is responsible for the rest of the heart's electrical activity, it is sometimes called the primary pacemaker.The reason the SA node controls the whole heart is that its action potentials are released most often to the heart's muscle cells; this will produce contraction. The action potential generated by the SA node passes down the cardiac conduction system, and arrives before the other cells have had a chance to generate their own spontaneous action potential. This is the electrical conduction system of the heart|normal conduction of electrical activity within the heart.
|
|
|
What is secondary pacemaker?
|
Atria-ventricular node. The cells of the AV node normally discharge at about 40-60 beats per minute. Because the SA node fires more often, it takes over the AV node, and it fires in the same speed as SA node. But if the SA node stop working, AV node takes over and that's why it is secondary pacemaker.
|
|
|
What is bundle of His?
|
Further down the electrical conducting system of the heart after the SA and AV nodes is the Bundle of His. The left and right branches of this bundle, and the Purkinje fibres, will produce a spontaneous action potential at a rate of 30-40 beats per minute, if the SA and AV node both do not function.
|
|
|
What are the main ion channels that are involved in pacemeaker cell action potentials?
|
Funny channels (If channels, Na), T-type Ca channels, L-type Ca channels, Ca dependent K channels (Vk channels).
|
|
|
Why are the funny channels so special to cardiac muscle AP?
|
Because they are responsible for the cardiac pacemaker activity, they open and close periodically without any external help.
|
|
|
Give a normal range of SV, HR and CO.
|
Normal HR is 70 b/min, SV is 70 ml/min, CO = SVxHR = 4,9 l/min.
|
|
|
What can increase preload?
|
Slow heart rate and exercise.
|
|
|
What can decrease preload?
|
Fast heart rate and blood loss.
|
|
|
What can increase contractility of the heart?
|
Calcium, hormones, SNS
|
|
|
What can increase afterload?
|
Hight hematocrit, stenosis of vessels, hight blood pressure, constricted blood vessels, lipids in blood which thickens the blood, too much fluid in the body.
|
|
|
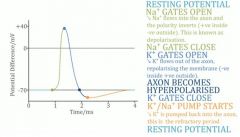
Why is the inside of the cell negative relatively to the outside of the cell?
|
Because of the constant work of the Na-K-ATPase, which pumps 3 Na ions out of the cell and only 2K ions into the cell, so more positive charge is concentrated outside than inside.
|
|
|
Describe voltage-gated ion channels.
|
VG ion channels have a positive charged gate that slides in response to the membrane voltage. If the inside is negative, it holds the gate closed, at less negative membrane voltages, the gate slides out and the channel is open. Different ion channels open in different voltages.
|
|
|
Name the approximate voltages on which Na, Ca and K channels open during AP?
|
Around -55mV for Na, then -40mV for Ca, and +30mV for K.
|
|
|
What ions repolarises the membrane and which depolarises during AP?
|
Na depolarises the membrane and K ions repolarises it.
|
|
|
How does the pacemeaker cell action potential graph look like?
|
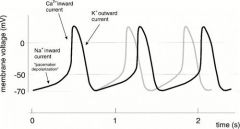
|
|
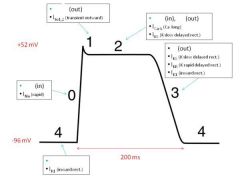
Put in the names of the ions which are involved in different stages of the action potential in the cardiac muscle (K, Ca, Cl, Na).
|
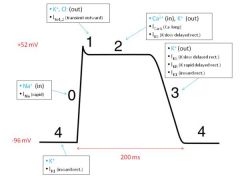
|
|
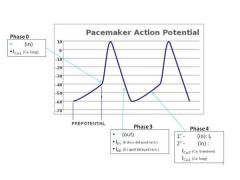
Add the ion names to the corresponding places in the graph of the cardiac pacemeaker action potential.
|
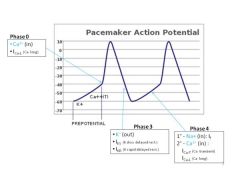
|
|
|
What effect does Epinephrine and norepinephrine have on pacemaker cells?
|
It binds to beta receptors on the surface of the pacemaker cells and results in more often firing of the action potentials - therefore more rapid heart rate.
|
|
|
How exactly does PNS slow heart rate?
|
It releases ACh onto muscarinic receptors in the surface of the pacemeker cells in the heart, that changes permiability of (Na and Ca) ion channels, and it decreases rate of firing of the AP.
|
|
|
How does AP travel from the pacemaker cells to the cardiac muscle cells?
|
Through the gap junctions between the cells.
|
|
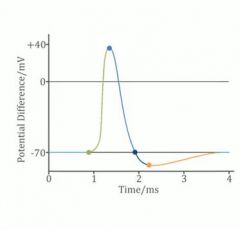
Explain the graph of action potential in the usual neurone cell.
|
|
|

Fill in blanks.
|

|
|
|
Is it right to say that the main role of the atrial is to fill the ventricles with blood?
|
No, because most of the blood is transferred from atria to ventricles passively. So the main role of the atria is to store blood.
|
|
|
By which three things is the blood pressure controlled?
|
Stroke volume, peripheral resistance, heart rate.
|
|
|
What is the difference between SV and CO?
|
CO is the amount of blood pumped out of the ventricle per minute, but SV is the amount of blood pumped out of the ventricle per each beat. CO=HRxSV
|
|
|
What is the name of the body regulation of the width of the blood vessels?
|
The ability to regulate the width of the blood vessels is called the peripheral resistance.
|
|
|
Where in the vasculature is the highest resistance to blood flow?
|
Most of the resistance to blood flow in the circulation occurs in the small-diameter arteries called arterioles.
|
|
|
Group of hormones called the renin-angiotensin-aldosterone system (RAAS) is critical player in blood pressure control. What do they do?
|
They regulate the amount of fluid in the blood, the width of the blood vessel, and the sodium and water balance by their action on the kidneys and blood vessels.
|
|
|
Explain the systolic blood pressure.
|
When the ventricles contract, blood is pumped out of the left ventricle into the main artery leading away from the heart to the body, called the aorta. This creates the highest pressure that occurs in the aorta, called the systolic blood pressure.
|
|
|
Explain diastolic blood pressure.
|
When the ventricles relax, blood stops flowing into the aorta and the pressure drops to its lowest level. This is called the diastolic blood pressure.
|
|
|
What type of pressure is blood pressure?
|
Blood pressure is a hydrostatic pressure.
|
|
|
What's Percy's law of flow?
|
Flow=pressure drop/resistance.
|
|
|
Which vessels are called resistance vessels?
|
Terminal arteries and arterioles.
|
|
|
Vascular wall comprises three layers. Name them.
|
Tunica intima (endothelium);
tunica media (vasc.smooth muscle, collagen, elastin); tunica externa (connective tissue). |
|
|
How large is the EDV?
|
About 120 ml.
|
|
|
Name the components of the blood.
|
Plasma (ab 3L out of 5, mainly consists of water, contains electrolytes, glucose, proteins, etc.);
buffy coat - white cells; red blood cells (ab.40%). |
|
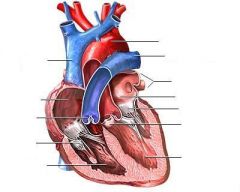
Label the diagram.
|
|
|
|
Can tetanus occur in cardiac muscle?
|
No.
|
|
|
Appr.how long are the AP in skeletal and cardiac muscle?
|
Cardiac - 200ms, skeletal - 5ms.
|
|
|
Why it is important to have a plateau phase in cardiac AP cycle?
|
Because while depolorised heart cannot be activated again (refractory period), so it protects the heart muscle from tetanus, which would be lethal.
|
|
|
Pacemaker cells lack _____ channels, and the AP is produced by ____ channels.
|
Pacemaker cells lack voltage-gated Na+ channels, and the AP is produced by Ca++ channels.
|
|
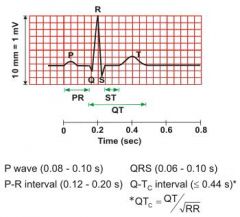
ECG. What happens in the heart in the time of:
P-wave; P-R interval; QRS complex; T-wave; QT interval. |
P-wave: Atrial depolarisation;
P-R interval: Delay at AV node +Bundle of His; QRS complex: Ventricular depolarisation; T-wave: Ventricular repolarisation; QT interval: Ventricular AP duration. |
|
|
Name two types of regulation of CO.
|
Intrinsic mechanisms: Frank-Starling's law of the heart, Importance of central venous pressure, Influence of arterial pressure;
Extrinsic mechanisms: sympathetic control of contractility. |
|
|
Which pressure is often considered as central venous pressure?
|
Pressure in the right atrium.
|
|
|
What is the name of the heart's ability to contract independent of preload or afterload?
|
Contractility.
|
|
|
What is the increase in contractility?
|
A change in the ability of cardiac muscle to generate force without a change in fibre length. Positive inotropy (contractility).
|
|
|
What is the name of increase in rate of relaxation of heart muscles?
|
Positive lusitrophy.
|
|
|
How does the positive inotropy occurs?
|
(Generating more force without changing the length of the muscle). Increased myocardic contractility happens by increasing the Ca++ uptake by cardiomyocytes.
|
|
|
How is it possible to estimate the CO using the Fick principle?
|
Q=V(oxygen)/(Ca-Cv).
Where: Q - cardiac output V - rate of oxygen uptake Ca - concentration of oxygen in arterial blood Cv - concentration of oxygen in venous blood |
|
|
How is it possible to estimate the CO?
|
The Fick principle
Indicator dilution Pulsed Doppler method. |
|
|
What prevents back-blood flow in veins?
|
Semi-lunar valves.
|
|
|
What is vascular tone?
|
The degree of vasodilatation/vasoconstriction of a vessel.
|
|
|
What is called aoutoregulation or Bayliss myogenic response?
|
The Bayliss effect in vascular smooth muscles cells is a response to stretch. This is especially relevant in arterioles of the body. When blood pressure is increased in the blood vessels and the blood vessels distend, they react with a constriction; this is the Bayliss effect. Stretch of the muscle membrane opens a stretch-activated ion channel. The cells then become depolarized and this results in a Ca2+ signal and triggers muscle contraction. No action potential is necessary here; the level of entered calcium affects the level of contraction proportionally and causes tonic contraction.
|
|
|
What is the other name for metabolic hyperaemia?
|
Active hyperaemia.
|
|
|
Name the examples of vasodilatatory metabolites.
|
K+ ions, CO2, adenosine, hypoxia (redused O2 levels in tissue).
|
|
|
What is reactive hyperaemia?
|
It is the increase of the blood flow that occurs following a brief period of ischaemia.
|
|
|
What is ischaemia?
|
An occlusion of blood flow to the tissue resulting in depletion of nutrients, oxygen, a built up of CO2.
|
|
|
What is the formula of CO which includes CVP?
|
CO=(MABP-CVP)/TPR
Cardiac output = (Mean arterrial blood pressure-Central venous pressure)/Total peripheral resistance. |
|
|
Why the blood flow within aorta is pulsatile?
|
Because of the rhythmic pumping action of the heart.
|
|
|
How large is the atmospheric pressure?
|
1 atm = 760mmHg.
|
|
|
Name three types of capillaries and state how they differ.
|
Continuous - made of one cell layer, tight junctions - big molecules cannot get through;
Fenestrated - have fenestrated walls, big molecules can go through; Discontinuous - have gaps between cells that are so big, that can let other cells pass through (e.g.bone marrow). |
|
|
State Fick law of diffusion.
|
Js =PS(Ccap-Ci),
Js - metabolite flux (moles/min) P - permiability coefficient S - surface area Ccap - capillary concentration (moles/l) Ci - interstitial concentration (moles/l). |
|
|
What is ultrafiltration?
|
Arteriolar pressure pushes water through the capillary walls. this is distinct from diffusion. Pi is slightly negative to the atmospheric pressure.
|
|
|
What is colloid osmotic pressure?
|
The osmotic pressure made by proteins (across capillary wall: it cannot let proteins diffuse fast, so they built up COP).
|
|
|
Name the Starlings forces involved in water movement across the capillary wall.
|
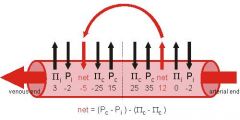
Capillary pressure and interstitial pressure, colloid osmotic pressure of the interstitium, colloid osmotic pressure of the plasma.
|
|
|
Give the formula of starling principle of movement of water across capillary bed.
|
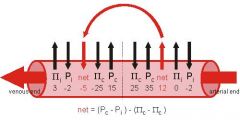
Net rate of fluid movement = hydraulic conductance x surface area ((hydraulic drive)-(osmotic drive)).
|
|
|
What is oedema?
|
Oedema is an abnormal accumulation of fluid beneath the skin or in one or more cavities of the body
|
|
|
What are the causes of oedema?
|
Oedema may arise when the fluid production by capillaries is higher than fluid removal by the lymphatics.
|
|
|
What does reflection coefficient mean?
|
The permeability of the membrane. If the RC is 0 - the membrane is totally permeable, 1 - totally impermeable.
|
|
|
What do baroreceptors sense?
|
Baroreceptors are mechanoreceptors, they sense stretch. So respond to the blood pressure.
|
|
|
What is the short-term control of the blood pressure?
|
Baroreceptor denervation.
|
|
|
Describe work of RAS.
|
The renin-angiotensin system (RAS) or the renin-angiotensin-aldosterone system (RAAS) is a hormone system that regulates blood pressure and water (fluid) balance.
When blood volume is low, juxtaglomerular cells in the kidneys secrete renin. Renin stimulates the production of angiotensin I, which is then converted to angiotensin II. Angiotensin II causes blood vessels to constrict, resulting in increased blood pressure. Angiotensin II also stimulates the secretion of the hormone aldosterone from the adrenal cortex. Aldosterone causes the tubules of the kidneys to increase the reabsorption of sodium and water into the blood. This increases the volume of fluid in the body, which also increases blood pressure. |
|
|
Describe work of pressure regulation by RAAS. Include blood pressure receptors, enzymes, effector organs.
|
In the kidneys specialized smooth muscle cells of the afferent arteriole, called granular juxtaglomerular (JG) cells, are mechanoreceptors that monitor blood pressure in the afferent arteriole. In the adjacent distal convoluted tubule, specialized cells, called macula densa, are chemoreceptors that monitor the concentration of Na+ and Cl− in the urine inside the tubule. If these receptors sense low blood pressure and low concentration of Na, Cl (that means that glomerular filtration is too slow and too much NaCl is reabsorbed), they result in Renin release from the JG cells. Renin converts angiotensinogen (a plasma protein produced by the liver) to angiotensinogen I. Angiotensinogen I, in turn, is converted to angiotensinogen II by angiotensin converting enzyme (ACE), an enzyme produced principally by capillary endothelium in the lungs. Angiotensinogen II circulates in the blood and increases GFR by
- constricting blood vessels throughout the body, causing the blood pressure to rise, - constricting the afferent arterioles, and - stimulating the adrenal cortex to secrete aldosterone, a hormone that increases blood pressure by decreasing water output by the kidneys. Also angiotensin II will affect on the hypothalamus and the ADH will be released, what will result in increased water reabsorbtion in the kidney. Next angiotensin II stimulates SNS which results in vasoconstriction of the arteries. Also angiotensin II has an effect to the thirst center, so the feeling of thirst will increase. |
|
|
Name the affects of the angiotensin II.
|
It works as a vasoconstrictor, works as enzyme for release of aldosterone and ADH (vasopresin).
|

