![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
244 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Exposure Required for Satisfactory Images: Photospot
|
1 mgy; less than film, more than cine
|
|
|
|
Exposure Required for Satisfactory Images: Cardiac cine
|
0.2 mgy (10x fluoro - one chest-xray per image)
|
|
|
|
Exposure Required for Satisfactory Images: Fluoro
|
0.01 - 0.02 mgy per image
|
|
|
|
ESE and effective dose for:
- CXR - CT Chest (effective) - Skull XR - CT Head - KUB - Abdominal CT - Lumbar spine - Nuc med average effective - PET average effective - Cardiac cath/cerebral angiography effective - Abdominal angio effective - IVP effective |
- CXR: 0.1 mGy/0.02 mSv
- Skull XR: 1.5 mGy/0.15 mSv - AXR: 3 mGy/1 mSv - VCUG - 2 mSV - IVP - 3 mSv (ie. 3 KUBs) - PET - 4 mSv - Nuc med - 5 mSv - Lumbar spine: 10 mGy/2 mSv - CT Head: 50 mGy/1 mSv - Cardiac cath/cerebral angio - 0.2 mGy per sec / 7 mSv - CT chest: 10 mSv - CT Body: 30 mGy/10 mSv - Abdominal angio - 20 mSv |
|
|
|
Increase pitch to 1.5 does what to dose
|
reduces by 33%
(1/1.5 = new dose) |
|
|
|
Whole body dose for:
- LD 50/2 - LD 50/5 - LD 50/60 - cataracts - acute/chronic dose - low sperm count/sterility - erythema - transient/main - epilation - temp/permanent - desquamation - dry/wet - chronic radiation dermatitis (cumulative dose) - chromosomal aberrations - low lymphocytes - genetic doubling dose - genetically significant dose - public general dose limit - public eye dose limit - public organ dose limit - public dose limit for radiation exposure from x-ray facilities (mSv) |
- LD 50/2: 100 Gy (cerebral edema)
- LD 50/5: 10 Gy (GI failure) - LD 50/60: 3.5 Gy (Heme failure); 8 Gy with treatment - skin necrosis: 30 Gy - vascular damage: 20 Gy - chronic radiation dermatitis - 20 Gy cumulative - desquamation - 10/15 Gy dry/wet - cataracts: 2/5 Gy (similar to erythema) - low sperm count/sterility: 0.150 Gy/5Gy - erythema - 2/6 Gy transient/main - epilation - 3/7 Gy temp/permanent (get red before you lose your hair) - chromosomal aberrations - 0.25 Gy - low lymphocytes - 1Gy - Genetic doubling dose - dose to double spontaneous mutation rate - 1 Gy - Genetically significant dose for entire population - 0.25 mGy - Public dose limit - 1 mGy - Public eye dose - 15 mGy (10%) - Public everything else - 50 mGy - public dose limit for x-ray facility exposure <1 msv/year |
|
|
|
Increasing each of the following has what effect on SNR with MRI
- slice thickness - matrix size - RF bandwidth - Magnetic field strength - Square of Nex - Size of coil |
- slice thickness will increase SNR
- matrix size will decrease SNR - RF bandwidth will decrease SNR - Magnetic field strength will increase SNR - Square of Nex will increase SNR by increasing number of acquisitions - Size of coil will decrease SNR Equation (p. 367 Bushberg) SNR = voxel size* (PE * Nex/bandwidth)^1/2 * field strength Voxel size = (FOV^2/matrix^2) * slice thickness |
|
|
|
In MRI you can increase Spatial Resolution by doing what to each of the following:
1. FOV 2. matrix size 3. pixel size (FOV/matrix) 4. gradient field strength 5. Receiver coil character 6. Sample Bandwidth 7. Signal to Noise |
Increase Spatial Resolution by:
1. FOV Decrease 2. matrix size Increase 3. pixel size (FOV/matrix) Decrease 4. gradient field strength Determines field of view 5. Receiver coil character 6. Sample Bandwidth increase at expense of time 7. Decrease |
|
|
|
Definition of a watt
|
1 joule/second
|
|
|
|
Low frequency radiation has what type of wavelength
|
Long
|
|
|
|
Equation for photon energy
|
E = 12.4/λ
|
|
|
|
Reducing II size has what effect on magnification
|
Increases magnification (loss of minification)
|
|
|
|
What are the three components of spatial resolution in image quality in x-ray
|
Focal spot, motion (exposure time), and receptor size
|
|
|
|
Low photon energy in mammography is done by what combination of filters?
Does this affect contrast or resolution? |
Mo/Mo
Contrast (reduced scatter) |
|
|
|
What types of grids are used in mammography?
What is a typical grid ratio What is a typical Bucky factor |
Carbon fiber or cellular grids; aluminum would attenuate too many low energy x-rays
Typical grid ratio is 5:1 (as opposed to 10:1 in regular x-ray) Bucky factor 2 |
|
|
|
Optimal film density in mammography
|
Between 1.6 and 2.0
|
|
|
|
What type of film γ is used in mammography
|
High film γ to achieve high film contrast
|
|
|
|
Nyquist frequency
|
Frequency beyond which information regarding images cannot be obtained
1/2 * sampling frequency |
|
|
|
Typical TV line pairs
|
250
(actual resolution is 0.7 x 250 due to Kell factor) |
|
|
|
Pet system with 5 mm FWHM can resolve how many line pairs per mm
|
1 / (2 * FWHM)
0.1 lp/mm |
|
|
|
100 Bq in the lung decays with effective half life of ten seconds; how many total transformations
|
10 1/2 lives to complete decay
10 * 100 Bq * 1.44 = 1440 |
|
|
|
What is emitted with 99Tc decay
|
Gamma leaves, as its leaving it can knock out an inner electron; outer shell falls in so you get a characteristic x-ray or Auger electron
|
|
|
|
How to calculate decay constant λ in nuclear medicine
|
λ = 0.69 / T 1/2
|
|
|
|
What are the photomutiplier tubes in PET? (thickness and material)
|
3 cm thick Bismuth Germanate
|
|
|
|
What is the definition of S factor in nuclear medicine
|
Dose to target organ (t) from activity in source organ (s)
Obtained by dividing the absorbed energy by the target organ mass |
|
|
|
What is the equation for cumulative dose in an organ (ie. the thyroid) after nuclear medicine scan?
|
1.44 * f * A * Te * S factor
1.44 FATES where Te is effective half life, A is activity, and f is fractional uptake S factor is dose to target organ from activity in source organ |
|
|
|
mix and match
Electron capture Isomeric Transmission Beta decay 67Ga, 111In, 123I 131I, 133Xe 99mTc |
Electron capture – 67Ga, 111In, 123I – all made by cyclotron
Beta negative emission 131I, 133Xe - made by fission Isomeric transmission 99mTc (ie. Its metastable; the ‘ideal’) - |
|
|
|
FWHM of 8 mm, means what limiting spatial resoution
|
1 / (2 * 8)
0.06 lp/mm FWHM is mm/line lp/mm is double the inverse |
|
|
|
How often & in what manner are the following dose calibrator QCs done?
- Accuracy - Linearity - Constancy |
Accuracy - annually using calibrated source (have to compare two machines)
Linearity - quarterly measuring 99Tc decay over 72 hours (takes 3 days) Constancy - daily; using 137-Cs due to its long half life |
|
|
|
Intrinsic versus extrinsic flood checks in scintillation camera QC in PET
- How often and how? |
Daily; place large 57-Cobalt disc or tiny point source in front of camera
Intrinsic - performed without the collimator; assess NaI crystal and light detectors Extrinsic - done with the collimator |
|
|
|
Pulse height analysis in nuclear medicine
- what is it - what effect does it have on time of scan and image quality |
Electronic device determines which part of spectrum used to make images; maximizes photopeak events while minimizing Compton scatter
- wide window has more scatter photons but completes exam in shorter time |
|
|
|
In nuclear medicine, effect of diverging versus converging collimators on field of view as a function of distance
|
Converging collimators have smaller field of view with more distance
Diverging collimators FOV larger with more distance |
|
|
|
Direct versus indirect radiation - ratio
|
Direct - when Compton/photoelectrons directly interact
Indirect - interact with water to make free hydroxyl ratio is 2/3 indirect and 1/3 direct |
|
|
|
Equivalent dose formula for biologic damage
|
Equivalent dose = Dose * weighting factor
H = D * Wr Wr for x-rays is 1 Wr for alpha particles is 20 |
|
|
|
LP/mm for the following
screen film mammo screen fim digital cxr digital photospot/DSA flouro CT |
screen film mammo - 12
screen film - 6 digital cxr - 3 digital photospot/DSA - 2 flouro - 1 CT - 0.7 |
|
|
|
Doubling the matrix size in digital images has what effect on sampling frequency and spatial resolution
|
It doubles the sampling frequency
sampling frequency/2 = Nyquist frequency (limiting spatial resolution) so it doubles spatial resolution |
|
|
|
CT increasing field of view has what effect on axial resolution
|
Decreases resolution because more pixels represent a certain amount of tissue
|
|
|
|
Relationship between FWHM and LSF
|
FWHM ~1/2 * LSF
LSF width is a measure of blur |
|
|
|
Types of interactions at x-ray tube
Types of interactions at soft tissue |
At tube (tungsten or molybdenum): BC CharacteristicBrehm
Brehmstrahlung (majority) - braking electron with energy lost expressed as x-ray photon that shoots out, removed by x-ray filter b/c degrade contrast Characteristic x-rays - incident e- knocks out K-shell electron; excess energy as Auger or x-ray At tissue? |
At tissue: CoCoP
Compton - x-ray photon turns into scattered photon and scattered electron Coherent - no energy transfer; x-ray changes direction Photoelectric effect - x-ray photon knocks out k-shell electron; excess as Auger or x-ray |
|
|
Typical CXR filter - size and material
|
3 mm of aluminum
|
|
|
|
Heel effect how affected by:
- anode angle - SID - field size |
Decrease anode angle to increase heel effect
Decrease the SID to increase heel effect (obtain more of angulated x-rays) Increase field size (catch more of angulated x-rays) |
|
|
|
Purpose of grid?
Typical grid ratios in x-ray versus mammo? Bucky factor? |
Purpose is increase image contrast
Grid ratio: - 10 for x-ray - 5 for mammography - 5 also used for stationary x-ray units; higher ratios for higher kV) Bucky: x-ray 5 versus mammo 2 |
|
|
|
Relationship between absorbed dose and exposure
|
D = R x K
K = Kerma R = quality factor based on x-ray photon keV and tissue type (fat absorbs less) |
|
|
|
Effective dose
|
multiplies average absorbed dose in each organ group
|
|
|
|
Intensifying screen
- advantage and disadvantage - thick screen versus thin screen - material |
Advantage: Film alone has very poor absorption efficiency for x-rays (1%); screens improve efficiency and reduce radiation exposure; usually amplifies by 50-fold
Disadvantage: Comes at the cost of image quality; increased mottle due to less dose - Thick screens are faster but lose spatial resolution due to light diffusion causing quantum mottle - Made from rare earths (lanthanum blue, yttrium violet, gadolinium green, calcium tungstate not used) |
|
|
|
Screen efficiency equation in casettes
|
ε = α ∗ κ
Efficiency = absorption efficiency * conversion efficiency How much light is absorbed and how much is converted Higher absorption efficiencies have more mottle |
|
|
|
Air kerma for adequate:
Mammo Extremity x-ray CXR |
200 μgy
20 μgy 5 μgy |
|
|
|
Digital radiography detectors - 3 direct, one indirect
Which is used in CT? |
- Gas chambers with xenon and high voltage
- Solid state detectors - ie. PSP; crystal structure with electrons in different energy bands; PSP (CR) store it in electron traps until released by light Cadmium tungstate solid state detectors are used in CT - Scintillator/phosphor - Cesium Iodide; emits light when exposed to x-ray - Photoconductor - (DIRECT) amorphous Selenium; direct light detection with voltage across |
|
|
|
Mechanism of analog to digital conversion for film
|
- Narrow laser light beam digitizer (more accurate)
- CCD digitizer (cheaper, low maintenance) - also used in fluoroscopy |
|
|
|
How many megapixels in monitors
|
2 for nuclear
3 for film 5 for mammo |
|
|
|
HVL in:
- mammography - x-ray - CT - soft tissue |
- mammo: 0.3 mm Aluminum (although Carbon is used)
- x-ray: 3 mm Al - CT: 6 mm Al - soft tissue - 3 cm ? |
|
|
|
Mammography screen film
|
rare earth (gadolinium oxysulfide)
|
|
|
|
Mammography
- phantom evaluation - fixer retention quarterly - repeat analysis - QC physics testing |
- phantom checked weekly
- repeat analysis (all films that required repeat exams) are evaluated quarterly - fixer retention quarterly - repeat and fix once a quarter - physics QC - checking sensitometry strips to assess HVL, kV, collimation, AEC checks; done annually |
|
|
|
Mammography grids interspace material
|
- Carbon filters or air interspaced cellular grid
- used instead of aluminum so don't remove low attenuation x-rays |
|
|
|
Relate SNR to dose, pixel size and slice thickness
|
Jenn's equation:
D α SNR^2 / (pixel size^3 * T) D = Dose T = Slice Thickness |
|
|
|
what are dicentric chromosome
|
two chromosomes having double strand breaks and joining with one another
|
|
|
|
Chromosomal aberrations in stimulated peripheral lymphocytes reflect what
|
whole body dose in radiation
|
|
|
|
Most variable stage of cell cycle
|
G1
|
|
|
|
after partial killing of a cell population, the remaining living cells revert to synchronous phase of cell cycle, which one?
|
S phase (more radioresistant)
|
|
|
|
which part of GI tract most vulnerable to radiation
|
Small intestine is most vulnerable portion of GI tract to radiation
|
|
|
|
% of people that have nausea after 1 Gy exposure
|
30% of people have nausea after 1 Gy exposure
|
|
|
|
what dose for lymphocyte suppression and when
|
Lymphocytes drop 0.5 Gy; nadir a few weeks later
|
|
|
|
In ultrasound tissue attenuation is how much per mHZ
|
0.5 dB/cm per mHz
|
|
|
|
Doubling both ultrasound transducer and thickness has what effect on Fresner field
|
it increases it by two
Radius^2/wavelength wavelength increases by 2x with transducer thickness therefore near field increases by 4/2 or 2x |
|
|
|
Lateral resolution in ultrasound versus axial resolution
|
lateral resolution = axial resolution/4
|
|
|
|
all cancer risk per gray? per Sv?
|
All cancer risk per exposure is 4%/Gy or 8%/Sv and for leukemia 1%/Sv
|
|
|
|
Two ways to increase subject contrast for a given lesion
|
- higher kv
- adding filters |
|
|
|
Effect of averaging frames in fluoro on noise?
|
fluoro - reduces noise but introduces lag
|
|
|
|
3 ways to increase signal to noise ratio in MRI
|
- increase slice thickness (larger voxels per tissue)
- decrease matrix size (larger voxels per tissue) - increase Nex (increase by root 2) - decrease RF bandwidth (decrease by root 2) |
|
|
|
Cumulative activity in exponential decay
|
A = 1.44 [Ao * Te]
|
|
|
|
Wipe test - how to check
|
NaI well counter
|
|
|
|
Matching layer purpose in ultrasound and thickness
|
matching layer is an intermediate impedance layer between the transducer and the tissue
wavelength is 1/4 of sound in that material |
|
|
|
Ultrasound harmonics
|
- integral multiples of primary ultrasound pulse frequency
- receivers tuned to high frequency to eliminate noise at the cost of attenuation - requires very broadband transducers |
|
|
|
axial resolution in ultrasound determined by
|
axial resolution = 1/2 pulse length
better resolution at shorter pulse lengths; does not vary with depth |
|
|
|
Nyquist frequency - screen film or digital
|
digital images; limiting spatial resolution based on matrix sampling frequency
|
|
|
|
CT effect of smaller field of view on axial resolution
|
smaller FOV means better axial resolution (more pixels per voxel)
|
|
|
|
Entering different tissues, which properties of ultrasound change and which stay the same
|
velocity and wavelength change, frequency stays the same (still visit as often, but the quality of visits are different)
- wavelength decreases when velocity decreases (say hello less and drive less) |
|
|
|
Fresnel zone definition
|
r^2 / λ
r = radius λ = wavelength larger transducers and shorter wavelengths have larger Fresnel |
|
|
|
using multiple focal lengths changes what aspect of ultrasound resolution
|
lateral resolution (ie. ultrasound beam width changes with different focal lengths)
|
|
|
|
x-ray intensity - kvp vs mas
|
mAs directly, kvp^2
|
|
|
|
Purpose of filters in x-ray
|
reduce patient dose
reduced subject contrast by removing lower energy photoelectric x-rays increased x-ray scatter due to more compton absorption efficiency of image receptor decreases HVL increases |
|
|
|
chest wall is at which side to take advantage of heel effect in mammography
|
cathode (C & C)
|
|
|
|
What chemical side group is radioprotective
|
sulfhydryl
|
|
|
|
plastic attenuates which type of energy emission
|
beta minus (minimal bremstrahlung)
|
|
|
|
BGO vs LSO in pet
|
- both are scintillator detectors
- LSO (lutetium) has faster decay time than BGO (bismuth) - LSO has 5x better light production (75% vs 15%) |
|
|
|
Thymine dimers produced by what type of radiation
|
UV rays (UV on your thyghs)
|
|
|
|
Most variable phase of cell cycle
Most radioresistant phase Most radiosensitive phase |
- G1 - cell decides whether to enter S and make DNA (ie enter S)
- S is most radioresistant - M is most radiosensitive |
|
|
|
LET vs Energy
LET vs Mass |
LET decreases as energy increases
LET increases as mass increases high energy electron has the lowest LET |
|
|
|
stochastic effects - effect of increasing dose
|
severity of effect does not vary with dose although the probability of the effect does increase
|
|
|
|
nausea and vomiting following radiation
|
0.75 - 1.25 Gy n/v in 30% of exposed
1.25 - 3.0 Gy n/v in 60% of exposed |
|
|
|
risk per gray of cancer in acute exposure
|
8% per gray
|
|
|
|
risk estimate per sievert for hereditary effects of radiation
|
0.2%/Sv
|
|
|
|
acute versus chronic radiation exposure, how much does cancer risk increase per Sv
|
acute 8%/Sv
chronic 4%/Sv |
|
|
|
microcephaly sensitivity - when during pregnancy
|
40% at 8-15 weeks
less sensitive at 15-25 weeks |
|
|
|
stochastic effect has no threshold - t/f
|
true
|
|
|
|
equation effective dose with radiation exposure
|
absorbed dose * tissue weighting factor * radiation weighting factor
|
|
|
|
radon is responsible for what percentage of lung cancer deaths/year
what is its half life |
10% of lung cancer
half life = 3 days |
|
|
|
difference between effective dose and equivalent dose
|
effective dose - sum of equivalent doses, weighted for relative risk of cancer and hereditary effects for all tissue
equivalent dose = absorbed dose * radiation weighting factor committed equivalent dose = dosimetric term when source of radioactive material is within the body, integrated over 50 years |
|
|
|
stage 3-5 CKD what do you do with the gadolinium
|
cut it in half
|
|
|
|
specific absorption rate in MR
|
absorption of transmitted RF energy by tissue
|
|
|
|
ultrasound - time gain compensation definition
|
post processing where the recorded signal is amplified based on time delay since trasmitted pulse
|
|
|
|
ultrasound cavitation is more likely to occur at (high/low) frequencies
|
low (ie. barry manilow)
|
|
|
|
MI shouldn't exceed ___ in ultrasound and TI shouldn't exceed ___
|
MI 0.5 (half hearted attack)
TI 1.0 |
|
|
|
how to reduce chemical shift artifact in MR
|
- increase bandwidth (narrow your slice)
- lower gradient strength (decrease your frequency shift per proton) |
|
|
|
how to reduce metal artifact in MR
|
- decreases relative voxel size -- ie. decrease FOV or slice thickness
- you lose metal artifact at expense of decreased SNR; higher resolution is achieved at expense of decreased SNR - GRE sequences are most severely affected; metal is too GREy - spin echo less so; spin it off - short TE |
|
|
|
frame integration - digital fluoro vs mask subtraction
|
in digital fluoro, reduces noise
in mask subtraction, increases noise |
|
|
|
proton density images - TE/TR
Gradient echo - T1, T2 or T2* weighted? |
Proton density - short TE (<20 ms) to minimize T2 differences and long TR (>1000 ms) to minimize T1 differences
GRE - T2* weighted; use low flip angles and short TRs to emphasize T1 differences between tissues gradient echo - short TR; increase T1 differences; GRE are T2* weighted |
|
|
|
increase SNR in MRI
|
anything that increases relative voxel size - increased slice thickness, increased magnetic field strength,
|
|
|
|
high sensitivity versus high resolution collimators
|
high resolution have low sensitivity; used more often
|
|
|
|
2d vs 3d PET re:
- septal collimator rings - sensitivity to counts |
3D don't use septa (SIX TIMES higher higher sensitivity; coincidences are detected by multiple detector rings don't need to be removed by septa)
|
|
|
|
axial versus lateral resolution on ultrasound
|
axial resolution is based on pulse length
lateral resolution is based on beam width |
|
|
|
harmonic imaging
|
works at twice fundamental frequency
improved sensitivity to contrast agents (ie microbubbles) reflections are generated by large difference in acoustic impedance between gas and surrounding fluid/tissues |
|
|
|
power doppler
|
relies on doppler signal strength alone, ignores doppler shift; lose information about directionality
|
|
|
|
how is x-ray beam quality measured
|
in HVL units
higher quality means more penetrating x-rays and fewer need to be used overall; therefore lower radiation dose |
|
|
|
- HVL equation
- what is the legal minimum HVL |
0.69/μ
legal minimum is 3.0 mm aluminum |
|
|
|
units for RBE
|
RBE compares the ability of different types of radiation to cause biologic damage; based on linear energy transfer (keV/μm) of 250 kV x-rays/LET of specific radiation and therefore is a ratio without labels
|
|
|
|
how long to stop breast feeding after
- gallium scan - technetium pertechnetetate - iodine -indium wbc |
- gallium/thallium - 4 weeks/3 weeks
- technetium - 12-24 hrs (depending on dose) - iodine 131 - indefinitely for this child - iodine 123 - 1-2 weeks - indium - 1 week |
|
|
|
f-factor
|
conversion from exposure to absorbed dose; 3-4x in bone than it is in tissue
|
|
|
|
how to convert from absorbed dose to equivalent dose
|
multiply by quality factor QF (account for different types of radiation -- ie. 1 for x-rays, 10 for slow neutrons, 20 for alpha particles and fast neutrons)
|
|
|
|
equivalent dose to effective dose
|
multiply by weighting factor (same units, but different meaning)
|
|
|
|
absolute risk of cancer in fetus from 10 mgy
|
0.06% (relative risk 1.4)
|
|
|
|
what is the purpose of filtered back projection in ct
|
- with simple back projection there is an intrinsic blurring
- with filtered back projecting kernels, blurring is reduced |
|
|
|
Acquisition time in mR
|
Acquisition time = TR * # phase encoding steps * Nex
|
|
|
|
x - rays
↓ in mammography, what is the order of emulsion, base and screen |
x - rays
↓ Base Emulsion Screen BESt images possible |
|
|
|
1 curie (mCi) is how many transformations
|
37 billion transformations/s
1 Bq = 1 transformation/s |
|
|
|
penumbra calculation for object that is 5 cm but looks 9 cm with standard x-ray
|
P = (M - 1) x f
= 0.8 x 1.2 = 0.96 Therefore, blur increases with ___ and ___. M = magnification f = focal spot size |
Blur increases with increasing focal spot size and magnification.
|
|
|
isomeric transition definition
|
radioactive atom with excess nucleus energy
3 options - "AGEx" - Auger + electron (A) - gamma photon (G) - electron + x-ray (E-x) gamma photon comes out of nucleus (basically an x-ray, but from the nucleus) internal conversion electron is when a gamma ray knocks out an internal electron if outer shell electron fills inner shell of internal conversion electron, a characteristic x-ray can be produced conversion x-rays are monoenergetic, unlike beta particles if the characteristic x-ray knocks out an outer shell electron on its way out, that becomes an Auger electron |
|
|
|
what organization is responsible for premarket approval of all radiation emitting devices
|
CDRH, a branch of the FDA (regulate x-ray systems, ultrasound equipment, laser pointers)
|
|
|
|
for a count interval of 1 second, there is 10% uncertainty
count interval increases to 100 seconds, uncertainty decreases by what factor |
1/square root of N = relative uncertainty decrease
10%/10 = 1% is new uncertainty |
|
|
|
I 131 has what type of emission
|
90% beta and 10% gamma
avoid contact because I131 is secreted into urine, saliva and perspiration |
|
|
|
In an ultrasound image scanned with 250 lines per frame and 30 frames per second, how do you calculate maximum depth
|
assuming 13 μs per line
1/(13 μs/line) = 77k lines/sec (77k lines/sec)/(250 lines/frame * 30 frames/sec) = 10 cm *Basically it's 77k/(lines/frame * frames/sec) |
|
|
|
what causes geometric unsharpness in film
|
focal spot blur (reflex answer)
|
|
|
|
Define in cell survival curves
Dq Do n |
Dq = width of "shoulder" of radiation exposure that cells can endure sublethal damage before dying; it is zero for high LET radiation (DQ is sublethal)
Do = index of sensitivity of cells to radiation after Dq; reciprocal of slope n = number of critical molecular sites that need to be hit; y-intercept |
|
|
|
what device directly measures exposure
|
Ionization chamber directly measures exposure
NaI is indirect measure as a scintillator TLD indirectly measures exposure via heating |
|
|
|
high sensitivity collimators
high spatial resolution collimators high energy collimators |
high sensitivity = thinner and larger holes
high spatial resolution = longer holes; difficult to do with very thick septa high energy collimators (ie. 131 I) very thick septa to avoid septal penetration |
|
|
|
average HVL in soft tissue?
in mammo? set me which organization? |
3 cm (specified in Aluminum)
1 cm in mammo CDRH of the FDA |
|
|
|
compton scatter - energy of recoil electron is equal to the incident x-ray minus what
|
recoil electron = incident x-ray - scattered photon
|
|
|
|
TLD measures what quantity
a. dose equivalent b. effective dose c. absorbed dose d. KERMA |
a. dose equivalent -- absorbed dose x weighting factor (Gy x Wr)
|
|
|
|
what component is important when looking at low contrast structures on CT
|
CT image noise (standard deviation of CT numbers on phantom)
measured by uniformity phantom |
|
|
|
CT dose index definition
|
integrate axial dose profile (based on CT abdomen vs head, pitch, mA, scan time)
then divide integrated axial dose profile by *beam width* (ie. slice thickness) |
|
|
|
tomography principle
|
tomography means 'drawing of a slice
- move x-ray tube and cassette synchronously in opposite directions - the amount of movement for a specific fulcrum determines the tomographic angle and thickness of the 'slice' that is imaged - the larger the angle, the thinner the slice (jam on bread) |
|
|
|
scintillator camera resolution depends on two things
|
- resolution of the collimator
- intrinsic gamma camera resolution |
|
|
|
Coherent scatter accounts for what % of x-ray interactions in soft tissue
|
5-10%
|
|
|
|
f-number in fluoroscopy
|
- focal length/aperture diameter
- higher f number means decreased lens strength - when you narrow aperture diameter, you increase f-number and ABC increases exposure to compensate for decreased lens strength |
|
|
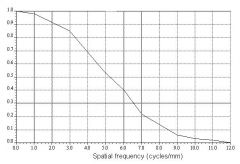
What does the y-axis represent and what is this curve?
|
MTF curve - a plot that shows resolution capabilities of system as function of spatial frequencies
Low spatial frequencies are large objects. |
|
|

|
Well counter
|
|
|

|
Thyroid probe
|
|
|

|
Dose calibrator on the left (bigger cylinder) and well counter on the right (a 'well' in the middle)
|
|
|
What is the artifact and how to reduce it?
|
Chemical shift
- Increase bandwidth (thinner slices) or lower gradient (less frequency induced per pixel) |
|
|

Artifact and how to reduce?
|

Gibbs/Truncation/Ringing
- bright or dark lines seen adjacent to borders of abrupt intensity change - increase number of encoding steps in Fourier transform |
|
|

What is it and how to reduce it?
|

Moire fringe - due to lack of homogeneity of magnetic field from one side to the other
- superimposed signals of alternating frequency; similar to looking through two screen doors |
|
|
|
Fingerprint artifact on mammo shows as bright or dark?
|

before exposure white
after exposure black |
|
|
|
scan time in MR
|
scan time * number of phase encodings * Nex
|
|
|
|
Radioactive decay curve and equation
|
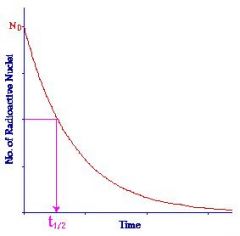
A = Ao * e^-λt
λ = 0.69/t 1/2 = decay constant take away the negative if you are going backwards in time to extrapolate an earlier value |
|
|
|
Linear attenuation coefficient curve and equation
|
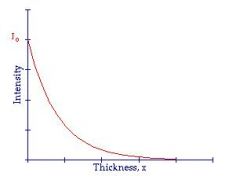
N = No * e^-μt
N/No = e^-μt Fraction of photons = N/No 0.69/μ = HVL μt = fraction of half value layer that you are traveling |
|
|
|
H&D Curve definition and image
|
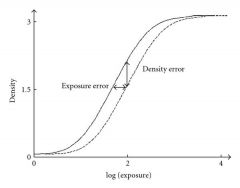
Characteristic curve showing relation between radiation intensity and optical density
|
|
|
|
Nuclear stability curve
|

|
|
|
|
Emulsion, base, screen order in standard film-screen.
|
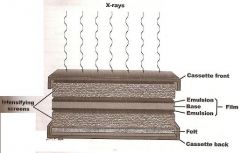
SEBES
|
|
|
|
Relate SNR to dose, pixel size and slice thickness
|
Jenn's equation:
D α SNR^2 / (pixel size^3 * T) D = Dose T = Slice Thickness |
|
|
|
How does heel effect change entrance to exit skin dose ratio?
|
Same as increasing filtration, it reduces it.
What effect does increasing SID have on heel effect? What effect does increasing anode angle have on heel effect? |
Increasing SID decreases heel effect because you lose outside part of the x-ray triangle (the scatter x-rays penetrate the patient)
Increasing anode angle decreases heel effect because you are making the > of the heel shorter. (High heels have more acute angles) |
|
|
Air kerma to get film OD of 1.5 in screen-film?
Air kerma to get film OD of 1.5 im mammography |
5 μGy
200 μGy (far higher exposure time, lower kV and mA) |
|
|
|
Double speed has what effect on radiation exposure
|
2x speed cuts radiation in half
|
|
|
|
1 Tesla is at larmour frequency for how many MHz
|
42 MHz
|
|
|
|
How many lp/mm for CT? for MR?
|
CT - 0.7 lp/mm
MR - 0.3 lp/mm |
|
|
|
Effects of added filtration
|
- decrease patient dose
- increase amount of scatter and reduce patient contrast because higher energy x-rays interact more by Compton than photoelectric - increased exposure time may be required to compensate for fewer x-ray photons, causing increased blur |
|
|
|
Collimation effect on scatter
|
Reduces scatter
|
|
|
|
Grids effect on scatter
|
Reduce scatter; increase dose, improve contrast (filtration reduces scatter but also reduces contrast)
|
|
|
|
Field of view effect on scatter
|
Increases with larger field of view; levels out at 1000 cm^2
|
|
|
|
Effects of grid placed:
- upside down - laterally decentered - distance decentered - combined lateral and distance decentered |
- upside down - center dark, periphery light
- lateral decentered - image uniformly decreased in density - combined lateral and distance - dark on one side and light on the other |
|
|
|
Intensifying screens trade what for what
|
reduced patient dose for reduced image quality
- reduction in radiation required increases quantum mottle - light dispersion in screen increases blur and reduces spatial resolution - based on this, why is only one screen used in mammography? |
- note: thicker (faster) screens and rare earth phosphors have higher conversion efficiencies --> increased patient blur 2/2 fewer total x-ray photons required
|
|
|
High temperature while developing has what effect on film-screen
|
Increases contrast (steepens H&D curve) at expense of reduced latitude
- Poor fixation has what effect on screen film - Delayed developer processing has what effect on screen film |
- poor fixation causes it to darken with time -- fixation is washing off unoxidized silver grains after development; if not washed off will 'fix' themselves with time
- opposite of delay in processing which is delayed oxidizing of film after x-ray exposure which causes latent image fading |
|
|
Calculate spatial resolution based on number of pixels and field of view
|
(1/2 * pixels) / FOV
ie. LP/FOV |
|
|
|
CR vs film screen
- radiation dose - spatial resolution |
CR
- higher radiation doses - lower spatial resolution (benefit is space efficiency, increased dynamic range) |
|
|

|
Contrast detail curve: Smallest detectable object diameters at various contrast levels
L-shaped curve |
|
|
|
Effective whole body dose limit to public?
Radiation worker whole body dose limit? Effective organ specific dose limit to public? Effective organ specific dose limit to radiation workers? |
Public:
- whole body: 1 mSv - organ specific: 50 mSv Radiation worker - whole body: 50 mSv - organ specific: 150/500 mSv |
|
|
|
What is the maximum depth of a 5 MHz probe in soft tissue?
|
Frequency (MHz)/Max depth (cm):
1/35 2/17.5 5/7 7/5 10/3.5 35/1 Always has to equal 1 (ie. MHZ to get to MTV) |
|
|
|
which have wider beam width in ultrasound -- low frequency or high frequency
|
high frequency have wider beam width, and therefore longer Fresnel zone:
Width = (1.2 * wavelength * focal distance)/diameter - Width of beam is inversely proportional to transducer diameter - narrow beam means better lateral resolution |
|
|
|
If a secretary is sitting in a room and a radioactive source next door decays at a rate of T1/2 10 minutes with an initial activity of 6 mGy/hr, what is her cumulative dose after 2 hours?
|
Assume complete decay so you don't need to incorporate T 1/2 into the cumulative dose equation.
Ac = 1.44 * A Teff Ac = 1.44 * 6 Ac = 8.6 mGy Easy peasy. |
|
|
|
What does an RBE curve look like?
|

|
|
|
|
When would a fan beam collimator be used in SPECT? (ie. for what organ studies)
|
Brain (small field size)
|
|
|
|
Ultrasound QC
|
Spatial resolution, TGC, contrast, dead zone, distance accuracy
|
|
|
|
LET curve?
|
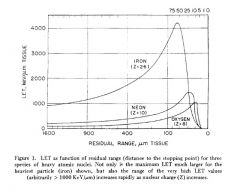
backwards L
|
|
|
|
Why does the heel effect decrease with longer SID?
|
Because the image receptor subtends a smaller x-ray angle (ie. as you get further, you receive less of the low attenuation x-rays)
|
|
|
|
Equation for SNR ratio in MRI
|
Chris's equation:
SNR α Voxel * (Nex)^1/2 / (BW)^1/2 * field strength Voxel = (FOV^2)/(pixels^2) * slice thickness FOV and pixels are the most weighted Slice thickness in the middle Band width and Nex are least weighted |
|
|
|
In an ultrasound image with 250 scan lines obtained at 30 frames/sec what is the maximum depth
|
Frame rate = 77/(sec * N * Depth)
where N = scan lines 250 scan lines/frame * 30 frames/sec 7500 scan lines/sec (which is the pulse repetition frequency) * Depth = 77000 Basically, 77k/(scan line frequency) = Depth Another name for scan line frequency is PRF Pulse repetition frequency = frames/sec * lines/frame = lines/sec |
|
|
|
Attenuation versus frequency in ultrasound
|
attenuation increases with increasing frequency
|
|
|
|
What determines section width in multislice vs conventional CT?
|
multislice - detector width
conventional - collimation |
|
|
|
Relate echo listening time to PRF
Relate PRF to depth How long does it take to travel 1 cm of soft tissue |
PRF is how much you talk.
Echo listening time is 1/PRF. PRF 4 Khz / Listening time 250 us PRF 10 kHz / Listening time 100 us PRF = scan lines/second (ie. how much you talk) Depth = 77,000/PRF The more you listen, the deeper you get. 1 cm soft tissue = 0.13 us |
|
|
|
Double wavelength in ultrasound, what happens to frequency and velocity
|
Velocity = frequency * wavelength
speed = how often * how long Double your length of visit, your speed of visiting has to cut in half. |
|
|
|
Effect on image quality of
- faster film - thicker intensifying screen |
- Faster film - increased quantum mottle (ie. contrast resolution)
- Thicker screen - decreased spatial resolution |
|
|
|
Compton scatter probability is greatest at what angle? Least at what two angles?
|
Greatest at 90 degrees.
Least at 0 and 180 degrees. |
|
|
|
Transformers require what type of current to function?
Transformers impact voltage or current? Then what has to change to compensate? |
- Alternating current
- Transformers impact voltage; consequently, current has to increase to keep VI = VI constant |
|
|
|
Molybdenum versus Tungsten for type of radiation produced.
|
Molybdenum is characteristic x-ray dominant (low Z)
Tungsten is brehmsstrahlung dominant (high Z) |
|
|
|
Heat units are the product of ___ and ___.
|
kVp and mAs
|
|
|
|
A certain high frequency generator can make a maximum of 600 mA at 100 kVp for a 100 msec exposure. What is the power rating of the tube?
|
Power RATING = VI where current is calcuated for 0.1 ms
= 100 kVp * 6 As * 0.1 sec = 60 kW (always convert to mA from mAs and period of time is always 0.1s by definition) |
|
|
|
Fast spin echo gradient manipulation
|
multiple phase encode gradients during the TR with multiple refocusing RF pulses to generate a train of up to 16 echoes
|
|
|
|
MRI order of encoding gradients?
|
-narrow band RF excitation pulse applied simultaneously with slice select gradient (determines slice thickness); longitudinal goes to transverse with a 90 degree flip angle causing the most transverse magnetization
- phase encode gradient is applied briefly to create differences along the phase encode direction, creating several views along y-axis of k-space - refocusing RF pulse is applied at TE/2 to reestablish phase coherence and make an echo at time TE - frequency encode gradient is applied during echo formation orthogonal to both slice encode and phase encode gradients; called the 'readout gradient' - ADC and Fourier transform massage the data into k-space |
|
|
|
Which pulse sequence uses low flip angles? Why?
|
GRE (at the cost of lower SNR and increased magnetic susceptiblity artifacts, similar to EPI)
- Low flip angle is because it uses a magnetic field gradient to induce the echo instead of the 180 degree pulses used in other sequences; smaller angles mean more transverse magnetization - Protons precess at slightly higher and lower frequencies along the gradient; this is then instantaneously reversed after a set period of time and produces a "gradient echo" |
|
|
|
Magic angle artifact in MRI
|
Water signal is seen in tendons due to an angle of about 55 degrees from the main magnetic field reducing inherent dipole causing a very long T2 signal
|
|
|
|
Two types of CT detectors
|
Cadmium tungstate (new) and pressurized xenon (cheap older model)
|
|
|
|
What filter reduces beam hardening artifact?
|
Bowtie
|
|
|
|
Negatron emission
- what is made? - what is the average energy of particles emitted? |
- occurs in neutron rich nuclei; get a neutron converted to proton, a negatron (electron) is emitted, and an antineutrino
- electrons have a range of energies with the average usually being 1/3rd of e-max - examples: 32P, 3H, 14C |
|
|
|
What determines spatial resolution in scintillation imaging?
How to check spatial resolution in scintillator imaging? What determines spatial resolution in SPECT? in PET? which is better SPECT vs. PET with regards to attenuation? |
- in scintillation imaging spatial resolution is based on:
1) collimator resolution (most important) 2) intrinsic resolution - crystal thickness (thin crystals are better) - average energy of photons up to 250 kEv; higher energy make more photons, leads to better resolution; after 250 this is offset by photon diffusing in crystal before photoelectric effect occurs - to check scintillator spatial resolution use image of a line source and determining line spread function (without collimators on) tells you intrinsic resolution; the collimator resolution is extrapolated based on this SPECT & PET re: spatial resolution - SPECT spatial resolution = based on collimator and distance from center; best at periphery; collimators need to by high sensitivity due to F18 being short lived, worsening spatial resolution; cameras aren't as close as in PET; best spatial resolution at periphery - PET spatial resolution = distance travelled from annihilation and intrinsic detector resolution (more important); relatively constant across detector; best at center (most attenuation); based on annihilation coincident detection; because so few make it, it has far better spatial resolution than SPECT PET vs SPECT re: attenuation - SPECT - less severe attenuation; less need for correction - PET - attenuation increases with distance from annihilation source; so few photons make it out, that's why spatial resolution is better; correct for by attenuation by adding transmission source in the detector |
|
|
|
How does scatter reduction differ in radiography versus PET
|
in PET you cannot use collimators because they discriminate scatter based on directionality; because origin is in the patient, directionality doesn't mean anything with regard to scatter
scatter is distinguished by its reduced energy (PHA) |
|
|
|
Crystal thickness in pet - thick versus thin
|
Thick - better conversion efficiency at the cost of spatial resolution
Thin - better spatial resolution at the cost of efficiency (less light spreading before it hits the PMT) Analogous to high versus low sensitivity collimators |
|
|
|
Detector material in PET vs SPECT
|
PET - cadmium tungstate
SPECT - bismuth germanate |
|
|
|
A radioactive source needs to have activity of 0.5 mCi at time of administration. If it arrives 5 days earlier, the activity will be ___ mCi. (Half life = 60 days)
|
A = Ao * e 0.69/(half life) * t
A = 0.5 * e 0.7/60 * 5 A = 0.53 Exponent becomes positive when going backwards in time. |
|
|
|
Convering versus pinhole collimator with regards to magnification and distance from collimators
|
Converging - mag increases as you move further away
Pinhole - magnification decreases until eventually you get minification |
|
|
|
Sinogram definition
|
Horizontal axis = data from different rays
Vertical axis = projection angle |
|
|
|
Equation for scintillation camera resolution relating intrinsic resolution to collimator resolution
|
Rsystem = (Rc^2 + Ri^2)^1/2
where Rc = Resolution of collimator and Ri = Resolution intrinsic to system |
|
|
|
collimators, compare high energy versus high sensitivity versus high spatial resolution
|
high sensitivity = wide holes; very efficient, sensitive, but poor spatial resolution
high energy = thick lead septa; low sensitivity/efficiency but can handle higher energy high spatial resolution = longer holes, less efficient, better spatial resolution |
|
|
|
equation to calculate what percent is reflected based on Z
|
[(Z2 - Z1)/(Z2 + Z1)]^2
Difference over the additive total squared |
|
|
|
What does extrapolation number (n) mean in cell survival curves
|
extrapolate linear portion of curve to its intersection with the y-axis; represents number of targets in a cell that must be hist to inactivate the cell OR hits required on a single critical achilles heel to inactivate the cell
|
|
|
|
focal spot size versus mAs and kvp
|
focal spot increases with increasing current (blooming); decreases slightly with increasing kvp
|
|
|
|
Pair production threshold energy
|
1.02 MeV (10x diagnostic x-rays which are 120 kVp at most)
|
|
|
|
Use factor vs workload
|
amount of time a beam is incident on a wall during the week (the wall being the primary barrier)
Workload is how often the machine is in operation (ma * min/week) |
|
|
|
Film has OD of 1 at exposure of 10 uGy and OD of 3 at 100 uGy, what is the gamma?
|
(OD2 - OD1) / (log Exposure2 - log Exposure1)
|
|
|
|
At what exposure do effects go from stochastic to deterministic
|
greater than 500 mGy is when they become more deterministic
|
|
|
|
Definition of pitch with helical CT
|
Pitch = table movement/collimator width
table movement is measured per 360 degree rotation |
|
|
|
If 1 second count interval has 10% uncertainty, what does 25 second count interval have?
|
To get new uncertainty, divide original uncertainty by square root of new count interval
Therefore, 10%/5 = 2% uncertainty |
|
|
|
What limits spatial resolution most in CR
|
Laser readout device
|
|
|
|
Units for cumulative activity
|
mCi*hr
|
|
|
|
equivalent dose definition
|
- absorbed dose * weighting factor
- weighting based on biologic damage - multiply by QF to get effective dose |
|
|
|
What type of detector is used in AEC
|
ionization chamber
|
|
|
|
PMT versus photodiode
|
PMT converts light into electrical signal (PM to e) and amplifies it
photodiode - light into electrical signal proportional to light intensity |
|
|
|
equation relating Larmour frequency and gyromagnetic ratio
|
Larmour = gyromagnetic ratio * magnetic field
ie.multiply magnetism x gyration ratio to get frequency of gyrations (Larmour) |
|
|
|
TE 20 TR 2000 vs
TE 80 TR 2000 |
TE 20 TR 2000 = proton density (minimize both)
TE 80 TR 2000 = T2 |
|
|
|
which sequence uses multiple RF pulses and phase encoding gradients
|
fast spin echo (multiple spins = multiple phases); amplify T2 and reduce T2*
|
|
|
|
which sequence uses multiple phase AND frequency encode gradients
|
EPI
|
|
|
|
AEC from 0 to -2 has what effect
|
Lower tolerance for exposure and earlier shut off meaning fewer total photons and therefore more noise
|
|
|
|
How long to stop breast feeding after 123I? Ga67? Thallium? MAA? Tech 99?
|
Ga67 = 4 weeks
Thallium = 3 weeks 123I = 1 week MAA = 12 hrs Tech = 24 hours |
|
|
|
Well counter vs dose calibrator - appearance generalizations
|
Generalizations:
Dose calibrators tend to be taller and have a wider hole at the top. The accompanying input device looks more like a calculator and the screen is smaller. Well counters are shorter, have a tinier hole and the accompanying device has a larger screen in order to display histograms. |
|
|
|
TR is usually short or long in FLAIR?
|
Long TR -- T2 emphasis.
|
|
|
|
Grid decentering makes film look
|
Too light (homogenous underexposure -- milky)
|
|
|
|
Harmonics which artifacts are removed and which resolution is improved
|
- reduced side lobe and reverberation artifacts
- increased lateral resolution |
|
|
|
If a photon with 1.687 MeV interacts with the nucleus, what is the maximum kinetic energy the positron can have?
|
Assuming this results in pair production, 1.022 MeV are used up to give rest mass of the electrons/positron pair. The excess energy is imparted as kinetic energy.
|
|
|
|
MR angiography sequence is based on?
|
Gradient echo phase contrast (ie. based on magnetic dipole of iron in blood)
|
|
|
|
doubling radiation dose decreases quantum mottle by how much
|
41%
|
|
|
|
At what angle will compton scatter photon have the highest energy? The lowest energy?
How about scattered electron? |
Highest energy = 0 degree angle (ie. it shoots straight on through)
Lowest energy = 180 degrees (complete backscatter) Vice versa applies to the electron (think billiard balls) |
|
|
|
Equation that Compton won the Nobel prize for relating incident photon energy and scattered photon energy
|
Compton of scattered photon = Compton incident photon energy - Scattered electron kinetic energy - Scattered electron binding energy
Es = Ei - Ek - Eb E scattered photon = E incident photon - Energy kinetic of scattered electron - Electron binding energy * electron binding energy is usually very small compared to compton photon energy and electron kinetic energy |
|
|
|
Which sequence cannot be obtained with gradient echo sequences?
|
T2 (cannot apply refocusing gradient to escape T2* effects)
|
|
|
|
Fan beam is used when in SPECT
|
Brain SPECT (FOV decreases with distance from collimator; essentially converging)
|
|
|
|
If you double SNR ratio how much o you increase dose?
|
4x
Jenn's equation: D = SNR^2/(pixel^3*T) |
|
|
|
Fission products
Cyclotron products Generator |
Fission - MIX - Moly, 131I, Xenon (all B-decay) - Hot MIX causes fission in your mouth
Gigi - Gallium(Thallium), Indium, Gobalt, 123I (All EC or B+ decay) & Flouro is also cyclotron produced 99Tech (IT - AGEx) - Old Tech |
|

