![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
76 Cards in this Set
- Front
- Back
|
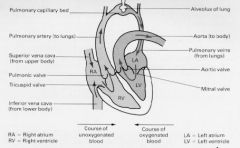
What are the valves present in the left part of the heart?
|
Mitral valve, Aortic valve.
|
|
|
What are the valves present in the right part of the heart?
|
Tricuspid valve, pulmonic valve.
|
|
|
What is the name of the largest vein?
|
Vena cava.
|
|
|
Name three types of tissue present in the walls of arteries.
|
Connective tissue, smooth muscle and elastic tissue.
|
|
|
Name the site of the highest resistance to blood flow in vasculature.
|
Arterioles.
|
|
|
In arterioles the resistance is often changed by alternations in what?
|
In sympathetic nerve activity, by circulating vasoactive substances.
|
|
|
Describe structure of veins and venules.
|
The walls of venules are thin, veins - have endothelial cell layer, modest amount of elastic tissue, smooth muscle and connective tissue.
|
|
|
Why veins are more capable to hold blood that arterioles?
|
Because there is less elastic tissue in veins than there is in arteries.
|
|
|
What is unstressed volume?
|
Volume of blood contained in the veins.
|
|
|
Name the relationship between blood flow, velocity and cross-sectional area of the the blood vessels.
|
v=Q/A
v - velocity of blood flow (cm/sec) Q - blood flow (ml/sec) A - cross- sectional area (cm2) A is calculated as A=πr2 |
|
|
What is the driving force for the blood flow?
|
The pressure difference between the two ends of a vessel.
|
|
|
Name the relationships between blood flow, resistance and pressure.
|
Q=(P1-P2)/R:
Q - blood flow (ml/min) P - pressure (mmHg) R - resistance (mmHg/ml/min) |
|
|
How is it possible to change resistance in blood vessels?
|
Change the radius of the vessels.
|
|
|
What is the major mechanism for changing the blood flow in the cardiovascular system?
|
Changing the resistance of blood vessels, particularly arterioles.
|
|
|
What is TPR and how can it be calculated?
|
Total peripheral resistance, the resistance of entire systemic vasculature. R = (P1-P2)/Q, where R is resistance, P1 is the pressure in the aorta, P2 is the pressure in vena cava, Q - cardiac output.
|
|
|
Name the Poiseuille equation for resistance of a blood vessels to the blood flow.
|
R=8ηl/πr4:
R - resistance η - viscosity of the blood l - length of blood vessel r - radius of blood vessel |
|
|
In laminar blood flow what is the velocity of blood at the vessel wall and what is it in the center?
|
The stream is maximal at the center and zero at the wall.
|
|
|
Name two types of blood flow?
|
Laminar and turbulent.
|
|
|
What is turbulent blood flow is accompanied with?
|
With audible vibrations called murmurs.
|
|
|
What is considered a predictor of blood turbulence?
|
Reynolds number, which considers blood viscosity, blood velocity and diameter of a blood vessel.
|
|
|
What is a compliance of a blood vessel?
|
Compliance of a blood vessel describes the volume of blood the vessel can hold at a given pressure. It is related to distensibility
|
|
|
What does the compliance of a blood vessel depend on? And what is the equation of it?
|
On the distensibility (rastjazhimostj) and is given by the following equation:
C=V/P, where C - compliance (ml/mmHg); V- volume (ml); P - pressure (mmHg). |
|
|
Compare compliance of veins and arteries (volumes, pressures).
|
Compliance of veins is higher than that of the arteries, in other words, veins hold large volumes of blood in a low pressures, arteries hold much less blood, and they do it at high pressure.
|
|
|
What is the mean pressure in the aorta?
|
100 mmHg
|
|
|
Why is the pressure in the aorta so high?
|
Because of the low compliance of the aorta and the big amount of blood pumped from the heart. the given volume causes greater pressure when compliance of the vessel is low.
|
|
|
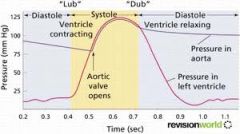
What is the diastolic pressure?
|
The lowest arterial pressure measured during a cardiac cycle and is the pressure in the artery during ventricular relaxation when no blood is being ejected to the left ventricle.
|
|
|
What is systolic pressure?
|
The highest arterial pressure measured during a cardiac cycle, the pressure in the artery after the blood has been ejected from the left ventricle during systole.
|
|
|
What is pulse pressure?
|
It is the difference between the systolic and diastolic pressures.
|
|
|
What is stroke volume?
|
The volume of the blood ejected from the left ventricle on a single beat.
|
|
|
What is a mean arterial pressure, and how is it calculated?
|
It is average pressure in a complete cardiac cycle and is calculated as follows:
MAP= DP+1/3PP. MABP = CO x TPR |
|
|
Name functions of cardiovascular system.
|
- Rapid connective transport
- Control system (hormones) - Body temperature regulation - Reproduction - erection. |
|
|
What is cardiac output?
|
CA is the volume of blood ejected by one ventricle in one minute. CA is the result of stroke volume and heart rate.
|
|
|
What is the difference between the blood flow and flow velocity?
|
Blood flow is how much blood is flowing per min, but flow velocity is how fast it is flowing.
|
|
|
There are 2 blood vessels with the same diameter, but different pressure gradients on both ends: first - 150-120mmHg, second - 90-40mmHg. Which blood vessel has more blood flowing through it per minute (where blood flow rate is higher)?
|
The second blood vessel, because the pressure gradient is higher - 50mmHg (30 in first blood vessel). Blood flow = pressure gradient/resistance.
|
|
|
What is the relationships between the blood vessel resistance and blood vessel radius?
|
R=1/r4.
|
|
|
What happens with flow velocity if the blood vessel radius decreases?
|
The velocity increases, because Flow velocity = Blood flow/Total crossectiolal area.
|
|
|
How does active tissue increase blood supply to it?
|
Active tissue releases metabolites to the blood and that dilates the blood vessels, bringing more blood to it.
|
|
|
What is metabolic hyperaemia?
|
Increased blood flow in the result of increased metabolic activity to the tissue.
|
|
|
Which organ in our body receive constant blood supply no matter if it the body is at rest or if it is exercising?
|
Brain.
|
|
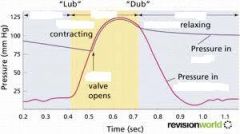
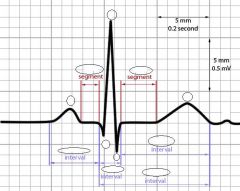
Fill in blanks and explain the picture.
|
|
|

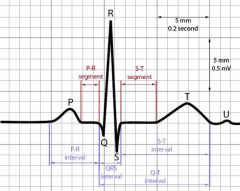
Fill in blanks and explain the picture.
|
|
|
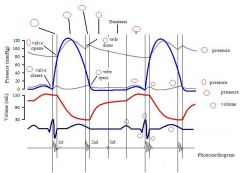
Fill in blanks and explain the picture.
|
|
|

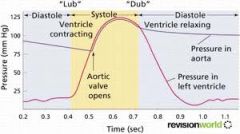
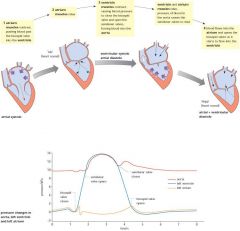
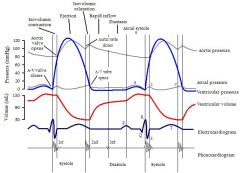
Label and explain.
|

|
|

Label and explain.
|

|
|

Label and explain.
|
|
|
Label and explain.
|
|
|
Label and explain.
|
|
|
Label and explain.
|
|
|
|
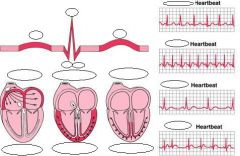
What is isovolumetric contraction?
|
Isovolumetric contraction is a term used in cardiac physiology to refer to an event occurring in early systole, during which the ventricles contract with no corresponding volume change.
|
|
|
What is isovolumetric relaxation?
|
That part of the cardiac cycle between the time of aortic valve closure and mitral opening, during which the ventricular muscle decreases its tension without lengthening so that ventricular volume remains unaltered; the heart is never precisely isovolumetric (vs. Isovolumic) except during long diastoles with a midiastolic period of diastasis. during isovolumetric relaxation the ventricle is not filled with blood, because the pressure there is still higher than in the atrium.
|
|
|
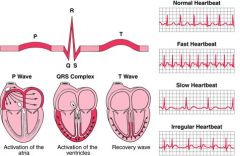
In the graph of left atrium pressure there are three waves: a, c, v, and two drops: x and y. What do they correspond to?
|
In order of the appearance on the curve:
a - wave is caused by active contraction of the atrium. c - wave occurs when the ventricles begin to contract causing the atrioventricular (AV) valves to bulge towards the atria. x - descent represents atrial relaxation and rapid atrial filling due to low pressure, while the ventricles contract and move the AV septum down. v - atria filling with blood, therefore pressure increasing. y - after atria-ventricular valves opening, blood flows from atria to ventricle, pressure decrease. |
|
|
What is the reason for the heart sounds "lub" - "dub"?
|
The closure of the valves in the heart. Lub - closure of AV valves. Dub - closure of the aortic and pulmonary valves.
|
|
|
What is the normal range for the cardiac output?
|
4,5 - 5,5 L/min.
|
|
|
It is possible to change cardiac output by changing what?
|
Heart rate or/and stroke volume, because
CO = HR x SV. |
|
|
How do you calculate the stroke volume using systolic and diastolic volumes?
|
SV = end diastolic volume - end systolic volume.
|
|
|
What is end diastolic volume?
|
The max volume of blood within the heart just before the contraction. Max filling of the ventricle during diastole.
|
|
|
What is end systolic volume?
|
Max volume of blood in the heart at the end of the contraction, systole.
|
|
|
What is afterload?
|
Resistance against contraction, in other words, the tension produced by a specified chamber of the heart in order to contract. For example, if the afterload is high (narrowing of the aorta) the resistance against contraction is high, so the heart must pump blood with larger force.
|
|
|
What NS input can increase the heart rate twice?
|
Sympathetic input.
|
|
|
How can the EDV be increased?
|
End diastolic volume can be increased by increasing the venous return to the heart and/or increasing ventricular compliance (ventricals are more easily expended).
|
|
|
How can the ESV be decreased?
|
End systolic volume can be decreased by increasing the contractility of the ventricles and/or decreasing afterload (resistance to contraction).
|
|
|
Present the Frank-Starling law about the stretching of the heart.
|
The more heart is stretched, the more it will contract. Because the venous return has to match the cardiac output. If there is more blood returning to the heart, the heart stretches and contracts harder to pump that blood out. The idea is that the contractility of the ventricle can be increased by increasing the EDV.
|
|
|
How the contractility of the ventricles can be increased without changing the EDV?
|
By the positive ionotropic agents.
|
|
|
What can decrease contractility of the ventricles without change in EDV?
|
Negative ionotropic agents (b blockers, ca channel blockers).
|
|
|
Shortly describe isotonic, isometric and auxotonic contractions of the muscle.
|
Isotonic contraction - same pressure/tension, change in length/ volume;
Isometric contraction - same volume/length, change in tension/ forse; Auxotonic contraction - change in volume and pressure. |
|
|
What is the difference between skeletal and cardiac muscle tension at a resting length?
|
At resting length skeletal muscle are able to generate maximum force, but cardiac muscle can generate stronger contraction at larger lengths than resting. This is important because of the Frank-Starling law: increase in EDV increases the contraction of the heart and therefore the cardiac output.
|
|
|
What is MABP?
|
Mean arterial blood pressure, it's the overal blood pressure within the body.
|
|
|
How the MABP can be calculated?
|
MABP = CO x TPR;
MABP = DP + 1/3 PP (which is SP-DP) |
|
|
How will the haemorrhage (blood loss) affect the cardiovascular system?
|
- Blood loss will decrease the volume of blood;
- therefore decreasing the venous return to the heart (because venous - - return is directly proportional to the blood volume/venous compliance); - next EDV is decreased (Frank-Starlings law); - SV is decreased (because SV=EDV-ESV); - CO is decreased (because CO=SVxHR); - thus MABP is going to decrease (MABP=COxTPR); - lower pressure, less blood supply to the tissues. |
|
|
What would be the response of sympathetic activity of the body to the haemorrhage?
|
Increased sympathetic activation. What has four effects:
- venoconstriction (releases blood stored in the veins and therefore increases the venous return to the heart, thus incr.in EDV); - increases contractility (which decr. ESV, thus incr.SV, => incr.CO); - incr.HR (incr.CO); - vasoconstriction (incr.in resistance => incr.TPR). So, all together, the incr. CO and TPR will incr.MABP. |
|
|
What would be the response of renin-angiotensin-aldosterone pathway?
|
In response to low MABP kidneys will release renin, which will be converted to angiotensin I and angiotensin II afterwards. Angiotensin II can directly cause the vasoconstriction and venoconstriction.
Second, angiotensin II is causing the release of vasopresin, which causes the reabsorption of water in the kidneys. Furthermore angiotensin II causes the release of aldosterone which through reabsorbtion of salts causes the increase of the blood volume (by the osmosis). |
|
|
Why the mean arterial blood pressure is called Arterial?
|
Because the blood pressure represents the pressure only in the arteries, not in the veins.
|
|
|
What is baroreflex?
|
Short term regulation of blood pressure. The baroreflex or baroreceptor reflex is one of the body's homeostatic mechanisms for maintaining blood pressure. It provides a negative feedback loop in which an elevated blood pressure reflexively causes heart rate and, thus, blood pressure to decrease; in similar fashion, decreased blood pressure activates the baroreflex, causing heart rate and, thus, blood pressure to rise.
The system relies on specialized neurons, known as baroreceptors, in the aortic arch, carotid sinuses, and elsewhere to monitor changes in blood pressure and relay them to the brainstem. Subsequent changes in blood pressure are mediated by the autonomic nervous system. Atrial natriuretic peptide forms a parallel negative feedback loop in an endocrinological contrast to the renin-angiotensin system. |
|
|
How does the decrease in MABP affects work of sympathetic and parasympathetic NS?
|
The parasympathetic activity is decreased and the sympathetic activity is increased.
|
|

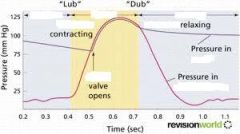
Label and explain.
|

|
|

Label.
|

|

