![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
60 Cards in this Set
- Front
- Back
|
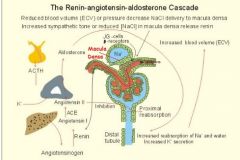
What is role of renin-angiotensin-aldosterone system (RAAS)?
|
RAAS plays important role in regulating blood volume and SVR, which together influence CO and arterial pressure.
Essentially, their primary function is to incr. H2O and NaCl reabsorption. |
|
|
macula densa
where located? |
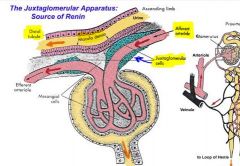
area of closely packed specialized cells lining DISTAL TUBULE (ascending loop) where loops back adjacent to vascular pole (afferent and efferent arteriole) of parent glomerulus,
|
|
Cells of macula densa are packed in distal tubule where runs near glomerus & JG cells between AA and EA.
Regarding the function of the macula densa cells... ►What tubular fluid change (stimuli) do these cells respond to? ►Macula densa cells and JG apparatus respond to these changes through what 2 mechanisms? |
* Macula Densa cells respond to Na & Cl ion levels in tubular fluid (osmoreceptors).
* If reduction in tubular NaCl detected by MD cells -> produce molecular signals --> stimulating (1)renin release from nearby JG cells into circulation Also (2)afferent arteriole will dialate as part of intrinsic regulation of GFR. (effects explained in later question) |
|
|
So renin is released by macula densa cells??
|
No!...renin release from nearby JG cells into circulation
|
|
|
Peritubular capillary pressure (capillaries around renal tubules) is higher OR lower than other capillaries in body?
|
LOWER blood pressure than other capillaries in the body; supports reabsorption!!!
|
|
|
Is Na+ conc. higher in tubular cell (epithelium lining tubules) OR is it higher in interstitium?
Why significant? |
Sodium conc. higher in interstitium. Therefore, Na+ must be actively transported (Na/K pump) in order to move ions from tubular cells into interstitial fluid, etc.
However, it passively moves from tubular lumen into epithelium, and from interstitium into peritubular capillary. |
|
|
How are MD cells involved in autoregulation of GFR?
|

Tubulooglomerular feedback mechanism:
When GFR high, insufficient time for peritubular capillaries to reabsorb, and concentration of solutes in tubules stays high. MD stimulated and somehow vasocontrictors (of afferent arteriole) released . |
|
|
Again...JG cells contain what? Where located?
|

•JG cells (granular) contain RENIN
•Located in smooth muscle near arteriole walls |
|
|
HA (weak acid) <-- ---> (H+) + (HCO3-)
Weak acid is only partially dissociated in solution.. What happens when more H+ is added to solution? |
Reaction shift to left
More undissociated HA |
|
|
HA (weak acid) <-- ---> (H+) + (HCO3-)
Weak acid is only partially dissociated in solution.. What happens when H+ is taken from solution (e.g. by kidney)? |
RxN shifts to right
More demand for dissociated H+, cause more bases and/or anions will be present |
|
|
What are 2 of most important intracellular buffers?
|
proteins e.g. hemoglobin
also phosphate (as urinary buffer) |
|
|
What is only open buffer system in body?
|
bicarb system, b/c both components are regulated
(expand on this further) CO2 by lungs HCO3- by kidney |
|
|
Respiratory acidosis occurs when..?
|
lungs NOT removing CO2 quickly enough
for example after hypoventilation |
|
|
Respiratory alkalosis occurs when..?
|
lungs removing CO2 faster than it can be produced
e.g. in hyperventilation |
|
|
Drop in plasma K+ (hypokalemia) causes...
|
K+ must leave cells, coupled with H+ influx. Change in intracellular H+ leads to secretion of H+ into tubule/urine, b/c some + has to leave to make room for K+...Thus metabolic alkalosis arises due removal of H+ ions.
Conversely, hyperkalemia leads to metabolic acidosis |
|
|
Increased aldersterone concentrations do what to K+ secretions?
What is end result? |
increase them, filtration incr and peritubular capillaries can only reabsorb so fast :(
this leads to hypokalemia (metabolic alkalosis - which is also b/c Na+ reabs and H+ leaves p.445) |
|
|
Glom.filtration is ______ process in which H2O and nearly all subst. in plasma move together (not really selective permeable).
|
bulk flow process p.372
reabsorption on other hand is a selective process |
|
|
How do u calculate [renal] plasma flow from [renal] blood flow?
|
Need to know hematocrit.
Multiply 1-HCT% by volume of blood. e.g. 1000ml/min * 0.6 = 600ml/min |
|
|
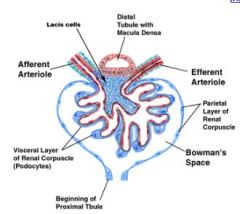
Which structure(s) appears first on tubular system: peritubular capillaries OR juxtamedullary apparatus?
|
peritubular capillaries; wraps around PCT
JGA (site of JG and MD cells) is where distal tubule runs between efferent and afferent arteriole. |
|
|
What is descending LoH impermeable to?
|
Na+
(but 2/3 leaves before LoH in PCT) |
|
|
What is ascending LoH impermeable to?
|
H2O
|
|
|
What is osmolarity of tubule entering LoH?
What is osmolarity of tubule leaving LoH before DCT? |
300
100 Then it goes way up in collecting duct as H2O leaves, amount depending on how much ADH acting on it... |
|
|
Approx. how much blood is filtered by kidney (dog) per minute?
|

80L/24 hrs OR 50mL/min (i believe)
|
|
|
Where part of tubule does alderstone act on?
What does it incr? Decreases? |

• Aldersterone is most important determinant of renal Na+ reabsorption
...Aldosterone is a SODIUM SAVER...remember A-S-S • acts on DISTAL tubule and collecting duct • Increases NaCl and H2O reabsorption....decreases K+ reabsorption |
|
|
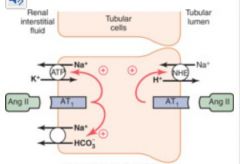
Where on tubule is AT2 act?
What does it incr? decr? |
AT2 stimulates secretion of aldersterone
PT, thick ascending, LoH, DT increases NaCl and H2O resorption in 2 ways 1. (indirectly by stimulating release of aldrerstone) 2. constricting afferent / efferent arterioles, reducing pressure in peritubular caps., promoting reabs. (for whatever reason, book says doesn't have much affect on GFR) Decreases hydrogen (b/c its puumped back in) Easy. You reabsorb Na+, then water and other solutes follow. |
|
|
What part of renal tubule does ADH act on?
What does it incr? decr? |

acts on distal tubule and collecting duct
increases H2O reabsorption |
|
|
ANF is what? Opposes what?
Decreases what? |
diuretic which opposes aldersterone
decreases salt, H2O absorption |
|
|
PTH acts on what part of tubular system?
stimulates abs. of? decreases reabs. of? |
PT, thick ascending, LoH, DT
increases calcium abs. decreases phosphate reabs, b/c binds with H+ and gets excreted |
|
|
Which cells contain renin?
What kind of cells are they? Describe them. |
Juxtaglomerular cells (or granular cells) are smooth muscle cells on afferent arteriole...JG cells stimulated by MD cells.
|
|
|
What stimulates release of renin? (name three factors)
|
decr in blood vol
In more detail: Peptide hormone is secreted by kidney from specialized cells called granular cells of JGA via 3 responses: * 1) A decrease in arterial BP (that could be related to a decrease in blood volume) as detected by baroreceptors (pressure-sensitive cells). This is most causal link between BP and renin secretion (other two methods operate via longer pathways). * 2) A decrease in NaCl levels in ultra-filtrate of nephron. This flow is measured by macula densa of JGA. * 3) Sympathetic nervous system activity, which also controls BP, acting through beta1 adrenergic receptors. |
|
|
1. Define renal clearance:
2. if "creatine clearance is 120", what does this mean? |
1. Volume of plasma cleared of substance (e.g. creatine) per minute
2. clearance of 120 = 120mL of plasma cleared of creatine per minute |
|
|
What substance gets excreted at 100% of volume entering filterate and secreted actively from peritubules (100% remaining renal plasma flow) until carriers are saturated?
|
PAH
fyi: can be used to calculate renal plasma flow b/c all PAH that flows through glomerulus (remainder secreted) is excreted; clearance of PAH (Cpah) = RPM |
|
|
What is formulas for renal clearance?
|
Clearance = urine conc. (mg/mL) x urine flow (mL/min) / plasma conc. (mg/mL)
|
|
|
Why is creatine great indication of GFR?
|
Produced by body and filtered 100%, but not secreted or reabsorbed.
|
|
|
Sample question:
PAH plasma conc. 0.2mg/ml PAH urine conc. 120mg/ml urine flow of 1mL/min HCt = 0.4 > determine renal BLOOD flow: |
Clearence = 600ml/min <plasma flow
(600ml/min) / 0.6= 1000ml/min renal blood flow |
|
|
clearance ratio
if clearance is greater than 1 if clearaance is less than 1 |
filtered and secreted
filtered and absorbed |
|
|
Approximately what percentage of plasma passing through DOG kidney is filtered thr. glomerulus?
|
25%, generate 55ml of filtrate per minute from 220ml of plasma (400ml of blood).
Remaining 165 ml (75%) goes to peritubular capillaries. (horse filters only 10%) |
|
|
3 layers of glomerular "filter"?
|
1. endothelium
2. podocytes 3. basal lamina (basement membrane) |
|
|
3 physiological mechanisms or conditions affecting GFR
|
1. autoregulation
2. angiotension 2 - 3. sympathetic nerve fibers |
|
|
Where are Na/K pumps located on renal tubules?
(And more specifically where in cell membrane?) |
Unlike most cells in body, Na/K pump not evenly distributed in cell membrane of renal tubular cells. Only present on basolateral membrane (NOT apical/luminal side).
Found on PT (primary location near peritubular capillaries), ascending limb of LoH, and of course DT. |
|
|
Challenge Question:
An increase in plasma K+ has what affect on aldersterone? What negative effects does hyperkalemia (high K+ in blood) have on heart? |

Aldersterone is SODIUM SAVER and stimulates K+ secretion;
K+ conc. should be higher in cells, not interstitium or plasma. If too high in plasma, can cause heart arrhythmias and weak heart contractions. See page 451 in text. |
|
|
3 hormones that act of DT and collecting duct
|

ADH, ANF, aldersterone
fyi: in pic adh = avp |
|
|
Describe mov't of urea during "recycling" routine?
Significance or purpose of this? |
DT and proximal (top) of CD impermeable to urea, so only H2O leaves. Osmolarity of CD increases as goes down. However, urea is able to get out on distal end. It moves towards and reenters tubular system at ascending loop.
In process it manages to redirect the flow of interstitial NaCl back towards blood. RECYCLING OF UREA SAVES NACL...from being ****** out. |
|

1. 90% of biocarbonate (HCO3-) is reabsorbed in ________. Reabs. motivated by secretion of ______ into tubular lumen.
2. Diffuses easily thru _______membrane as CO2. 3. Bicarbonate returns to blood via ______ together with Na+ |

1. 90% of biocarbonate (HCO3-) is reabsorbed in PROXIMAL tubule. Reabs. motivated by secretion of [H+] into tubular lumen.
2. Diffuses easily thru APICAL (LUMINAL) membrane as CO2; H+ (not sure about relationship there) <- maybe b/c doesn't form CO2 unless H+ binds to bicarb (HCO3-) 3. Bicarbonate returns to blood via symport together with Na+ |
|

Bulk [flow] takes place in ______ and ______.
|

PT and LoH
(mostly PT - 2/3 H2O and Na+, 100% of glucose and amino acids) |
|
|
Strong acid dissociates ______ in solution into H+ and an anion. This anion is called ______.
|
Strong acid dissociates almost completely into H+ & anion; anion is called a [conjugated base]
In aqueous solution almost all H+ is dissociated, and only if H+ conc. increases(added) then is H+ forced back into binding. |
|

If acid accumates and pH drops, which form becomes more prevalent (associated or dissociated)
|
reaction moves to left
more H+ means more substrate for HCO3- to bind to |
|
|
Phosphate Buffers are usually in blood or inside cells?
|
not in blood; prevalent inside cell
|
|
|
RPF (mL/min) / 1 - HCT
tell you what? (check this) |

basically this is just formula for converting plasma clearance rate (ml/min) to blood clearance rate (ml/min)
need to know the hematocrit (percentage of blood which is cells or not plasma) helps to know RPF RPF = urine conc x urine flow rate / plasma conc |
|
|
Renin release from JG cells is stimulated by ? (name three primary stimuli)
|
Release is stimulated by:
1. sympathetic activation by B1 2. renal artery HYPOTENSION 3. decreased Na+ delivery to distal tubules of the kidney. FYI: remember decr. BP & volume = leads to reduced GFR, reduced water and NaCl loss into urine. |
|
|
Renin stimulates release of ___ from blood and tissues.
|

Renin stimulates the formation of ANGIOTENSIN-1 in blood and in tissues (A1 then converted to A2 in lungs and other tissues)
|
|
|
Angiotensin II (A2) has many functions:
1. stimulates the release of ___ from adrenal cortex 2. Stimulates release of ___ from posterior pituitary gland |

1. Angiotensin II stimulates release of ALDOSTERONE from adrenal cortex.
2. Stimulates release of (ADH) from posterior pituitary |
|
|
Which hormone also has following affects:
3. Stimulates thirst centers within the brain (polydipsia) 4. Facilitates norepinephrine release from sympathetic nerve endings, enhancing sympathetic (adrenergic) effects |
Angiotensin II --> polydipsia, NOR release
in addition to aldersterone and ADH... |
|
|
ADH is also known as ?
|
ADH = vasopressin
|
|
|
ADH released from ?
|
ADH is released from posterior pituitary gland
|
|
|
ADH stimulates? function?
|

Vasopressin (ADH) from posterior pituitary, increases fluid retention by the KIDNEYS.
|
|
|
what 2 things stimulate the adrenal cortex to make aldosterone?
|
- ATII
- hyperkalemia |
|
|
what does aldosterone stimulate?
|

stimulates NaK ATPase pump
- retain Na - secrete K ...Aldosterone is a SODIUM SAVER...remember A-S-S |
|
|
For more Renin-angiotensin-aldersterone system info...
http://www.cvphysiology.com/Blood%20Pressure/BP015.htm |
http://www.cvphysiology.com/Blood%20Pressure/BP015.htm
|
|
|
What is end result of A2 induced norepinephrine release on systemic BP?
|
cddvdvfbvfdbd
|

