![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
231 Cards in this Set
- Front
- Back
|
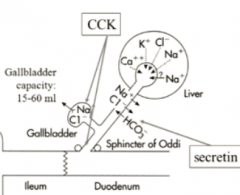
Name all hormones released in response to fat in the SI
|
secretin (also activates GB)
CCK (needed to activate GB) and GIP (feel sluggish due to low blood sugar) |
|
|
What can you say about the effect of SS on the general GI system?
Does it affect all hormones or all motility? |
it decreases secretion of all hormones
|
|
|
Generalize all the hormones that will constrict the pylorus
|
all the ones that sense that food is here:
gastrin, CCK, Secretin, GIP |
|
|
What stimulates GIP release in the SI?
|
every nutrient - AA, FA, and glucose
|
|
|
How can you easily remember the effects and triggers for GIP?
|
it triggers insulin release and insullin triggers the storage of all nutrients in the body
|
|
|
How do you remember the three SI hormones (secretin, CCK, and GIP)'s effect on the stomach.
|
They only have one function each.
They all inhibit gastric acid secretion except for CCK which inhibits the motility. Lucy used to take those oil shots to delay gastric emptying and feel fuller... even though they didn't work. |
|
|
How do you remember the actions of secretin? (3)
|
it just aims to decrease acid everywhere
increase HCO3- in pancreas and GB decrease H+ in stomach |
|
|
Why it a good thing that we decrease salivation when we sleep?
|
then We don't lose all our moisture by it evaporating
|
|
|
How do I remember that CCK is also released in response to amino acids?
|
You have to remember that it has the alternate function of releasing pancreatic enzymes to deal with that
|
|
|
What are the 2 gastrointestinal hormone groups that are analogous to one another?
|
CCK and gastrin
secretin, GIP, and glucagon |
|
|
What common analogous functions do CCK and gastrin have in common?
|
Only that they maintain the growth of the cells around them
|
|
|
How does retropulsion work again? What is the muscle contraction pattern?
|
It works because peristalsis increases in force and velocity as it goes to the antrum. The velocity becomes bigger than the chyme and squeezes it back
|
|
|
How do you remember what vagal neuropathy does to stomach tone and emptying?
|
it's just like an UMN. The stomach becomes unable to relax when it is gone.
|
|
|
What is the difference between a retch and a vomit?
What spincters are open vs closed? What is the pressure in the thoracic and abdominal cavities? |
UES is closed in a retch
both cavities are increeased pressure in vomiting thoracic pressure is decreased and abdominal pressure increased in retching |
|
|
How do you decreas thoracic pressure in a retch?
|
you inspire against a closed glottis (air same, volume llarger)
|
|
|
How do you increase pressure in vomiting?
|
by pressing both your abdomen and chest in
|
|
|
Do gastrin and CCK have the same second messenger? If so, what is it?
|
yes, they both increase Ca2+
|
|
|
Mnemonic for second messenger of gastrin and CCK
|
Take first letter of CCK and second letter of gastrin to get Ca
|
|
|
Name all 3 stimulators for pancreatic enzyme secertion
|
vagal Ach
CCK secretin (GIP deals with regulating insulin more) |
|
|
Are the strongest signal for pancreatic enzyne secretion the gut derived hormones or the vagal stimulation?
By how much? |
the gut hormones
|
|
|
Which two have the greatest potentiation and why?
|
CCK and secretin
secretin because it has the econd messenger that is different CCK because it is the most powerful |
|
|
What are twp rules that dictate what controls gastric acid and pancreatic secretions?
|
there are always 3 transmitters, one of which is vagal ACh
|
|
|
How is it that we get neural control to the pancreas? What stikmulates it? What phage of digestion is this in?
|
in all phases of digestion, but strongest early on- this is in the cepahlic and gastric phases when we are getting signals from our brain and the enteric NS that food is coming
intestinal phase- vagovgal reflexes from afferent nutrient and H+ sensors in the duodenum |
|
|
What is the more specific role of secretin vs CCK vs ACh in the pancreas?
|
CCK and ACh stimulate both duct and acinar cells
secretin only concerns itself with duct cells |
|
|
Why is retching good for preparing for vomiting?
Explain the advantages of creating the different pressures. |
it brings food up to the esophagus by negative thoracic pressure.
then in vomiting you can increase thoracic pressure to squeze out that food |
|
|
How can hypervitaminosis A lead to esophageal varices?
|
too much vitamin A in stellate liver cells --> injury --> turn into myofibroblasts --> secrete collagen into hepatic portal circulation --> portal HTN --> blood goes to esophagus
|
|
|
If we took away one hormone to simulate cystic fibrosis, what would it be? WhY?
|
secretin because it's mechanism is to open up the CFTR
|
|
|
similarities between achalasia and delayed gastric emptying pathophysiologies
|
tehy are bot cause by a decrease in vagal stimulation
|
|
|
compare when the UES vs LES opens.
|
UES opens when the bolus is knocking
LES gets wind of the UES opening and will open soon after it opens to be ready for the bolus |
|
|
What is the role of secretin in both the GB and pancreas?
|
open up CFTR to increase bicarb and water secretion in the ducts
|
|
|
Secretin is sidekick to which hormone? Why?
|
CCK because CCK releases the ezymes/bile and secretin helps to give enough water and bicarb to SECRETE them
|
|
|
What vitamin are bile acids reabsorbed with? Where in the GIT is this?
|
Vitamin B12 in the distal ileum
|
|
|
What was the most important lecture?
|
the second one about stomach, pancreas, and small intestine (thank goodness I spent so long on it!)
|
|
|
What does ACh do to sphincters?
|
contraction
|
|
|
Is costanzo infallible?
|
no, apparently it has a lot of errors
|
|
|
What is responsible for the emulsifying properties of bile? (2)
What is emulsification? |
fat and electrolytes
breaks fats into tiny droplets |
|
|
talk about the hydrophobic and electronic things that must happen to emulsify fat in the SI by bile.
|

the lipid part of bile attracts the fat.
The negative outside of bile sticks outside The negatives repel one another to make sure the droplets don't coalesce |
|
|
Why is bile acid synthesis clinically significant?
|
gallstones can happen when it goes wrong
|
|
|
Why do gallstones form? (what conditions need to be present)
|
They form when there is an imbalance of cholesterol, bile salt, or bilirubin
|
|
|
What purpose do bile salts serve for cholesterol?
What happens if there is not enough bile salts compared to cholesterol? |
They emulsify cholesterol just like that. We get precipitation of cholesterol gallstones. If there is not enough bile salts or too many cholesterol's
|
|
|
What do you get if there is too much bilirubin?
|
Precipitation of bilirubin gallstones.
|
|
|
What is the difference in appearance of cholesterol versus bilirubin gallstones?
Which one is most prevalent |

Cholesterol stones are yellowish greenish and light colored
bilirubin stones are darker. The above are bilirubin stones Cholesterol stones are 80% of all gallstones |
|
|
Show cholesterol stones
What is the size variation of gallstones? |

They can be as small the grain of sand or as large as a golf ball
|
|
|
Why does bilirubin and chl form stones?
|
they are hydrophobic in an aqueous worlds and there is not enought bile salt to emulsify them
|
|
|
What kind of stones do you get when there are too little bile salts?
|
a mix of chl and bilirubin stones
|
|
|
What is the mnemonic for what demographics are likely to develop gallstones?
|

The 5 F's
Female- more estrogen Fourties Fertile- more estrogen Fair Skinned Fat- more cholesterol |
|
|
What two nutrients require bile salts?
|
fats and fat soluble vitamins
|
|
|
How does bile end up in the gallbladder? (physics)
|
if the liver is secreting bile and the sphincter of oddi is closed, it will back up to the gallbladder
|
|
|
What are the function of CCK on bile secretion?
|
It will both contrast the gallbladder and open the sphincter of Oddi
|
|
|
Describe the they enterohepatic circulation of bile salts.
In a normal meal. How many times will the cycle happen? How many times can it happen in a high-fat meal? |
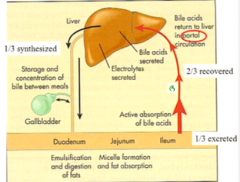
Usually happens 2 to 3 times meal, but in a high-fat meal it can happen as many as 10 times
|
|
|
What are the 2 functions of the liver when it comes to bile?
|
It does de novo synthesis and secretion
|
|
|
How much bile is reabsorbed and is this a active or passive process?
What vessel carries reabsorbed bile back to the liver? |
Two thirds of it is actively reabsorbed in the ileum and what into a portal circulation directly back to the liver. (This is not the same as the hepatic portal vein)
|
|
|
What sign regulates both files secretion and synthesis in the liver?
|
The rate that bile comes back to the liver in the portal circulation
|
|
|
What does increased bile return to the liver due to de novo synthesis versus secretion?
What is this essentially telling the liver? |
The liver knows that a meal is going on, so it increases secretion, but decreases synthesis because it is putting all of it's Energy towards secretion
|
|
|
What trigger would stimulate the liver to start synthesizing more bile salts?
|
A decrease in return of bile salts
|
|
|
What effect would CCK have on bile secretion and synthesis? Why?
|
It would increase secretion and decrease synthesis because it would allow bile salts to get out into the small intestine to later be reabsorbed
|
|
|
Generally, what happens to the liver as we age?
|
All functions go down
|
|
|
What happens to our risk of gallstones? Why?
|
It increases because the liver is able to produce less emulsifying bile salts
|
|
|
What happens to our ability to process toxins and drugs? How must doctors modify prescription doses for geriatrics?
Name 2 reasons why this happens |
It goes way down. So older people must have lower doses of drugs
The liver is not able to enzymatically breakdown of the drugs as fast and it circulation is also decreased so it gets less of the drugs delivered to it |
|
|
How does the effects of medications change as we age? 2 ways due to the liver
|
The half-life increases and so does the side effects
|
|
|
What happens the secretory ability of the pancreas As we age?
|
, It is able to secrete and synthesize less enzymes
|
|
|
What nutrient do we become much less tolerant to as we age? Name one liver and one pancreas related reason why
|
Facts
liver is able to produce less bile salt. Pancreas is able to produce less lipase |
|
|
What happens to the duct cells of the pancreas As we age?
|
They undergo ductal hyperplasia and fibrosis
|
|
|
How much fluid does the liver secrete into the lumen every day?
Does the liver change the pH of the blood like the pancreas and the stomach did? |
1 L per day
no because it doesn't secrete any acid or bicarb |
|
|
Compare the small and large intestine in terms of how
much nutrients is absorbed long it is wide it is long food stays in there |
Small intestine absorbs 90% of nutrients, is much longer, but not as wide, and only keeps food for 2 to 3 hours as opposed to 1 to 2 days
|
|
|
Compare the length of each section of the small intestine
|
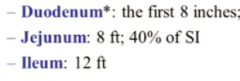
They get progressively longer
|
|
|
Which 2 sections are responsible for the majority of the digestion and absorption?
|
The duodenum and the jejuneum (first two sections)
|
|
|
What kind of absorption is the ileum responsible for?
|
Just vitamin B12 and bile salts
|
|
|
What is special about the way that the duodenum is held in space?
|
It is the only part of the small intestine that does not have mesentery because it doesn't need to move. It is fixed in space
|
|
|
What are the two main surface features of the SI?
|
villi and crypts
|
|
|
What are the epithelial cells of the villi joined by?
How does this change from the start of the small intestine to the end? Why? |
They are joined by tight junctions which get tighter and tighter as you go further on. This is because more absorption takes place earlier on
|
|
|
What goes through the leaky tight junctions?
|
Water and electrolytes
|
|
|
After that is absorbed through the epithelia, what is its course?
|
It goes through the central lacteal into the thoracic duct and then into the left subclavian
|
|
|
What secretory function does the crypts have?
|
They secrete water and electrolyte
|
|
|
How are cells in the intestinal epithelia turned over?
|
The cribs contain themselves which migrate to the tip of the villi as we mature and then get shed off the tip as they die
|
|
|
What happens to the intestines in radiation therapy and why?
|
The lining suffers because there is such a high mitotic rate for crypt cells normally that is highly regulated
|
|
|
What kind of muscle movement produces segmentation?
What 2 functions does segmentation serve? |
Alternating contraction of circular muscle
Segmentation serves to mix kind and propel it forward |
|
|
How does segmentation manage to propel food forward?
|
There is a higher rate of alternating contractions in the duodenum than in the ileum
|
|
|
Compare the amount of peristalsis versus segmentation in the small intestine
Why is this ratio advantageous for this organ? |
There is much more segmentation and peristalsis because we don't want the food to move so quickly that we can't absorb it
|
|
|
Do we ever have more than one meal in the small intestine at a time?
What about in the large intestine? Why is this so? |
Only one meal in the small intestine at a time because every new meal mediates a clearing out of the small intestine via the gastroileal reflex.
We can have several meals in the colon at a time |
|
|
What mediates the gastroileal reflex? 2 things
|
It is under neuronal and hormonal control
It is stimulated by gastrin (we learned about this before) it is modified by extrinsic nerves such as the vagus |
|
|
Now we will hear some important nutritional information that Dr. Podolin got from DR. ANDREW WEIL!
|
yay!
|
|
|
Compare the GI of white vs whole wheat bread
|
it is the same
|
|
|
why are they the same?
|
because inw hole wheat they just add the bran back in, but it doens't encapsulate the endosperm to reduce it's absorption time at all
|
|
|
What percent of cancers can be attributed to diet?
|
35%
|
|
|
What experimental evidence is there against GMO's?
|
Rats refused to eat genetically modified tomatoes at 1st and then started displaying proliferative cell growth when forced to eat it
|
|
|
How will our corn GMO's able to resist insects normally? What is their mechanism of insecticide?
How may this be a risk to us? |
They secrete BT toxin which pokes holes in the guts of insects, but may also poke holes in the guts of humans as well
|
|
|
Besides just directly getting BT toxin in our gut, what longer-lasting implication does GMO's have on our health? Mechanism?
|
Some bacteria can take up the BT toxin gene and start secreting it constituitively in our gut
|
|
|
What changed about our food composition that we tend to eat more now than we did in the 80s?
|
We talk all the fat out of food and replaced it with high fructose corn syrup, which is not as good of the satiety signal as fat
|
|
|
What is the glycemic index of flour compared to sugar?
|
It is the same because they are both absorbed just as rapidly
|
|
|
Why a high glycemic index foods cause diabetes?
|
They are constantly stimulating a huge amount of insulin release, which may lead to insulin resistance
|
|
|
What else does chronically high insulin lead to? (A process inside the body)
|
Chronic inflammation and all the diseases that come with it
|
|
|
What are some low glycemic index carbs?
|
Not whole-wheat, but beans, squash, and cracked grains
|
|
|
Give an example of a cracked grain
|
rolled oats, quinoa, Brown rice
|
|
|
What is the GI of glucose?
|
100 (the most you can have)
|
|
|
What is a quality of bread that tells you it is a higher GI index?
|
if you can roll it up into a ball rather than it being very crispy or billowy
|
|
|
What modification can you make the food to make the glycemic index higher?
|
If you just boil stuff for longer, the glycemic index rises
|
|
|
Is white rice or white bread a higher glycemic index?
|
White rice
|
|

|

|
|
|
How high glycemic index for normal cereal?
|
almost 100
|
|
|
How much is hummus?
|
6
|
|
|
Why do you think it is so low?
|
high fat content
|
|
|
What is the strategy for decreasing the glycemic index of normal foods?
|
Mix them in with some fat
|
|
|
What is the best predictor of of type II diabetes development? Why?
|
Intrahepatic fat because that indicates that you are putting into many cards for the liver to properly process into fat and it is backing up. That probably means that you have a lot of insulin in your blood.
|
|
|
Our animal proteins of free from pesticides?
|
No they actually concentrate environmental toxins
|
|
|
What are heterocyclic amines and how are they need?
|
This is that charred stuff that comes from cooking protein too heavily. It is carcinogenic.
|
|
|
What is the difference in nutritional content of farm fed fish and wild fish? Why?
|
Find fish have no more omega-3's then beef because they obtain their omega-3 is from food. Wild fish eat krill and algae to get omega-3's
|
|
|
What are the 3 locations of enzymes required for digestion in the small intestine?
|

|
|
|
The majority of the carbohydrates we taken are in what form?
|
Plant starch
|
|
|
What are the 2 types of plant starch? What is the difference between the 2? What are the similarities?
|
Amylose and amylopectin.
They both contain a-1,4- glycosidic bonds of glucose, but amylopectin (longer name) also has branch point at a-1,6 |
|
|
Which one is more prevalent of the 2 starches? Mnemonic?
|
Amylopectin because it has a longer name so it takes up a bigger proportion and also had the extra branches
|
|
|
What are the other 2 types of polysaccharide that are not as significant in our diet?
|
Animal glycogen and cellulose
|
|
|
What kind of cleavage will salivary amylase give?
|

|
|
|
What kind of products will come out of amylase (pancreatic and salivary are the same) starch digestion?
|
Since it can only leave internal a-1, 4 bonds, it can only give di or tri-saccharides of glucose and the branches on the end
|
|
|
What are the di or trisaccharides of starch called?
|
Maltose and maltotriose
|
|
|
What are the branched end chains of glucose called?
|
a-dextrins
|
|
|
What happens to these starch breakdown products after α-amylase gets to them?
|
They are broken down into glucose by enzymes in the brush border membrane
|
|
|
Which sections of the small intestine does this happen in?
|
The duodenum and the jejunum
|
|
|
What is the composition of lactose and sucrose?
Are there any pancreatic amylases that break them down? |
Lactose= glucose + galactose
sucrose = fructose + glucose No because these are disaccharides that must be handled at the brush border |
|
|
Do any disaccharides go inside the epithelial cells? What does?
|
No, only monosaccharides go inside the cell
|
|
|
Do monosaccharides come into the cell immediately? What has to happen?
|
no, after they are broken down, they must be transported
|
|
|
What is the special enzymatic property of maltase?
|
It is finally able to cleave That end a-1,4 glycosidic bond
|
|
|
What enzyme is able to handle the branched a 1,6 glycosidic dextrin?
|
isomaltase
|
|
|
what enzyme cleaves lactose and sucrose?
|
lactase and sucrase
|
|

|

|
|
|
Is there more glucose inside the epithelial cell or in the intestinal lumen?
What does this mean for how much work the transporters need to do? |
Much more inside the cell, Which means that we need to use active transport to bring it inside the cell
|
|
|
Which sugars have to go against a concentration gradient and which ones can just flow down it?
|
Galactose and glucose have to go against the concentration gradient
Fructose can just flow down its concentration gradient |
|
|
What is the active transport system that moves glucose and lactose into the cell?
|
Secondary active transport by hitching a ride with sodium down its concentration gradient created by the Na/K pump
|
|

|

|
|
|
Why is one transporter SGLT where is the other one is GLUT?
|
The stands for sodium, which means that it is a co-transporter
|
|
|
How were the GLUT transporters named?
|
In the order that they were discovered
|
|
|
What % of carbohydrates don't get absorbed in the SI?
|
5-15%
|
|
|
What happens to those unabsorbed carbs?
|
Bacteria in the colon get it hold of them and turn them into short chain fatty acids
|
|
|
Why are short chain fatty acids important for us?
|
They are important fuel for the epithelial cells of the colon
|
|
|
What is the law of movement in the intestine?
|
When there is pressure in one part of the intestine, the intestines contracts the segment behind and relaxes the segment in front so that it can move via peristalsis
|
|
|
What is the intestino-intestinal reflex?
What is it designed to protect you from? |
A protective mechanism or when there is overdistention of one part of the intestine. There are neural mechanisms that relax the segment in front to prevent rupture
|
|
|
Mnemonic for fructose apical transporter?
|
It is GLUT5
5 looks like F |
|
|
What is special about the GLUT2 transporter to for different sugars?
|
It has a low affinity for glucose
|
|
|
What does this mean about the conditions for glucose transport? Where is it present?
|
It will only transport glucose if the concentration gradient is very high. It is only present in the intestinal epithelial cells, pancreatic islet cells, and the liver.
|
|

|
D
|
|
|
Where is most of our protein absorbed?
|
before the mid jejuneum
|
|
|
What happens to slough off cells that come off before the mid jejunum?
|
We digest and absorb them like cannibals
|
|
|
What grains contain gluten?
|
Protein inside wheat, barley, and rye
|
|
|
Why do we put gluten inside of cooking?
|
to give things a elastic, chewy texture
|
|
|
What percent of people have a gluten intolerance?
What is special about gluten that elicits inflammation? |
6% of the population not including celiac disease
we cannot fully breakdown gluten so people tend to have immune responses to it |
|
|
Can anyone fully breakdown gluten?
|
no
|
|
|
What is the difference between gluten intolerance and celiac disease?
|
Gluten intolerance is community targeted at the gluten.
Celiac disease is an autoimmunity targeted at our cells that is exacerbated by gluten |
|
|
How long does gluten stay in the G.I. tract?
Why may this also negatively affect people? |
Longer than other nutrients, which means that it diverse blood flow from muscles and brain tissue (although the brain is supposed to have a very tight vascular autoregulation)
|
|
|
What percent of proteins are broken down in the stomach versus in the intestine?
|
At most, 15% of protein is broken down in the stomach
|
|
|
What form do proteases in the stomach and intestines break protein down into?
|
oligosaccharides
|
|
|
What are the oligosaccharides broken down into at the brush border?
|
AA's, di and tripeptides
|
|
|
How are the amino acids transported inside the cell?
How are the di and tri peptides transported inside? What happens to them afterwards inside the cell? |
Amino acids have their own special transporters
dipeptides and tripeptide share one transporter. Their breakdown to amino acids continues inside the cell. |
|
|
How many different amino acid transporters to we haven't the brush border?
What are the 2 different types? |

|
|
|
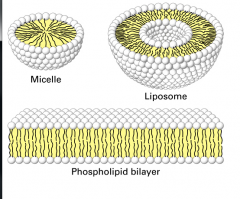
What is the difference between micelle and a liposome?
|
|
|
|
What role does the muscularis mucosa play in fat absorption?
|
Shakes up the unstirred layer so that the micelle can get even closer and release the fatty contents through passive diffusion
|
|
|
Is this necessary? Why?
|
The micelles can't passively diffuse unless they are really really close
|
|
|
What component of the bile secretion makes the outside of the miceele?
|
the lecithin (phospholipid)
|
|
|
What happens to the fats before they go into the endothelial cell? What are they broken down to?
|
They are broken down by pancreatic lipases into
1 triacylglycerol = 2 fatty acids + one 2 – Mono glyceride |
|
|
How are pancreatic lipases able to get access to the fats inside of micelles?
What 2 components are blocking them from the inside of the micelle? |
They sit on the surface of the micelle and another pancreatic enzyme called colipase will move the bile salts aside so it can get to the center
|
|
|
Without colipases, would lipases be able to work?
|
NOPE
|
|
|
What happens to the lipids after they enter the epithelial cells?
What organelles do they go to 1st? |
They are moved to the endoplasmic reticulum where they are reassembled into triglycerides
|
|
|
What happened after they are reassembled? What organelles do they go to?
|
They are sent to the golgi where they are combined with apolipoprotein to form chylomicrons
|
|
|
Compared to other lipoproteins, how big are chylomicrons?
|
They are the biggest.
|
|
|
How come chylomicrons don't go into the capillaries?
|
They are much too big for the capillaries and would rather be carried in the arteries
|
|
|
Where did the chylomicrons go?
|
They are picked up by the lacteal and then moved through the thoracic duct into the bloodstream
|
|
|
What happens to the micelles?
|
They continue on in the intestines and are reabsorbed in the terminal ileum
|
|
|
What kind of fats can go directly into the bloodstream?
|
The small and medium chain fatty acids
|
|
|
What does that look like when it 1st enters the duodenum and what does it look like by the time it reaches the jejunum?
|
It is in big droplets when it 1st enters, but then is a emulsified later on
|
|

|

|
|
|
What factor is the main driving force behind duodenal secretion of fluid into the lumen?
|
hypertonicity of chyme due to the leakiness of the tight junctions there
|
|
|
Describe the 2 steps in which sodium is absorbed from the lumen into the capillaries
Describe the one step in which water makes this journey |
Sodium is co-transported along with many things into the epithelial cell and then pumped out through the Na/K pump
Water just follow sodium through the trans-cellular route |
|
|
What 3 cotransporters get sodium through the apical side of the epithelial cell?
|
Glucose, some amino acids, and bile salts
|
|
|
What role do crypt cells have in fluid secretion? Why is this important to digestion?
|
The crypt cells will secrete sodium and chloride and water to follow.
This is necessary to dissolve amino acid and carbs for absorption |
|
|
What transporters are necessary to put sodium, chloride, and water out into the lumen of the intestine?
|
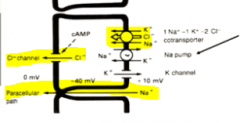
a Na/2Cl/K transporter on the basolateral side
a CFTR on the luminal side |
|
|
What 2nd messenger system activates the CFTR channel?
How can you use a certain hormone to remember this? |
cAMP
Secretinopens up the CFTR channel and its 2nd messenger system is cAMP |
|
|
What is the mechanism by which vibrio cholera can cause diarrhea?
What kind of diarrhea is this? |
It secretes cholera toxin which binds to and won't let go of a receptor that up regulates cAMP
Too much sodium, chloride, and water get secreted into the lumen and we have diarrhea This is called secretory diarrhea |
|
|
Mnemonic for cholera toxin 2nd messenger?
|
GaS canisters at the base cAMP
|
|
|
What simple solution did scientists develop save people from cholera without medication?
How does this work? |
Oral rehydration therapy- People can drink a solution of sodium and glucose.
Both these things are absorbed through the epithelial cell and will try water with it, negating the open CFTR channel causing water movement in the opposite direction |
|
|
How long do people need to do this? Why?
|
3-6 days until the intestinal epithelial cells with the toxins stuck on it is shed
|
|
|
Would people with CF get cholera diarrhea? WHy?
|
No because the cholera can't bind to their mutated CFTR channel
|
|
|
What if help people with 1 good copy of the CFTR channel and one defective copy? How much diarrhea will they get?
|
The same as a normal person because the osmosis pressures are still the same
|
|
|
Why is it so important to regulate our absorption of minerals?
|
Too much of them can be toxic to our bodies
|
|

|

|
|
|
What stimulates increase synthesis of Vit D?
|
Our need for calcium
|
|
|
What states would count as "needing more calcium"?
|

|
|
|
Do most of us have a calcium deficient diet?
|
yes
|
|
|
Why is our vitamin D levels so low then?
|
It must not be a perfect check and balance system then.
|
|
|
Is the intracellular concentration of calcium in an epithelial cell high or low? How do you know this?
|
low Because otherwise the cell would die
|
|
|
How is the intracellular calcium Low? (2 ways)
|
It is immediately bound to calbindin or put into vesicles
|
|

|

|
|
|
What role does vitamin D play in all this? (3)
|
Vitamin D acts by stimulating the synthesis of calbindin, calcium channels, and CaATPases.
It also opens the apical Ca channels |
|
|
Why doesn't calcium end up doing signalling by binding calmodium?
|
these epithelial cells absorbing Ca probably don't have as many calmodiums
|
|
|
WHat oxidation state is iron absorbed in?
How can you deduce this? |
Ferrous (2+) because the iron we eat is not red
|
|
|
How is iron taken into the cell and what are it's two options once it comes inside?
|
Ionic iron is absorbed as Fe2+ with the help of co-transporter Divalent metal transporter-1. Fe2+ can be stored intracellularly bound to ferritin or transported out of the cell by an ion transporter called ferroportin
|
|
|
What is the fate of iron that is bound to ferritin?
What phenomenon does this remind you of? |
It is stuck there and eventually the cell gets sloughed off with it when it dies
|
|
|
How are we able to regulate how much iron is absorbed?
How much ferritin is in an epithelial cell when we have to much iron in our blood? |
The liver secretes hepcidin which will bind to ferroportin and cause it to be internalized and degraded. Basically, we get less basolateral iron transporters
More iron will get backed up in the epithelial cell and be stored as ferritin |
|
|
How much iron is absorbed each day?
|
1-2mg
|
|
|
Where are minerals absorbed along the intestines? Why does this make sense?
|
In the very beginning in the duodenum because they do not need to be processed nor do they serve any further role
|
|

|

|
|
|
What is the role of the crypts versus the villi in electrolyte and water secretion and absorption and Mark
|
The crypts specific create all of the solution and the villi absorbed all of it.
|
|
|
Do the crypts secrete more or do the villi absorbed more? How do you know?
|
the villi absorb more there is overall fluid absorption in the small intestine
|
|
|
On a macroscopic level, why is there more fluid absorption in the small intestine?
|
You are absorbing single units all the nutrients so water will follow them
|
|
|
What is Hirshsprung's disease?
How do you get it? |
a congenital failure of neural crest cells to migrate completely, resulting in part of the colon being uninnervated
|
|
|
What part is usually uninnervated?
How does this section of the colon look and act differently? |
the end part with the internal anal sphincter
since there is no UMN innervation, it is shut tight |
|
|
What is another name for Hirshsprung's disease? Why is it called this?
|
congenital megacolon because people get super backed up and the colon distends
|
|
|
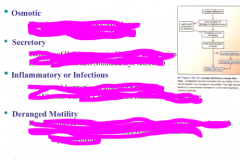
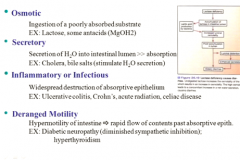
What are the 4 different types of diarrhea?
|
1. osmotic
2. secretry 3. inflammatory or infectious 4. deranged motility |
|
Describe each and give some examples.
|
|
|
|
WHat 2 substances can actually get absorbed in the stomach?
|
aspirin and alcohol
|
|
|
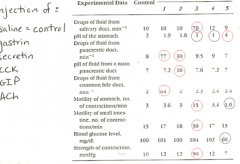
1- CCK
2- secretin 3- ACh 4- gastrin 5- GIP |
|
|
from this, what can you tell about the power of gastrin vs ACh in intestinal and gastric motility?
|
ACh is waaaayyyy stronger (but she says that this data may be faulty for gastrin's low effect)
|
|
|
Does secretin add more fluid to the pancreatic duct or CCK? Why?
|
secretin because it is involved in the ducts where water moves.
CCK is more hormone involved/ |
|
|
Accoring to this experiement, does secretin have any effect on the GB?
|
no.... (strange)
|
|
|
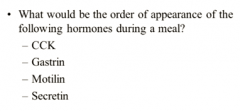
1. gastrin
2. secretin 3. CCK 4. Motilin |
|
|
What are the corners by which the LI hangs called?
|
right- heptatic flexure
left- splenic flexure names after the organs they are near |
|
|
What does the cecum and appendix loook like?
|

|
|
|
What do the longitudinal muscles look like in the LI? What are they called?
|
they are taeniae coli which are 3 bands of longitudinal muscle
|
|
|
What is mixing called in the LI vs the SI?
How are they different? |
Li- haustrations
SI- segmentation haustrations happen less frequently |
|
|
What are haustrations like? What muscles contract?
|
the circular muscles contract on either side like in segmentation, but the taeniae coli also contract and force the poop to mix in the three pouches (haustra)
|
|
|
What is the method of propulsion called in the LI vs SI?
|
LI- mass movement
SI- peristalsis |
|
|
describe how mass movement is different
|
it pushes contents a much further length
|
|
|
What 2 things are we absorbing and what 2 things are we secreting in the large intestine?
|

|
|
|
What hormone must be acting in the large intestine to mediate this ion exchange?
|
Aldosterone
|
|
|
What reflex initiates mass movements? How often should mass movments happen and what do they lead to?
|
gastrocolic reflex
they should happen 1-3 times/day and lead to a trip to the bathroom |
|
|
What electrlyte imbalance can we get from diarrhea? (2)
|
loss of bicarb and K
|
|
|
What relaxes the internal anal sphicter?
|
anything knocking on the door (pressure) will open it (reflex)
|
|
|
What happens To the feeling of having to go when we decide to contract our external sphincter?
long vs short term consequences? |
In the short term, the urge to go goes away
In the long term, we get constipated because we aren't to to the signals to go |
|
|
What is the main Cause of constipation in children?
What happens to the quality of the feces when we hold it in? |
voluntary retention (anal retentive children)
it gets dried out by sitting there and getting water reabsorbed for too long |
|
|
What age related anatomical change in the intestines can result in the following:
flatulence diverticulitis bowel incontinence intestinal infections longer transit time |
flatulence- decreased digestive enzymes and thinning of villi giving more fodder to colon bacteria
diverticulitis- decreased elasticity of rectal wall bowel incontinence- decreased internal anal sphincter tone intestinal infections- decreased mucous production longer transit time- atrophy of muscular layer |
|
|
What are the two main things that decrease in absorption as we get older? (nutrient and vitamin)
|
fats and B12
|
|
|
What is one explanation for why old people get constipated?
|
they neural impulses are dulled and they don't sense the urge to defacate as much
|
|
|
3 consequences of dullled neural transmission on pooping.
|
1. bowel incontinence- don't close sphincter in time
2. incomplete emptying- muscularis externa is weak 3. constipation- decreased evacuation reflex |

