![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
248 Cards in this Set
- Front
- Back
|
What does glucocorticoids do to the WBC production?
|
Decrease it.
|
|
|
What is Kussmaul breathing?
|
Kussmaul breathing is a deep, labored breathing pattern that occurs in response to severe metabolic or diabetic acidosis.
|
|
|
Which hormones increase blood glucose level? |
Glucocorticoids, glucagon, growth hormones, thyroid hormones and catecholamines. |
|
|
Which branch of the vegetative nervous system and which nerve increases the secretion of insulin?
|
Parasympathetic, vagus nerve.
|
|
|
Which hormones decrease insulin production?
|
Somatostatin and catecholamines via alpha receptors.
|
|
|
Where is GLUT-1 found?
|
Blood brain barrier, RBCs and skeletal muscle.
|
|
|
Where is GLUT-2 found, and what is its function?
|
Small intestine, β-cells of pancreas, hepatocytes and proximal tubule of kidney. In the small intestine it's involved in glucose absorption, in the liver it's involved in glucose uptake and release, and in the proximal tubule it is involved in glucose reabsorption. |
|
|
What is the innervation of adrenal cortex?
|
Trick question, adrenal cortex has no innervation.
|
|
|
What is Addison's disease?
|
Addison's disease, or primal adrenal insufficiency, is an endocrine disorder where the adrenal cortex doesn't produce enough glucocorticoids, mineralocorticoids or androgens. |
|
|
What is Cushing syndrome?
|
Cushing syndrome, or primary adrenal hyperplasia, is caused by too much glucocorticoids in the blood. |
|
|
What can cause Addison's disease? |
It can be caused by autoimmune destruction of adrenal cortex.
|
|
|
What are the symptoms of Addison's disease?
|
It gives hypoglycemia due to low glucocorticoids and increased ACTH due to less glucocorticoid secretion, which means less negative feedback inhibition of ACTH secretion.Increased ACTH secretion also gives increased MSH secretion, which gives hyperpigmentation.
|
|
|
What can cause Cushing syndrome?
|
This can come from too high pharmacologic doses of glucocorticoids, or a hyperplasia of the adrenal gland.
|
|
|
What are the symptoms of Cushing syndrome?
|
Symptoms are hyperglycemia due to increased glucocorticoids, hypertension due to increased mineralocorticoids, decreased ACTH secretion due to negative feedback, central obesity and hypertension.
|
|
|
What is the difference between Cushing syndrome and Cushing disease? |
If the excess production of hormones by the adrenal gland is caused by too much ACTH (e. g by an ACTH secreting tumor), then it's called Cushing disease. If decreased ACTH is a symptom of something else (like glucocorticoid drugs), it's called Cushing syndrome. |
|
|
The deficiency of the enzyme 21-β hydroxylase will cause the deficiency of which hormones?
|
Aldosterone and cortisol.
|
|
|
The deficiency of 11-β hydroxylase will cause the deficiency of which hormones?
|
Aldosterone and cortisol.
|
|
|
The deficiency of 17-α hydroxylase will cause the deficiency of which hormones?
|
Cortisol and androgens (testosterone).
|
|
|
What is produced in the adrenal medulla?
|
Catecholamines
|
|
|
What innervates the adrenal medulla?
|
Preganglionic sympathetic cholinergic fibers.
|
|
|
How does insulin secretion affect K+ levels in the blood?
|
Decreases it due to increased K+ uptake in the cell.
|
|
|
Which cells produce somatostatin?
|
Delta cells in the Islets of Langerhans
|
|
|
What are the effects of parathyroid hormone, and where is it produced?
|
It increases serum Ca2+ and decreases serum phosphate. It is secreted by chief cells in the parathyroid gland. |
|
|
What are the functions of calcitriol (or 1,25-dihydroxycholecalciferol)?
|
It decreases Ca2+ and phosphate levels in the serum
|
|
|
What can block fast voltage-gated sodium channels?
|
TTX and lidocaine.
|
|
|
What can block voltage-gated potassium channels?
|
TEA
|
|
|
Which neurotransmitters are inhibitory?
|
GABA and glycine
|
|
|
Which neurotransmitters are excitatory?
|
Glutamate and aspartate.
|
|
|
How long does an action potential last in a neuron?
|
1-2 ms
|
|
|
How long does an action potential last in skeletal muscle?
|
4-6 ms.
|
|
|
How long does an action potential last in cardiac muscle?
|
200-300 ms.
|
|
|
How long does an action potential last in smooth muscle?
|
100-1000 ms.
|
|
|
Which type of neuron has the highest conduction velocity?
|
Aα.
|
|
|
Which type of neuron has no myelin sheet?
|
Type C fibres.
|
|
|
Where on the axon are fast voltage-gated sodium channels found?
|
On the axon hillock and the nodes of Ranvier.
|
|
|
Where on the axon are voltage-gated potassium channels found?
|
Under the myelin sheath.
|
|
|
What is the equilibrium membrane potential of K+?
|
-90 mV
|
|
|
What is the equilibrium membrane potential of Cl-?
|
-60 mV
|
|
|
What is the equilibrium membrane potential of Na+?
|
+50 mV
|
|
|
What are the extra-and-intracellular concenctrions of sodium ions?
|
Extracellular: 150 mM Intracellular: 15 mM |
|
|
What are the extra-and-intracellular concenctrions of potassium ions?
|
Extracellular: 5 mM Intracellular: 150 mM |
|
|
Will there be influx or efflux of sodium ions if the membrane potential is +65 mV?
|
Efflux (outflow).
|
|
|
Will there be influx or efflux of sodium ions if the membrane potential is +35 mV?
|
Influx (inflow).
|
|
|
Will there be influx or efflux of potassium ions if the membrane potential is -100 mV?
|
Influx (inflow).
|
|
|
Will there be influx or efflux of sodium ions if the membrane potential is -70 mV?
|
Influx (inflow) |
|
|
Will there be influx or efflux of sodium ions if the membrane potential is +50 mV?
|
Neither. There will be no net flow of sodium ions.
|
|
|
Will there be influx or efflux of chloride ions if the membrane potential is -100 mV?
|
Efflux (outflow).
|
|
|
Will there be influx or efflux of chloride ions if the membrane potential is -30 mV?
|
Influx (inflow).
|
|
|
What type of nerve fibers are used in the case of epicritic sensation (fine touch)?
|
Aβ.
|
|
|
What type of nerve fibers are used in the case of protopathic sensation (crude touch)?
|
Aδ.
|
|
|
What is the motor end plate potential?
|
0 mV
|
|
|
What is an inhibitory post-synaptic potential (IPSP)?
|
An IPSP is a postsynaptic potential that makes it more difficult for the postsynaptic neuron to generate an action potential, by increasing the threshold needed to generate the AP.
|
|
|
What is an excitatory post-synaptic potential (EPSP)?
|
An EPSP is a postsynaptic potential that makes it less difficult for the postsynaptic neuron to generate an action potential, by decreasing the threshold needed to generate the AP.
|
|
|
Where in the body are the slowest action potentials generated?
|
The ventricles.
|
|
|
Where are the upper motor neurons?
|
Contralateral precentral gyrus.
|
|
|
Where are the lower motor neurons?
|
In the cranial nerve nuclei in the case of the muscles innervated by cranial nerves, and in anterior horn of the spinal cord in the case of the other skeletal muscles.
|
|
|
What type of receptors are found on the neuromuscular junction? And what can block them?
|
Nicotinic acetylcholine receptors. Curare
|
|
|
The influx of which ion causes depolarization of the presynaptic membrane and release of the vesicles containing acetylcholine into the neuromuscular junction?
|
Ca2+.
|
|
|
What can be blocked by botulinus toxin?
|
The release of acetylcholine from the presynaptic terminal in the neuromuscular junction.
|
|
|
What is the effect of curare?
|
Curare is a competitive antagonist for nicotinic acetylcholine receptor. They can be used to relax muscles.
|
|
|
What is the effect of atropine? |
Atropine is a competitive antagonist for muscarinic acetylcholine receptor.
|
|
|
What does the Bell-Magendie law state?
|
It states that the ventral roots of the spinal nerve contain only motor fibres, while the dorsal roots contain only sensory fibres.
|
|
|
If you step on a piece of Lego with your left foot, what will happen to the flexors and the extensors on both legs?
|
The flexor in the left leg will be activated, the extensor in the left leg will be inhibited, while the flexor in the right leg will be inhibited and the extensor of the right leg will be activated.
|
|
|
What is the normal fasting blood glucose level?
|
4 - 5.5 mM
|
|
|
Which glucose transporter is insulin-dependent, and where is it found?
|
GLUT-4, which is found on all muscle types and adipose tissue.
|
|
|
What is rheobase?
|
The rheobase of a nerve is the minimal amount of current that is needed to excite the nerve, if the current was applied for an infinite amount of time.
|
|
|
What is chronaxie?
|
Chronaxie is the minimal amount of time needed for exciting a nerve or muscle by applying a current that is twice as high as the rheobase.
|
|
|
What is the effect of ether on a nerve?
|
Ether will block the nerve.
|
|
|
Which hormones are synthesized from the POMC polypeptide?
|
α-MSH, β-MSH, γ-MSH, ACTH, β-lipotropin and β-endorphin.
|
|
|
Which visual field crosses in the optic chiasm?
|
The temporal visual fields.
|
|
|
If you cut the optic chiasm, what will happen to the vision?
|
Both temporal visual fields will be lost, also known as heteronymous bitemporal hemianopia.
|
|
|
If you cut the right optic nerve, what will happen to the vision?
|
The whole visual on the right eye will be lost.
|
|
|
If you cut the right optic tract, what will happen to the vision?
|
The temporal visual field of the left eye, and the nasal visual field of the right eye will be lost, called homonymous contralateral hemianopia.
|
|
|
If you cut the right geniculocalcarine tract, what will happen to the vision?
|
The temporal visual field of the left eye, and the nasal visual field of the right eye will be lost, but the visual field of the macula will be spared. This is called homonymous hemianopia with macular sparing.
|
|
|
At what membrane potential will there be influx of Na+ and efflux of K+?
|
Between -90 mV and +50 mV.
|
|
|
At what membrane potential will there be influx of both Na+ and K+?
|
Below -90 mV.
|
|
|
At what membrane potential will there be influx of Na+ and influx of Cl-?
|
Between +50 mV and -60 mV.
|
|
|
At what membrane potential will there be efflux of both Cl- and K+?
|
Below -60 mV.
|
|
|
Which hormone is always produced in a 1:1 ratio as insulin?
|
C-peptide.
|
|
|
Where is GLUT-5 found, and what is special about it?
|
Found in the small intestine, transport fructose and not glucose.
|
|
|
What type of muscle fibers are innervated by α-motoneurons?
|
Extrafusal muscle fibers.
|
|
|
What type of muscle fibers are innervated by γ-motoneurons?
|
Intrafusal muscle fibers, a component of the muscle spindle.
|
|
|
What is the effect of somatostatin on insulin and glucagon?
|
Decreases secretion of both insulin and glucagon.
|
|
|
What are the three conditions where, if one of them is present in the patient, indicates diabetes mellitus?
|
1. Random plasma glucose > 11.1 mM 2. Fasting plasma glucose > 7.0 mM 3. Oral glucose tolerance test > 11.1 mM |
|
|
What cells can be found during the proestrus phase of the estrous cycle?
|
Parabasal and intermediary cells (nucleated, regular shaped epithelial cells), and a few leukocytes.
|
|
|
What cells can be found during the estrus phase of the estrous cycle?
|
Superficial cells (large, irregular shaped keratinized epithelial cells).
|
|
|
What cells can be found during the metestrus phase of the estrous cycle?
|
Leukocytes and a few cells with no nucleus (enucleated cells).
|
|
|
What cells can be found during the diestrus phase of the estrous cycle?
|
Very few cells, mostly leukocytes.
|
|
|
Which hormones are produced by the placenta?
|
hCG, hPL, chorionic TSH, chorionic ACTH, GnRH, progesterone, estriol (E3 estrogen).
|
|
|
In what way is hCG similar to certain other hormones?
|
The α-segment of TSH, FSH, LH and hCG are all identical.
|
|
|
What are the function of hPL?
|
Increases blood glucose and increases milk production.
|
|
|
What is DHEAS and where is it produced?
|
DHEAS, or dihydroepiandrosterone is produced in the reticular zone of the adrenal cortex, and is an intermediate in the sex hormone synthesis. DHEAS has very weak androgenic activity in the body. |
|
|
The deficiency of aromatase enzymes will lead to reduced levels of which hormones?
|
Estron (E1) and estradiol (E2).
|
|
|
What are the receptors of mineralocorticoids a nd glucocorticoids?
|
Receptor type 1 (mineralocorticoid receptor) - Binds both mineralocorticoids and glucocorticoids with the same affinity Receptor type 2 (glucocorticoid receptor) - Binds glucocorticoids with high affinity - Binds mineralocorticoids with low affinity |
|
|
In the case of protanopia which type of cone is affected?
|
It's caused by the lack of red-sensitive cones.
|
|
|
In the case of deuteranopia which type of cone is affected?
|
It's caused by the lack of green-sensitive cones. |
|
|
In the case of tritanopia which type of cone is affected?
|
It's caused by the lack of blue-sensitive cones.
|
|
|
What is the hypothalamo-hypophyseal-adrenal axis?
|
The hypothalamus secretes CRH, which stimulates the hypophysis to secrete ACTH, which stimulates the adrenal cortex to secrete steroids. It's regulated by feedback inhibition.
|
|
|
What are the effects of mineralocorticoids?
|
Increased Na+ and Cl- reabsorption, increased water reabsorption, increased blood pressure, increased H+ and K+ excretion. |
|
|
What is Conn's syndrome?
|
Conn's syndrome, or primary hyperaldosteronism is an endocrine disorder in which the adrenal cortex produces too much aldosterone.
|
|
|
What can be the causes of Conn's syndrome? |
Adrenal gland enlargement (hyperplasia), or an adrenal tumor that secretes aldosterone.
|
|
|
What are the symptoms of Conn's syndrome? |
Hypertension, hypokalemia, metabolic alkalosis and decreased renin secretion.
|
|
|
What is the hormone that the body produces in response to stress in the short-term?
|
Adrenalin, noradrenalin
|
|
|
What is the hormone that the body produces in response to stress in the long-term?
|
CRH -> ACTH -> Cortisol
|
|
|
What is the normal serum Ca2+ level?
|
2.2 - 2.6 mM
|
|
|
In what form is most of the calcium in the serum transported?
|
In free form (as Ca2+), up to 50% of the calcium in the serum.
|
|
|
What protein in the blood is Ca2+ bound to?
|
Albumin
|
|
|
A certain hormone is given to a test animal. The adrenals become enlarged, while the pituitary, thymus and body weight all reduce in size. What was the given hormone?
|
ACTH
|
|
|
A certain hormone is given to a test animal. The seminal vesicles, testes and body weight increase in size, while the pituitary decreases in size. What was the given hormone?
|
LH
|
|
|
A certain hormone is given to a test animal. The seminal vesicles and the body weight increase in size, while the pituitary and the testes decrease in size. What was the given hormone?
|
Testosterone
|
|
|
A certain hormone is given to a test animal. The pituitary and thyroid glands increase in size, while the body weight decreases. What was the given hormone?
|
TRH
|
|
|
A certain hormone is given to a test animal. The pituitary, thymus, adrenals and body weight all decrease in size. What was the given hormone?
|
A glucocorticoid.
|
|
|
A certain hormone is given to a test animal. The thyroid gland increases in size, while the pituitary and the body weight decrease in size. What was the given hormone?
|
TSH
|
|
|
The amplitude of an action potential is constant during it's propagation. True or false?
|
True. An action potential propagates with constant amplitude.
|
|
|
The size of the action potential is proportional to the size of the stimulus. True or false?
|
False. The size of an action potential is not proportional to the size of the stimulus.
|
|
|
The action potential has a refractory phase. True or false?
|
True. Action potentials are followed by a refractory phase.
|
|
|
An action potential can be both a depolarization or a hyperpolarization. True or false?
|
False. An action potential can only be formed by a depolarization.
|
|
|
Which parts of the body can discriminate the shortest distance between two points?
|
The fingertips, the tongue and the lips.
|
|
|
Which parts of the body is worst at discriminating the shortest distance between two points?
|
The back.
|
|
|
Which of the following will affect the contractile force of skeletal muscle? 1. the size of the motor unit 2. the amplitude of action potential in α-motoneurons 3. the amount of neurotransmitter released into the NMJ 4. the frequency of action potentials in the α-motoneuron |
4. Increased frequency of the action potential in the α-motoneuron will increase the contractile force.
|
|
|
Which of the following will affect the contractile force of skeletal muscle? 1. duration of the action potential in the α-motoneuron 2. amplitude of action potential in the α-motoneuron 3. number of activated motor units 4. the number of functional motor units |
3. When more motor units are activated, the contractile force of the skeletal muscle increases. and 4. |
|
|
What happens in myasthenia gravis?
|
Antibodies are produced against nicotinergic acetylcholine receptors.
|
|
|
Which type of receptor is found in the neuromuscular junction?
|
Nicotinergic acetylcholine receptor.
|
|
|
Which type of acetylcholine receptor is a metabotropic receptor?
|
The muscarinic acetylcholine receptor is a metabotropic receptor.
|
|
|
What is a metabotropic receptor? |
A receptor that is a G-protein coupled receptor
|
|
|
What is an ionotropic receptor? |
A receptor that is a ligand-gated ion channel.
|
|
|
Which type of acetylcholine receptor is an ionotropic receptor?
|
Nicotinic acetylcholine receptor.
|
|
|
What is the mechanism of malignant hyperthermia?
|
A mutation in the ryanodine receptor causes increased Ca2+ release from the sarcoplasmic reticulum
|
|
|
What is the reversal potential of nicotinic acetylcholine receptor ion channel?
|
0 mV
|
|
|
What is the motor unit potential?
|
The motor unit potential is the sum of the muscle fiber action potentials in one motor unit.
|
|
|
What will cutting the dorsal roots do when the test subject has decerebrate rigidity?
|
Decrease the excessive muscle tone.
|
|
|
What is adrenogenital syndrome (virilism)?
|
Adrenogenital syndrome is a condition where too high production of sex hormones leads to changes in sex characteristics.
|
|
|
What can be the cause of adrenogenital syndrome? |
21β-hydroxylase deficiency, overproduction of hormones in the reticular zone or overproduction of androgens.
|
|
|
Conduction velocity is measured in a nerve. The distance between the first recording site and the electrode is 15 mm, and the distance between the second recording site and the electrode is 28 mm. The latency between the two stimuli was 0.5 ms. What is the conduction velocity?
|
26 m/s (28 mm -15 mm)/ 0.5 ms = 26 mm/ms = 26 m/s |
|
|
What are the symptoms of spinal shock?
|
No peripheral thermoregulation Passive incontinence Hypotension Anasesthesia below lesion Areflexia below lesion Paralysis below lesion No autonomic reflexes below lesion. Respiration paralysis (If lesion above C4). |
|
|
What is the innervation rate?
|
The number of muscle fibers that are innervated by one α-motoneuron in one muscle.
|
|
|
What is the motor unit potential?
|
The motor unit potential is the sum of the action potentials of the muscle fibers in one motor unit
|
|
|
What is the consequence of a neurogenic muscle weakness?
|
The amount of motor units decrease while their size increase (increased innervation rate).
|
|
|
What is the consequence of a myogenic muscle weakness??
|
The size of motor units decrease.
|
|
|
The opening of which channel causes EPSP?
|
Opening of nonspecific cation channels.
|
|
|
Which of the dynamic and static afferents of the muscle spindles adapt fastest?
|
The dynamic afferents adapt faster than the static.
|
|
|
In which muscle types can tetanic contraction develop?
|
In smooth and skeletal muscle.
|
|
|
What are Renshaw cells?
|
Renshaw cells are inhibitory interneurons in the grey matter of spinal cord.
|
|
|
Which sensory organ in the skin is the fastest adapting?
|
Pacinian corpuscles.
|
|
|
The the central descending analgetic system, which neurotransmitter is important?
|
Serotonine
|
|
|
The electrotonic potential in a dendrite propagates with constant amplitude. True or false?
|
False. The potential in dendrites propagate with decreasing amplitude.
|
|
|
The size of the electrotonic potential is proportional to the size of the stimulus. True or false?
|
True.
|
|
|
The electrotonic potential in dendrites have refractory period. True or false?
|
False. Electrotonic potentials in dendrites have no refractory period.
|
|
|
The polarity of the electrotonic potential in dendrites is only depolarization. True or false?
|
False. It can be either depolarization or hyperpolarization.
|
|
|
What is myopia? How is the longitudinal axis of the eye in the case of this condition?
|
Myopia, or nearsightedness, is a condition when the eye has a longer longitudinal axis than normal. |
|
|
In the case of myopia, are the light rays focused behind or in front of the retina? |
In front of the retina.
|
|
|
What is hyperopia? How is the longitudinal axis of the eye in the case of this condition?
|
Hyperopia, or farsightedness, is a condition where the eye has a shorter longitudinal axis than normal.
|
|
|
In the case of hyperopia, are the light rays focused behind or in front of the retina?
|
Behind the retina.
|
|
|
Is ATP needed for skeletal muscle relaxation or contraction?
|
Both. ATP is needed for both skeletal muscle relaxation and contraction.
|
|
|
What is the function of intrafusal muscle fibers?
|
Intrafusal muscle fibers determine the sensitivity of muscle spindles.
|
|
|
What is the normal blood pH?
|
7.35 - 7.45
|
|
|
What is the normal serum protein concentration?
|
60 - 80 g/L
|
|
|
How does the stimulus intensity affect sensory receptor potentials?
|
The size of the sensory receptor potentials depend on the size of stimulus intensity.
|
|
|
What is the direction of blood flow in the adrenal cortex?
|
Glomerular zone > Fascicular zone > Reticular zone Basically from outside towards the medulla. |
|
|
How is the motor unit potential affected in the case of a neurogenic muscle weakness?
|
The motor unit potential has a larger amplitude.
|
|
|
The stimulation of which adrenergic receptor increases myocardial strength?
|
Beta -1 adrenergic receptor |
|
|
Give the correct order of Ortho-Tuildin blood glucose determination (sample from rabbit).
|
1. Protein denaturation by TCA
2. Centrifugation 3. Add color reagent (Orto-toluidin) 4. Boiling on water bath 5. Photometry at 630 nm |
|
|
What does the all-or-none law state, and to which type of membrane potential does it apply?
|
The law states that the magnitude of an action potential is independent of the size of the stimulus. If the stimulus reaches threshold, there will be an action potential, but if the stimulus doesn't reach threshold, there will be no action potential. There is no effect where a bigger stimulus gives a bigger action potential. |
|
|
We apply two electrodes to a nerve connected to a muscle. In this case, the negative pole (cathode) is closer to the muscle than the positive pole (anode). We apply a medium stimulus. Will the muscle contract when we close or break the circuit?
|
When the cathode is closest to the muscle, it will contract when we close the circuit (turn on the electrodes).
|
|
|
We apply two electrodes to a nerve connected to a muscle. In this case, the positive pole (anode) is closer to the muscle than the negative pole (cathode). We apply a medium stimulus. Will the muscle contract when we close or break the circuit?
|
When the anode is closest to the muscle, it will contract when we break the circuit (turn off the electrodes).
|
|
|
We apply two electrodes to a nerve connected to a muscle and turn them on, delivering a continuous direct current. At which pole is excitability increased and at which is it decreased?
|
Excitability increases at the cathode (negative pole), and decreases are the anode (positive pole).
|
|
|
Conduction velocity is measured in a nerve. The distance between the electrode and the recording sites are 10 mm, 15 mm, 20 mm and 25 mm. The latency between the two stimuli was 0.5 ms. What is the conduction velocity?
|
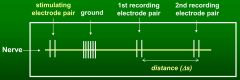
20 m/s In this question, there are two pairs of recording electrodes, like in the drawing. So to find the distance Δs (on the figure), we need to subtract either 25 mm - 15 mm = 10 mm or 20 mm - 10 mm = 10 mm. 10 mm / 0.5 ms = 20 m/s |
|
|
Which factors increase conduction velocity?
|
Nerve fiber diameter ↑ Myelinization ↑ Increased temperature |
|
|
Which tracts form the pyramidal tract?
|
The corticospinal and corticobulbar (or corticonuclear) tract.
|
|
|
What are the signs of an upper motoneuron lesion?
|
Muscle stength ↓ Increased muscle tone of flexors of upper extremities Increased muscle tone of extensors of lower extremities Increased muscle tone generally Clasp knife reflex can be seen Babinski sign can be seen Hyperreflexia |
|
|
What does positive Babinski sign indicate?
|
An upper motoneuron lesion.
|
|
|
What are the signs of a lower motoneuron lesion?
|
Muscle stength ↓ Muscle tone ↓ Significant atrophy Hyporeflexia |
|
|
What are the symptoms of cerebellar damage?
|
They are ipsilateral Nystagmus Walking deviation, in the same direction as the damage (left/right) Muscle tone ↓ Myotatic reflexes ↓ Drunk-like speech |
|
|
Which cell type of the cerebellum is excitatory? |
The granule cells. |
|
|
Which cell type is the only output of the cerebellum, and is it excitatory or inhibitory? |
The Purkinje cell, which is inhibitory.
|
|
|
The parallel fibers in the cerebellum are the axons of which cells?
|
Granule cells.
|
|
|
Where do the climbing fibers come from, and are they excitatory or inhibitory?
|
They come from the inferior olivary nucleus (olivocerebellar tract), and are excitatory.
|
|
|
Which mechanoreceptors in the skin are slow-adapting?
|
Merkel cells and Ruffini corpuscles.
|
|
|
What type of fibers are the preganglionic fibers of the autonomous nervous system?
|
Type B nerve fibers. |
|
|
What type of fibers are the postganglionic fibers of the autonomous nervous system?
|
Type C nerve fibers.
|
|
|
What is the neurotransmitter in autonomic ganglia, and what is the neurotransmitters receptor?
|
Acetylcholine, the receptor is nicotinic acetylcholine receptor.
|
|
|
How many molecules of acetylcholine are needed to activate the nicotinic Ach-receptor in the NMJ?
|
2 molecules are necessary
|
|
|
What are the functions of the different troponins? |
Troponin C: Binds Ca2+ (4 binding sites) |
|
|
What kind of receptors can be found in the T-tubules of the striated muscles? And what do they do? |
DHP-receptors (Dihydropyridine-receptors). They change conformation when depolarization occurs. |
|
|
How does Ca2+ get released into the sarcoplasma? |
When a DHP-receptor is depolarized by Action Potential, it will change confirmation and open up the Ryanodine receptors of the terminal cisternae --> Ca2+ goes out in the sarcoplasma. |
|
|
What is Calsequestrin? |
Its a protein that binds up Ca2+ inside the Terminal Cisternae, to maintain low concentration of Ca2+ and reduce work load on Ca2+-ATPase. |
|
|
What kind of changes happen in the sarcomere during contraction? |
- Width of I-band and H-band decrease - M-lines and Z-lines get closer. - Myosin slides among actin filaments. |
|
|
What is the function of Dystropin? |
It anchores Actin to the cell membrane. |
|
|
Which reflexes are proprioceptive? |
Patellar reflex Achilles reflex Radius reflex Biceps reflex Triceps reflex Masseter reflex |
|
|
What are the characteristics of proprioceptive reflexes? |
They are deep reflexes, they are intrinsic (receptor and effector is the same), they are monosynaptic and they have their reflex centres in the spinal medulla (except masseter reflex). |
|
|
What are the receptors, afferent limb, efferent limb and effectors of a myotatic reflex?
|
Receptor: Muscle spindle Afferent limb: Iα sensory fiber Efferent limb: Aα motoneuron Effector: The muscle that was stimulated will contract, the antagonist will relax. |
|
|
What is the mechanism of the tetanus toxin (the toxin from Clostridium Tetani)? |
Inhibiting inhibitory motoneurons in spinal medulla, like Renshaw cells by blocking GABA and glycine transmission, causing spastic paralysis. |
|
|
What is the main neurotransmitter of Renshaw cells? |
Glycine |
|
|
What are the receptors, afferent limb, efferent limb and effectors of the inverse myotatic reflex (Golgi tendon reflex)? |
Receptor: Golgi tendon organ Afferent limb: Ib sensory fibers Efferent limb: Aα motoneuron Effector: Relaxation of agonist muscle, contraction of antagonist muscle. |
|
|
What are the characteristics of the inverse myotatic reflex (Golgi tendon reflex)? |
It is a deep reflex, it's polysynaptic, has its reflex center in the spinal medulla and is extrinsic (the effector is different from the receptor). |
|
|
What is the role of the inverse myotatic reflex (Golgi tendon reflex)? |
To protect against tearing of the tendon and to regulate contraction force during movement. |
|
|
Which reflexes are exteroceptive (extrinsic)? |
Flexor reflexes Crossed extensor reflexes Corneal reflex Abdominal skin reflex Plantar reflex Cremasteric reflex |
|
|
What are the characteristics of the exteroceptive (extrinsic) reflexes? |
Their receptors are located in the skin, they are extrinsic (the receptor is not the same as the effector), they are polysynaptic and have fast adaptation. |
|
|
What are the receptors, afferent limb, efferent limb and effectors of the flexor - crossed extensor reflex? |
Receptors: Nociceptors in skin Afferent limb: Type Aδ and type C sensory fibers. Efferent limb: Aα motoneuron Effector: Contraction of ipsilateral flexor, relaxation of ipsilateral extensor, contraction of contralateral extensor, relaxation of contralateral flexor. |
|
|
What are the receptors, afferent limb, efferent limb and effectors of vegetative reflexes? |
Receptors: Skin receptors (like Vater-Pacini corpuscles) or visceral interoceptors Afferent limb: Aβ, Aδ and type C sensory fibers Efferent limb: Preganglionic fibers -> ganglion -> postganglionic fibers Effector: Smooth muscle, glands |
|
|
What are the characteristics of viscero-visceral reflexes? |
Both the receptor and the effector are parts of the vegetative nervous system. |
|
|
What are some examples of viscero-visceral reflexes? |
Carotid sinus reflex, depressor reflex, chemoreflex. |
|
|
What are the characteristics of somato-visceral reflexes? |
The receptor is a part of the somatic nervous system while the effector is a part of the vegetative nervous system |
|
|
What are some examples of somato-visceral reflexes? |
Pilomotoric reflex (hairs standing up during cold), pupillary light reflex. |
|
|
Which reflexes can be elicited in the intact frog? |
Corneal reflex, turning reflex, immobility reflex, compass reflex (+ the spinal frog reflexes obviously). |
|
|
Which reflexes can be elicited in the spinal frog? |
Wiping reflex, embracing reflex, flexor-crossed extensor reflex |
|
|
What causes decerebration rigidity?
|
Lesion of the CNS at the level of medulla oblongata or pons. |
|
|
The lesion of what part of the brain makes the test animal a bulbospinal animal? |
Lesion between medulla oblongata and pons, above Deiters nucleus (low decerebration). |
|
|
The lesion of what part of the brain makes the test animal a mesencephalic animal? |
Lesion above the caudal end of red nucleus (nucleus ruber). (high decerebration) |
|
|
The lesion of what part of the brain makes the test animal a thalamic animal? |
Lesion above the thalamus (decortication). |
|
|
What are the symptoms of a bulbospinal animal (low cerebration)? |
- Increased tone of extensors - Normal somatic sensation (but is unconscious) - Cannot stand up spontaneously - Normal respiration (eupnoe) - No thermal regulation - No spontaneus locomotion. - Static reflexes and grasp reflexes are present - Reflexes are normal - Circulation is normal |
|
|
What are the symptoms of a mesencephalic animal (high decerebration)? |
- Increased tone of extensors - Normal somatic sensation (but is unconscious) - Cannot stand up spontaneously (non-primates can!) - No spontaneous locomotion - Normal thermoregulation - Normal respiration (eupnoe) - Circulation is normal - Static reflexes and grasp reflexes are present - Reflexes are normal |
|
|
What are the symptoms of a thalamic animal (decortication)? |
- Normal thermoregulation - Normal circulation - Normal respiration (eupnoe) - All signs of pyramidal lesion are present - Flexion in upper extremities - Extension in lower extremities |
|
|
Which brain nuclei increase muscle tone? |
- Rostral reticular formation - Deiters nucleus (lateral vestibular nucleus) |
|
|
Which brain nuclei decrease muscle tone? |
- Certain parts of cortex - Basal ganglia - Cerebellar cortex - Caudal reticular formation - Red nucleus (nucleus ruber) |
|
|
What is decerebrate regidity? |
When the extensors in both upper and lower limbs increase, often because of decerebration. |
|
|
What can decrease the excessive muscle tone of the extensors in the case of decerebration rigidity?
|
Cutting dorsal roots. |
|
|
What is the reason for astigmia?
|
The surface of the cornea is not perfectly spheric |
|
|
What is the main neurotransmitter of the rods and cones? |
Glutamate |
|
|
What types of vision are the rods responsible for?
|
Light sensation, achromatic (no color), scotopic (in the dark) vision |
|
|
What types of vision are the cones responsible for? |
Phototopic vision (color vision) |
|
|
What is the "dark current"? |
When rods are not stimulated (in dark), an electric current flows in the cell that leads to continuous Glutamate release. This current is called "dark current". |
|
|
What is special about the activation of rods? |
When activated they are hyperpolarized and not depolarized, like is normal in other receptors. |
|
|
What takes the most time; adapting to dark or adapting to light? |
Adapting to dark takes the most time. |
|
|
The change of intracellular level of which ion is essential for dark and light adaptation? |
Ca2+ |
|
|
What is the main neurotransmitter of horizontal cells in the retina? |
GABA |
|
|
What is the function of horizontal cells in the retina? |
Horizontal cells increase contrast by inhibiting bipolar cells surrounding them. |
|
|
What are the two parts of the lateral geniculate nucleus, and what type of visual information do they process? |
Parvocellular part of LGN - Color vision - Recognizes shapes, details - Understands what is being looked at Magnocellular part of LGN - No color vision - Recognizes depth, motion - Understands where we are looking |
|
|
Where do extrageniculte optic fibers terminate to? |
- Erdinger-Westphal nucleus - Superior colliculus - Hypothalamus (suprachiasmatic nucleus) - Tegmentum of mesencephalon - Pretectal area |
|
|
What is the reflex arch of the pupillary light reflex? |
Receptor: Photosensitive ganglionic cells in retina Afferent limb: Optic nerve Reflex center: Pretectal nucleus -> Erdinger Westphal nucleus Efferent limb: Occulomotor nerve --> ciliary ganglion --> short ciliary nerves Effector: Contraction of pupillary sphincter |
|
|
When we see something moving the peripheral visual field, which brain structure is activated? |
Superior colliculus |
|
|
What is nystagmus? |
Nystagmus has two components: 1. When the eye moves slowly to one side 2. When the eye quickly moves back to the center |
|
|
Which component of nystagmus determines its direction? |
The fast component |
|
|
Inserting warm water into the right external ear canal will induce nystagmus in which direction? |
Nystagmus to the right. |
|
|
Inserting cold water into the right external ear canal will induce nystagmus in which direction? |
Nystagmus to the left. |
|
|
Damage to the vestibular system will cause nystagmus to which side? |
Contralateral to the side of the damage. |
|
|
Damage to the cerebellum will cause nystagmus to which side?
|
Ipsilateral to the side of the damage. |
|
|
What are the types of brain waves? |
Alpha, beta, delta, gamma and theta waves |
|
|
What are the characteristics of beta waves?
|
13-30hz. Present while awake with open eyes, during activity or during REM sleep |
|
|
What are the characteristics of alpha waves? |
8-12hz. Present at rest with closed eyes. |
|
|
What are the characteristics of theta waves? |
4-8hz. Normal in children. Found in adults during deep sleep or fatigue. |
|
|
What are the characteristics of delta waves? |
0.5-4 Hz. During slow wave sleep. If present while awake -> brain damage. |
|
|
What are the characteristics of gamma waves?
|
>30 Hz.
|
|
|
What are evoked potenitals? |
When we give an external stimulus to the patient, like a sound, shock or light blink, a short potential can be seen on EEG. They're usually very small compared to the "background noise" on the EEG and must be therefore be repeated many times to be seen. |
|
|
What is the function of the ascending reticular activating system (ARAS)? |
Waking up during sleep, arousal and maintaining attention while awake. |
|
|
Which hormone and which molecular events are involved in sensitization? |
Serotonin causes inhibition of presynaptic K+ channels and activation of voltage-dependent Ca2+ channels. |
|
|
During which phases of absorption is insulin active? |
Between meals (postabsorptive phase) but mainly after meals (absorptive phase) |
|
|
During which phases of absorption is glucagon active? |
The postabsoprtive phase |

