![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
96 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
1. What are the units for Dose area product?
A. Gy-cm2 B. Sv-cm2 C. mGy-cm-2 D. Gy-cm-2 |
A. Gy-cm2
Dose area product (DAP), also called Kerma area product (KAP)[1] is a quantity that reflects not only the dose but also the area of tissue irradiated. Therefore, it may be a better indicator of risk than dose. DAP is expressed in Sievert square centimetres (Gy*cm²)[1] (sometimes mGy*cm² or cGy*cm²). Coronary angiography and PCI produces expose patient to an average DAP in the range of 20 to 106 Gy*cm² and 44 to 143 Gy*cm² respectively.[2] |
|
|
|
2. Fluoroscopy is done on a 10 kg child. How do you decrease the dose?
A. Decrease focal spot size B. Remove the grid C. Increase the distance between the patient and the image intensifier. D. Increase the mAs |
Answer: B – removing the grid eliminates the Bucky factor. On multiple old tests.
|
|
|
|
3. What could be done to fix this artifact? aliasing on us
A. Larger transducer B. Decreasing the angle C. Increase the PRF. D. Increasing gate diameter. |
Answer: C – here are the ways you can decrease aliasing in Doppler U/S by increasing the maximum velocity:
Increase PRF (aka - decrease SPL) Increase angle Decrease transducer frequency Remember the equation: Vmax = (PRF * c)/(2fi * cosθ) C. Increase the PRF. |
|
|
|
4. The following CT image is from a child suspected of having appendicitis.
pitch: 0.75. kVp: 120 mA 340. |
A. Dose too high.
Answer: A – The mAs should be lower, and the pitch should be higher (>1). |
|
|
|
5. Regarding HIS and PACS, HL-7 is _____.
A. Something about transfer speed B. Something about security C. Image storage compatible with DICOM. |
Answer: B – HL-7 is a standards development organization that creates standards on how to represent and communicate data regarding health care.
|
|
|
|
6. What is the advantage of using two cameras vs one in nucs?
A. Better calculation of the linear attenuation coefficient B. Decreased acquisition time C. Improved spatial resolution D. Noise reduction |
Answer: B – on multiple old tests. Two cameras allow collection of counts twice as fast, so the imaging time can be decreased.
|
|
|
|
7. What is needed in PET for attenuation correction?
|
A. total LAC(linear attenuation coefficient) for a projection
Answer: A – this is a new question. Wish more options were recalled, but this is the correct answer. |
|
|
|
8. Object on the table is 4 inches and the image on the II screen is 7 inches. The distance between the table and the II is 12 inches. How far under the table is the tube?
A. 10 in B. 16 in C. 24 in D. 48 in |
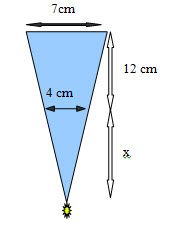
Answer: B – on multiple old tests. Here is how you do it: M = SID/SOD
Then solve for x: x/4 = (12 + x)/ 7 7x = 48 + 4x 3x = 48 x = 16 cm |
|
|
|
9. In MRI, chemical shift (i.e. in fat and water) is due to differences in:
A. T1 B. T2 C. Resonant frequency D. Atomic number |
Answer: C – on every single set of recalls ever made, so don't miss this one. The reason is that the fat and water process at different frequencies, so the artifact shows up in the frequency encode direction. NOTE: motion artifact is most pronounced in the phase encode gradient.
|
|
|
|
10. Molybdenum instead of Aluminum used as the filter for Molybdenum targets in mammography because?
A. The Molybdenum filter is relatively transparent to the characteristic X-rays of the Molybdenum target. B. Prevents scatter radiation from hitting the film C. Transmits high energy bremsstrahlung radiation with little attenuation D. Transmits low energy x-rays <10 kev with little attenuation E. Is usually 1 mm thick |
Answer: A – If you use the same material for the anode and the filter, the filter K-edge is always slightly higher than the characteristic xrays because the energy of the K characteristic x-ray is K-L. The characteristic xrays for Moly are 17.5 and 19.6 keV
|
|
|
|
11. For a given focal spot size and all other factors unchanged, what can be done to decrease the geometric unsharpness?
A. Increase the distance between the tube and the detector B. Decrease the distance between the patient and the detector C. Decrease the distance between the tube and the detector D. Increase distance between patient and dectector |
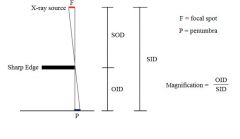
Answer: B – decreasing OID decreases magnification penumbra. See drawing below:
|
|
|
|
12. What is the total dose to a secretary from a source with a dose rate of 6mGy/hour at the secretary's desk and a half life of 10 minutes? The secretary and the source remain at the same distance for 2 hours.
A. 1.4 mGy B. 2.8 mGy A. 6 mGy C. 10 mGy D. 12 mGy |
Answer: A – Basically we need to find the accumulative dose (Ã) via the MIRD equation. The only tricky thing is to convert the half life to hours (10 min = 0.167hrs) b/c the dose rate is given in hours. Here is the MIRD equation:
à = 1.44 * f * Ao * Te à is the accumulative dose f is the fraction of activity per organ, which is 1 if you are calculating whole body dose (all the organs added together) Ao is the original dose rate Te is the effective half life (1.44 * Te is the average half life) à = 1.44 * 1 * 6mGy/hr * 0.1667 hr à = 1.44 mGy |
|
|
|
. Reducing workstation flicker can be accomplished by:
A. Data compression B. Lower bandwidth C. Contrast suppression D. Increasing the refresh rate E. Synchronization |
Answer: D – on multiple old tests.
|
|
|
|
14. Which of the following will have the best SNR?
A. T1 B. T2 C. Proton Density D. T2* |
Answer: C – T2* has the worst SNR.
|
|
|
|
15. What is the largest man made contributor to community radiation exposure?
A. Medical and dental x-rays. B. Nuclear fuel production. C. Them there big power lines running right over Searcy-Simmonds Medical Center. D. Weapons testing. E. Radioactive gold stolen from the famous Crighton, Alabama, Leprechaun. |
Answer: A – leprechaun gold isn't radioactive unless it's been licked by a unicorn.
|
|
|
|
16. What is the cause of lucent artifacts such as rings in mammography, paraspinal lines, and pseudo fractures of the odontoid?
A. Hanhaun filter B. Mach line |
Answer: B – according to an online medical dictionary, the Mach line is “the apparent line of contrasting density bordering a soft tissue shadow on a radiograph; is is an optical illusion constructed by the observer's retina.” I honestly never hear of it...
|
|
|
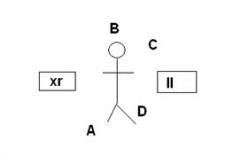
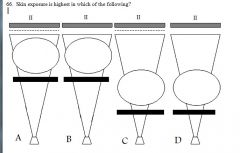
20. Standing at which site will give the radiologist the highest dose?
|
Answer: A – this is from a prior exam. 2006 test was the same except described in words not a picture.
|
|
|
|
21. In conventional linear tomography, a high density point (small round structure) located 2 cm below the imaging plane will appear on the image as:
A. a star B. a line C. an ellipse D. a point E. a rectangle |
Answer: B – ah, the token tomography question. If the answer to the question isn't 'fulcrum' or 'a line,' then I'm in trouble.
|
|
|
|
. In US of the liver, what is most important for creating the image?
A. Specular reflection. B. Non-specular reflection. C. Reverberation D. Electron density |
Answer:A specular reflection give each tissue it's characteristic ultrasound appearance. Specular reflections include the diaphragm, gallbladder wall, endometrial stripe, bladder distended with urine, etc.
|
|
|
|
23. What is the high dose fluoroscopy (1995 FDA rule) maximal exposure limit?
A. 100 mGy / min B. 200 mGy / min C. 40 mGy/ min D. 60 mGy/min |
Answer: B – Here are those limits:
Fluoroscopy unit under “normal usage” - 10R/min (100mGy/min) Fluoroscopy unit during “high-level control” (HLC) – 20R/min (200mGy/min) |
|
|
|
24. What is the maximal lifetime exposure limit for a 65 year old radiologist?
A. 3250 mSv B. 65 mSv C. 650 mSv D. 32500 mSv |
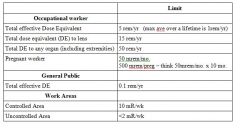
Answer: C – the limits for exposure include an average of no more than 1 rem (10 mSv) per year, with no individual year greater than 5 rem (50 mSv). Be sure you do the RSNA syllabus for radiation biology and/or check out the practice tests at this webpage: www.web-rad-train.org – username is trainee and password is enjoytheride
|
|
|
|
25. Which of the following groups do not have a special limit for radiation exposure?
A. Persons over the age of 65. B. Workers under the age of 18 C. The fetus of a pregnant worker D. General public E. Radiologist |
Answer: A – see the chart after #54.
|
|
|
|
26. Before obtaining counts for a thyroid uptake study, counts are first obtained over the patient’s thigh. Why is this?
A. Background B. To estimate non-thyroidal activity in the neck C. Decay Correction D. To assess for ectopic thryoid |
Answer: B – note, a background count is also obtained. However, you don't use the patient's thigh as the background (you use the room or the neck phantom without any pill inside).
|
|
|
|
27. Which organ’s parenchymal tissue is more sensitive than connective tissue?
A. Skin B. Liver C. Kidney D. Brain |
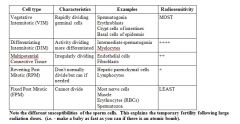
Answer: A – The stem describes a radiosensitive organ. The basal cells of the dermis are Vegetative Intermitotic (VIM), which is the most sensitive type of cells. Other radiosensitve organs include the testes, lymphoid organs, small bowel, ovaries, blood, and bone marrow. Here is a small chart of the cell types from most radiosensitive to the least.
|
|
|
|
28. Why do we used filtered back projection in CT instead of just back projection?
A. Reduce beam hardening B. Reduce effects of partial volume averaging C. Reduce blurry images. D. Less radiation dose |
Answer: C – filtering removes the 1/r blurring
|
|
|
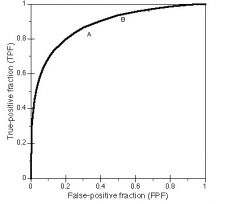
30. What happens when a radiologist moves from A to B ?
A. Increased false positives B. Increased sensitivity C. Increased specificity D. Increased positive predictive value E. Become a useless overcaller guy |

Answer: A (& B) – Sensitivity will also be increased (TPF is sensitivity).
|
|
|
|
31. Fourier analysis ratio of output to input modulation (signal amplitude) of an imaging system at each spatial frequency is known as:
A. Modulation transfer function B. Contrast Detail analysis C. Region of interest curve D. Graft versus host disease E. Herpes |
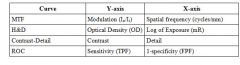
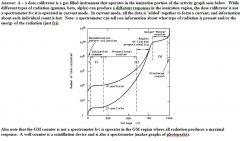
Answer: A – This is just a fancy way of saying the y-axis is modulation and the x-axis is spatial frequency. Decoding what the questions are asking is half the battle. Just as a side note, here are the x and y axis of multiple graphs that may show up on the test:
|
|
|
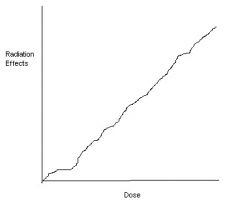
32. What is represented in the following graph?
A. Small sensitive population within a larger population B. Linear non-threshold C. Small resistant population within a larger population D. Large sensitive population |
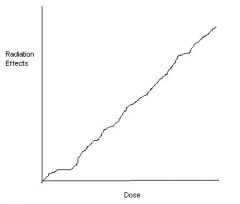
Answer: B – linear non-threshold is classic for stochastic effects.
|
|
|
|
33. Decreasing the magnification from 12 inches to 4 inches will result in what change in II image characteristics?
A. Decreased spatial resolution. B. Decreased image lag C. Increased contrast D. Increased conversion factor. |
Answer: A – decreasing mag increases the FOV on the input phosphor, which worsens the spatial resolution (more area mapping to the output phosphor, which doesn't change in size). Increasing the FOV also worsens pincushion and vignetting artifact.
|
|
|
|
34. Two brass wires are placed 5 cm apart on a fluoroscopy table. The screen is 36 cm above the table. The brass wires are 9 cm apart on the screen. How far under the table is the x-ray source?
A. 9cm B. 28cm C. 36cm D. 45cm E. 81cm |
Answer: D – see the explanation for #8 (essentially the same question).
|
|
|
|
35. When is XR tube housing leakage most important?
A. CT B. Fluoroscopy C. Dedicated CXR machine D. PET/CT |
Answer: B – do you remember the limit for leakage radiation from a flouro machine??? It is 100mR/min at maximum kVp and maximum continuous mA at a distance 1 meter from the tube.
|
|
|
|
36. In diagnostic imaging, damage to biologic tissue is most likely the result of:
A. Scattered x-rays B. Characteristic x-rays C. Photoelectrons and Compton recoil electrons D. Neutrons |
Answer: C – on multiple old tests.
|
|
|
|
|
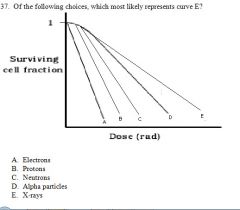
Answer: E – curve E is low-LET radiation. Both electrons and x-rays are low LET radiation, but X-rays are lower LET than electrons b/c they have no mass or charge.
|
|
|
|
Answer: E – curve E is low-LET radiation. Both electrons and x-rays are low LET radiation, but X-rays are lower LET than electrons b/c they have no mass or charge.
|
|
|

|
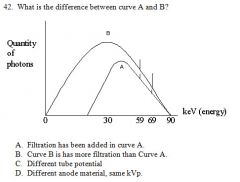
Answer: D – know this stuff b/c it should be easy points. It is on every recall.
PPV = TP/TP+FP NPV = TN/TN+FN Sensitivity = TP/TP+FN Specificity = TN/TN+FP Remember that sensitivity and specificity do not depend on disease prevalence but positive and negative predictive values do. |
|
|
|
Answer: A – the same max keV means the kVp is constant (C is false). The same characteristic xray spikes means the same anode material was used (D is false). The more filtration will preferentially removes the lower end of the spectrum.
|
|
|
|
43. What is the result if an abdominal image (plain film) is obtained using digital technique and “twice the normal radiation”?
A. Too light B. Too dark C. Decreases noise D. Decreasing latitude |
Answer: C – more photons are used, which lowers quantum mottle (noise). There is some controversy among the residents as far as what happens to latitude, contrast, and grayscale. See the discussion and graph on #122 of the 2004 version of the recalls...
|
|
|
|
44. What process dominates in Tc99 photons?
A. Photoelectric effect B. Pair production C. Compton D. Photodisintegration E. Auger electron |
Answer: C – Tc-99m energy is 140 keV. Over 26 keV favors Compton effect.
|
|
|
|
45. What can directly measure exposure?
A. NaI well counter B. TLD badge C. Ionization chamber D. Dose calibrator |
Answer: C – exposure is defined as charge per unit air. The ionization chamber is an air filled instrument ideal for measuring exposure. Whenever you see the word exposure in a question, think ionization chamber.
|
|
|
|
46. Calculations based on detection in the radiation badge (film or TLD) is reported as:
A. Effective dose B. Equivalent dose C. Air Kerma D. Absorbed dose |
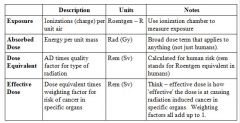
Answer: B – Dose equivalent takes into effect weighting factors based on the different types of radiation. The film badges have different thickness filters to discern high LET from low LET radiation. The dose reports from the badges are in mrem. Plus, there is a recall question about a “pregnant intervetionalist” that gives her dose from a film badge in mSv. Effective dose is also reported in rem (Sv); however, it is a risk assessment of different organs getting cancer via the weighting factor. The total of all the weighting factors is equal to 1. Here is a chart to keep the units straight:
|
|
|
|
47. The mammography tech changes the AEC setting from 0 to –1. What is the result?
A. Decreased optical density on the film. B. Increased optical density of the film C. No change in the optical density of the film. D. More radiation dose. |
Answer: A – decreasing the AEC will decrease radiation dose, so the exposure will have a lower OD via the H&D curve. Note: B and D go together and can be eliminated as the answer b/c they both can't be right.
|
|
|
|
47. The mammography tech changes the AEC setting from 0 to –1. What is the result?
A. Decreased optical density on the film. B. Increased optical density of the film C. No change in the optical density of the film. D. More radiation dose. |
Answer: A – decreasing the AEC will decrease radiation dose, so the exposure will have a lower OD via the H&D curve. Note: B and D go together and can be eliminated as the answer b/c they both can't be right.
|
|
|
|
48. How do you increase the sensitivity of a well counter?
A. Increase the time for measurement. B. Decreasing the PMT voltage C. Some other options... |
Answer: Not given – remember that with a scintillation device (such as a gamma camera or a well counter) sensitivity is the number of counts measured per number of decays occurring in the sample. Increasing time increases counts, but degradations increase at the same rate. So increasing time does not increase the sensitivity. The correct answer is not present. One way to increase the sensitivity would be to increase the depth of the well to increase geometric efficiency. Another would be anything that increases the absorption or conversion efficiencies, such as decreasing the dead time b/t counts...
Sample Volume and Dead-Time Effects in Sodium Iodide Well Counters The position of a sample in a sodium iodide well counter has a dramatic effect on the detection efficiency. ‘When liquid samples in vials of a particular shape and size are counted, the detection efficiency falls as the volume increases. Most nuclear medicine in vitro tests require the comparison of a liquid sample from the patient with a reference s-ample. It is crucial that both samples be in identical containers and have identical volumes. In addition, the high efficiency of the Nal well counter can cause unacceptable dead-time count losses, even with sample activities itt the microcurie range. In is important to ensure that the activity placed in the well counter is sufficiently small that dead-time effects do not cause a falsely low count. In general, well counters should nor be used at apparent count rates exceeding about 5,000 cps, which lim irs samples of 1-125 and Co-57 no activities less than about 0.2 RCi. However, larger activities of sonic radionuclides may be counted without significant losses; for example, activities ofCr-Si as large as 5 j.tCi may be counted, because only about one out of every ten decays yields a gamma ray. |
|
|
|
49. What is dose calibrator?
A. Ionization chamber B. Proportional chamber C. Scintillation crystal D. Semiconductor diode |
|
|
|
|
50. The purpose of pulse height analyzer is to:
A. increase the sensitivity of the camera B. compensate for photon absorption C. reduce the effect of scatter D. increase photon detection |
Answer: C – scatter radiation should have less energy b/c of energy lost to Compton electrons.
|
|
|
|
51. There is an area of intense activity within the FOV but not the field of interest. What can be done to decrease pulse pile up?
A. Place a lead shield over this area B. Narrow your energy window |
Answer: ?? Seems like placing lead over this area may work depending on the type of radioisotope. Narrowing your window will reduce pulse pile-up. Unsure of the answer.
|
|
|
|
52. Regarding Radon 222:
A. Higher concentration in basements than outdoors. B. Comes from the breakdown of polonium C. Is an insignificant source of radiation D. Increases the risk of bone cancer |
Answer: A – read the RSNA syllabus on radiation biology as it contains information about radon. Available at rsna.org under the residents section.
The short-lived decay products of radon 222 Rn-222 are the most significant source of exposure from the inhalation of naturally occurring radionuclides. Radon- 222, a noble gas, is produced in the U-238 decay chain by the decay of radium-226 Ra-226. Rn-222 decays by alpha emission, with a half-life of 3.8 days, no polo nium 218 Po-2 18, followed by several other alpha and beta decays, eventually leading to stable lead-206 Pb-206. Once the short-lived daughters of radon are inhaled, the majority of the dose is deposited in the tracheobronchial region of the lung. Radon concentrations in the environment vary widely. There are both sea sonal and diurnal variations in radon concentrations. Radon gas emanates primar ily from the soil in proportion no the quantity of natural uranium deposits; its dis persion is restricted by structures producing significantly higher levels than found outdoors in the same area. Weatherproofing of homes and offices and other energy conservation techniques typically decrease outside air ventilation, resulting in higher indoor radon concentrations. |
|
|
|
53. Dose limit for nonworker
|
1 mSv / year
|
|
|
|
54. Dose limit to fetus?
|

0.5 mSv /month
Radioactivity is measured in Becquerel (Bq) per second. 1 Bq means one disintegration per second. It is also measured in Curie (Ci), named for Madam Curie, who shared Nobel Prize with her husband. 1 Curie = 3.7 x 1010 Bq or disintegrations per second. The radiation absorbed dose is measured in Gray, rad, rem and Sievert (Sv). In the United States, absorbed dose is commonly given in rad or Gray and other protection quantities, such as equivalent dose and effective dose, are given in rem. The following table is provided to help avoid confusion among persons not familiar with these quantities. The use of the newer system of units would be particularly useful during radiological incidents involving international responders. Conversions for Effective Dose, Equivalent Dose, Dose Equivalent, and ambient dose equivalent 0.001 rem = 1 mrem = 0.01 mSv 0.01 rem = 10 mrem = 0.1 mSv 0.1 rem = 100 mrem = 1 mSv = 0.001 Sv 1 rem = 1000 mrem = 10 mSv = 0.01 Sv 10 rem = 100 mSv = 0.1 Sv 100 rem = 1000 mSv = 1 Sv (Sievert) 1000 rem = 10 Sv Conversions for Absorbed Dose 0.001 rad = 1 mrad = 0.01 mGy 0.01 rad = 10 mrad = 0.1 mGy 0.1 rad = 100 mrad = 1 mGy = 0.001 Gy 1 rad = 1000 mrad = 10 mGy = 0.01 Gy 10 rad = 100 mGy = 0.1 Gy 100 rad = 1000 mGy = 1 Gy (Gray) 1000 rad = 10 Gy Measured Dose (Temporary Measurements) – gamma radiation or X-rays 1 R (roentgen) = 0.01 Gy = 0.01 Sv |
Radioactivity is measured in Becquerel (Bq) per second. 1 Bq means one disintegration per second. It is also measured in Curie (Ci), named for Madam Curie, who shared Nobel Prize with her husband. 1 Curie = 3.7 x 1010 Bq or disintegrations per second. The radiation absorbed dose is measured in Gray, rad, rem and Sievert (Sv).
In the United States, absorbed dose is commonly given in rad or Gray and other protection quantities, such as equivalent dose and effective dose, are given in rem. The following table is provided to help avoid confusion among persons not familiar with these quantities. The use of the newer system of units would be particularly useful during radiological incidents involving international responders. Conversions for Effective Dose, Equivalent Dose, Dose Equivalent, and ambient dose equivalent 0.001 rem = 1 mrem = 0.01 mSv 0.01 rem = 10 mrem = 0.1 mSv 0.1 rem = 100 mrem = 1 mSv = 0.001 Sv 1 rem = 1000 mrem = 10 mSv = 0.01 Sv 10 rem = 100 mSv = 0.1 Sv 100 rem = 1000 mSv = 1 Sv (Sievert) 1000 rem = 10 Sv Conversions for Absorbed Dose 0.001 rad = 1 mrad = 0.01 mGy 0.01 rad = 10 mrad = 0.1 mGy 0.1 rad = 100 mrad = 1 mGy = 0.001 Gy 1 rad = 1000 mrad = 10 mGy = 0.01 Gy 10 rad = 100 mGy = 0.1 Gy 100 rad = 1000 mGy = 1 Gy (Gray) 1000 rad = 10 Gy Measured Dose (Temporary Measurements) – gamma radiation or X-rays 1 R (roentgen) = 0.01 Gy = 0.01 Sv |
|
|
55. Sensitivity of a collimator is improved by?
A. Moving the source closer to the collimator B. Thicker septa C. Increasing hole size D. Longer septa E. Widened photopeak |
Answer: C – widening the photopeak will increase sensitivity of the system, but doesn't involve the collimator. Moving a source closer to the collimator does not improve sensitivity, which is a little counterintuitive. Bigger holes let more counts through, but a high sensitivity collimator has poorer spatial resolution.
-Collimator sensitivity is the fraction of gamma rays reaching it from all directions that pass through the holes. -Collimator sensitivity is low, with approximately 10-A (or only 0.01%) of the emit- ted photons being detected. -Collimators generally involve a tradeoff between spatial resolution and sensitivity. -Resolution is increased if the size of the holes is reduced (thicker septa) or if the collimator is made thicker. -These same changes decrease the number of photons reaching the crystal, thus re- ducing system sensitivity. -Parallel-hole collimators are classified for high-sensitivity (i.e., low-resolution), general-purpose, and high-resolution (i.e., low-sensitivity) uses. -High-sensitivity collimators are thinner and have larger and, therefore, fewer holes and lower resolution. -High-resolution collimators have smaller and, therefore, more holes and lower sen- sitivity; these can transmit half as many photons as the general-purpose collimator. -Low-energy collimators, for use with 99 mTe and 20 'TI, have thin septa. -Medium-energy collimators, used with 67 Ga, "'I, and 111 In, have thicker septa and, therefore, fewer holes and lower sensitivity. -High-energy collimators are used for 131 I and 15 F, and have even thicker septa. |
|
|
|
56. Subtle ring artifact in a nuclear medicine study
A. Something wrong with the detector (dent?) B. Energy was wrong C. Linearity misaligned D. PMT defect |
Answer: probably A – Ring artifact in SPECT is due to Flood field inhomogeneity. A defective PMT will give a circular defect in an planar image. Photopeak off center will make all PMT dark or light depending on the direction of the error.
|
|
|
|
57. Lateral decentering in a focused grid causes ________ .
A. One side of the film to be darker than the other. B. Uniform cutoff C. Brighter in the center than the edges D. Cutoff on one side of the image |
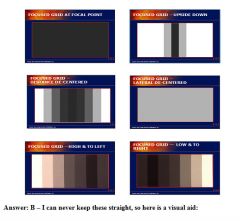
|
|
|
|
. Which option would be best to improve the resolution in planar imaging of the heart?
A. Move the collimator from 5 inches to 1 inch away from the patient. B. Remove the collimator C. Move the collimator from 1 inch to 5 inches away from the patient D. Smaller kernal in filtered backprojection |
Answer: A – collimator resolution is best at the surface. The crystal resolution is independent of distance. Image cannot be obtained without the collimator, which creates the projection on the surface of the crystal. Filtered backprojection is not used in planar imaging.
|
|
|
|
60. What is a pacemaker a contraindication for MRI? All of the following can occur except:
A. wires detach B. current in wires can burn the patient C. changes from synchronous to asynchronous D. may damage the pacemaker |
Answer: A. Asynchronous mode for pacemaker can be used for getting MRI done on a patient with pacemaker.
|
|
|
|
61. What is the advantage of the following :
TR 2000 TE1 20 TE2 80 A. T2 and PD images acquired at the same time B. T1 and PD images acquired at the same time C. T1 and T2 images acquired at the same time D. PD images acquired with fat saturation |
Answer: A – Long TR should remove T1 as an option. PD uses a short TE to minimize T2 signal. T2 needs a long TE. Fat saturation is an entirely different process (inversion).
|
|
|
|
62. Which sequence is the fastest?
A. IR B. EPI C. FSE D. T1 |
Answer: B – just think about those fuzzy T2 weighted images that the techs get on patients who keep moving. They are labeled EPI (echo planar imaging).
-Echo planar imaging (EPI) uses rapidly switching gradients to refocus echoes. -Frequency-encode gradients that rapidly change polarities are paired with an ap- plied phase-encode gradient. -EPI can generate MR images in 50 milliseconds but with limited resolution (64 2 or 1282 matrix). -Special high gradients between 20 and 60 mT/m (2 and 6 G/cm) are required to per- form EPI. |
|
|
|
64. How many images to fill a 40 Megabyte hard drive with a 512x512 matrix and 16 bits?
A. 80 B. 120 C. 50 D. 10 |
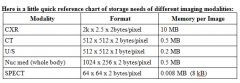
Answer: A – here is the math:
512 x 512 x 16 bits x 1byte/8bits = 524,528 = ~0.5MB/image 40MB/(0.5MB/image) = ~80 images |
|
|
|
65. Decreasing the FOV in MRI causes ________ .
A. decreased SNR B. decreased resolution C. longer imaging times D. angry leprechaun |
Answer: A – decreasing area means less signal, which lower SNR
|
|
|
|
Answer: C – the small SOD, large OID, and the grid all increase the patient dose. B would have the lowest dose for the opposite reasons.
|
|
|
|
67. 25 cm with 512 matrix size, what is the resolution?
A. 0.75 lp/mm B. 1 lp/mm C. 2 lp/mm D. 5 lp/mm E. 7 lp/mm |
Answer: B – 512 pixels create 216 lp. 216 lp/250 mm = 1.02 lp/mm. OR size of pixel is 250mm / 512 pixels = 0.488mm. Put into equation 1/2(pixes size) = 1.02 lp/mm
|
|
|
|
68. Something about HL7, HIS, RIS
A. Security B. Hospital and DICOM communicate |
Answer: B
Health Level Seven (HL7), is an all-volunteer, non-profit organization involved in development of international healthcare standards.[1] "HL7" is also used to refer to some of the specific standards created by the organization (e.g., HL7 v2.x, v3.0, HL7 RIM).[citation needed] HL7 and its members provide a framework (and related standards) for the exchange, integration, sharing, and retrieval of electronic health information. v2.x of the standards, which support clinical practice and the management, delivery, and evaluation of health services, are the most commonly used in the world |
|
|
|
69. What is the efficiency of the detector?
3700 Bq count rate 37000 in one minute A. 0.17 B. 0.10 C. 0.60 D. 0.26 |
Answer: A – Here is the math:
3700 Bq = 3700 degradations per second x 60sec/min = 222,000 deg/min 37000cpm/(222,000 deg/min) = 0.167 counts/deg |
|
|
|
70. For a CXR, which is not needed in a digital system?
A. Edge enhancement B. Recursive filtration C. Histogram equalization D. Look up table |
Answer: B – Used in fluoroscopy.
- Recursive filtering: used in fluro/angio Different averaging algorithms can be used, but a common approach to frame averaging is called recursivefiltering. In this approach, the image just acquired, I,,, is added with the last image L1-z using - edge enhancement enhancement of structure margins (edges) using digital processing tech-niques. Unsharp masking is a method of edge enhancement that involves subtraction of a smoothed version from the original which is then added to a replicate original. Fine details are enhances at the expense of increased noise and artifacts. - Histogram equalization eliminates white and black pixels that contribute little diagnostic information and expands the remaining data to use the full dynamic range. - Look up tables are a method of altering the tonal qualities of an image by mapping intensity values to a desired brightness level. This is similar to an H and D curve, which maps xray intensity values to film optical density. |
|
|
|
71. How do you decrease shadow artifact in CT. Something about an abrupt cutoff in the Z-direction.
A. decrease pitch B. bow tie filter C. something about algorithm |
Answer: ??
I presume this is aimed at reducing beam hardening artifact which is performed in a retrospective manner with synthesized projection samples cutting off the hardened projections. bowtie filter a filter shaped like a bowtie that may be used in computed tomography to compensate for the shape of the patient's head or body. It is used with fan-shaped x-ray beams to equalize the amount of radiation reaching the film. |
|
|
|
72. What is the best way to decrease Noise in CT?
A. Reduce kVp B. Reduce mA C. Reduce Scan tine D. Reduce patient size |
Answer: D – noise is due to decreased # of photons detected. Decreasing patient size will lower attenuation, and more photons will reach the detector.
|
|
|
|
73. How is screen-film contact measured in mammography QC ?
A. Wire mesh B. Phantom OD C. Microscope D. Densitometer |
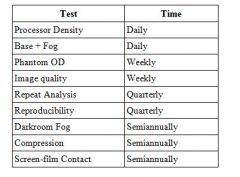
Answer: A – see the chart for timeline of mammography quality control:
|
|
|
|
74. How does a sonographer adjust the foci?
A. Electronically altering the transducer elements by changing the amplitude B. Physically rocking the transducer elements C. Mechanically rocking the transducer elements D. Electronically altering the transducer elements by introducing delays E. Rotating the transducer elements within the transducer |
Answer: D – on multiple old tests.
|
|
|
|
75. The probability of decay of a radioactive isotope per unit time is ?
A. logarithmic B. constant C. semi-logrithmic D. linear |
Answer: B – this is the definition of the decay constant (λ).
decay constant (A) the rate of decay of radionuclides (X = 0.693/T 1/2, where T1/2 is the half- life) |
|
|
|
76. What does an eV represent?
A. Energy B. Potential C. Charge D. Velocity |
Answer: A – kVp represents potential. Another question asks what is that mAs? The number of photons.
|
|
|
|
Which of the following is a benefit of US harmonics?
|
- Reducing near field artifacts.
- Also best used for better depth resolution - another recall relates to this. |
|
|
|
78. Where does Molybdenum come from?
A. Reactor B. Cyclotron C. Generator D. Cox Pharmaceuticals |
Answer: A – you just have to know that Mo degrades by Beta (-) emission, which means it has a neutron excess (needs more protons, so it loses a negative charge, which is the same as gaining a positive charge). Neutron rich radiopharmaceuticals are made in a reactor where neutrons from the fuel rods are jammed into the target molecules.
|
|
|
|
79. Increasing II aperture causes?
A. Decreased dose B. Less noise C. Increased dose D. the f number to increase |
Answer: A – the other options are backwards.
|
|
|
|
80. Images from two perfusion scans:
A B A. B has fewer counts then A. B. B has less noise than A C. Artifacts in B are from motion D. Some other wrong answer |

Answer: A
|
|
|
|
81. Max keV is determined by?
A. kVp B. mA C. filament current D. tube current |
Answer: A – Max keV is always kVp. B and D are the same thing.
|
|
|
|
82. If a large obese patient develops a rash that is 7 x 10 cm in size on the right mid back 2 weeks after undergoing 5 hours of cardiac fluoroscopy that had a window size of 16 x 16 cm what is the cause of his rash?
A. Improper defibrillator pad placement B. Radiation induced injury C. Allergy to the adhesive in the defibrillation pad D. Electric burn from broken defibrillator wire E. Pannusitis |
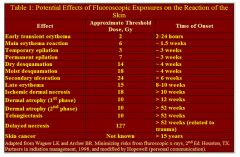
Answer: B – on multiple old tests. Oh no, I haven't put that chart of skin reaction to radiation on this set of recalls yet. Well, here it is:
|
|
|
|
DSA quantum noise is increased by?
|
Answer: A – also know that QM is 1.4 times higher in the subtracted image than the mask.
|
|
|
|
Decreased FOV in MRI causes?
|
Deceased SNR
|
|
|
|
85. What is the kVp for cardiac angio?
A. 50 B. 70 C. 90 D. 110 E. 150 |
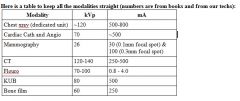
Answer: B – I walked down to the cath lab and asked one of the cardiologists. His response was “what is kVp?” So I asked one of the techs. They said in general the kVp is 70. What about the mA??? ~470
|
|
|
|
86. If, over a 4 minutes period, the total counts is 6000 and the background counts are 4000, what is the Sample rate its standard deviation?
A. 500 +/-11 B. 44 +/- 25 C. 2000 +/- 25 D. 2000 +/- 44 |
Answer: A – the sample rate is the number of counts in the sample (6000 - 4000 = 2000) divided by the counting period (2000/4 = 500 cpm). The error rate is the square root of the sample counts divide by the counting period (√2000/4 = 11.2). NOTE: you cannot just take the square root of the count rate to get its standard deviation.
|
|
|
|
87. Artifact in a MRI phantom with alternating black and white parallel lines
A. Aliasing B. Motion C. Gibbs D. Phase encode something |
Answer: C – Gibbs artifact is due to algorithm problems (not enough PEG steps). To fix Gibbs, increase the matrix from 256x128 to 256x256.
|
|
|
|
88. Compression is used in mammography for all of the following except?
A. Decreased quantum mottle. B. Create uniform film optical density C. Decrease dose to the breast D. Increase the amount of tissue imaged at the chest wall E. Increase contrast |
Answer: A – compression causes decrease in dose and increased quantum mottle. Note: A and C are opposite, so one of them has to be the right answer.
|
|
|
|
89. In CT Fluoroscopy, how can you improve temporal resolution?
A. Increase the pitch B. Increase the mA C. Change your acquisition range from 360 to 180 degrees. |
Answer: C, I think – I changed this answer from B to C b/c B makes no sense. Increasing temporal resolution can be achieved by decreasing pitch, adding a second x-ray source, increasing rotation speed, and gating.
|
|
|
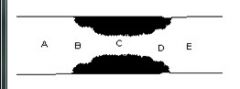
. Where is the laminar flow?
|
Answer: A – laminar flow is normal, streamline flow (before the stenosis). At the stenosis there will be turbulent flow, and distal to the stenosis, there will be slow, post stenotic flow.
|
|
|
|
100. What is the most common cause of quality control problems in screen-film mammography?
A. Processor B. Phantom C. Screen film contact D. Compression device |
Answer: A – a clue is that you check the processor daily, so it must have more problems.
|
|
|
|
101. What is used to measure the OD in screen-film mammography?
A. Sensitometer strip B. Densitometer C. The radiologist opinion D. Your momma |
Answer: B – A sensitometer exposes the film to make a sensitometry strip, which is then read by a densitometer to tells the OD.
Phantom OD is checked weekly |
|
|
|
102. If the center of rotation of a SPECT machine is not well-aligned with the center of the projection image, the resulting clinical image will demonstrate:
A. cupping B. degraded spatial resolution C. enhanced star artifact D. bright spot in center E. some other artifact |
Answer: B – although it is often described as a 'doughnut' artifact with a circle of activity instead of a dot, in real life, the result of a improper center of rotation is simply a “smudging” of the image (loss of spatial resolution). The SPECT image doesn't have the spatial resolution to see the 'doughnut.' Remember that cupping artifact (A) is just another word for streak artifact. Star artifact (C) is a result of back projection.
|
|
|
|
103. What determines the slice thickness in multidetector CT?
A. Collimator B. Detector Pitch C. Detector width D. Pitch |
Answer: C – slice thickness depends on detector size in multidectector systems and on beam collimation in single detector systems.
|
|
|
|
104. Childhood leukemia resulting from intrauterine exposure is best described as a ________ effect.
A. Somatic stochastic B. Stochastic genetic C. Deterministic genetic D. Deterministic somatic |
Answer: A – I changed this answer from B b/c I think A makes more sense.
SOMATIC STOCHASTIC EFFECTS: SOMATIC STOCHASTIC EFFECTS: CANCER CANCER Cancer development is the main somatic stochastic effect induced by ionising radiation. Cancer development is an extremely complex process involving many changes, which nature will depend on: • • The cell involved. • • The mechanism of the carcinogen inducing cancer. • • The cancer type that is developed. Several generic models to describe cancer process have been developed: Multistage model. HEREDITARY STOCHASTIC EFFECTS HEREDITARY STOCHASTIC EFFECTS Occur in the progeny of the irradiated person. They have NOT been demonstrated in humans. Data in experimental animals and plants are available. To estimate hereditary effects risk, the ”Doubling Dose” (DD) method is used. DD: Dose needed to produce as many mutations as those occurring spontaneously in one generation. |
|
|
|
105. What measurement used for CT dose best estimates risk?
A. Effective dose B. CTDI C. Dose length product |
Answer: A – The DLP is calculated from the CTDI via the relationship:
CTDIweighted = 1/3 CTDIcenter + 2/3 CTDIperiphery The effective dose is calculated from the DLP via the relationship: Effective Dose (mSv) = DLP x 0.19 So, I think the answer is effective dose. Another clue to this question is the word RISK, which is best defined by the effective dose. |
|
|
|
106. The physical half life of a radionuclide is 6 hours and the biological half life is 3 hours. What is the effective half life?
A. 0.5 hours B. 2 hours C. 3 hours D. 6 hours E. 9 hours |
Answer: B – Here is how you do it:
Teff = (Tb x Tp)/(Tb + Tp) Teff = (6 x 3) /(6 + 3) = 18/9 Teff = 2 hrs |
|
|
|
107. MI and TI displayed during the acquisition of ultrasound images describe:
A. Impedance and specular reflection B. Motion and temporal resolving time C. Receiver and transmitter gain D. Frequency and depth of focus E. Cavitation and heat |
Answer: E
|
|
|
|
108. Something about the K-edge of barium and iodine.
|
Iodine - 33.2 keV and Barium - 37.4 keV
There is a later recall that asks about the KVP for angio and you have to know the k edge of idodine. Ideal mean is 1/2 to 1/3 max kvp - so roughly 70-80 kvp |
|
|

109. The following artifact is caused by what occurring proximal to the artifact?
A. high attenuating material B. low attenuating material C. two close interfaces D. side beam interference |
Answer: C – Ring down has the same cause as reverberation. Also called specular reflection. specular reflection ultrasound reflections from large smooth surfaces
|
|
|
|
110. What will be the effect of using a high pass RAMP filter instead of a low pass RAMP filter?
A. Worsened spatial resolution B. More smoothing C. Increased noise D. Decreased patient dose E. Increased sensitivity for low contrast tumors |
Answer: C – I totally just made this question up... the original recall only said, “Something about a RAMP filter.” Basically, just know that the high pass RAMP filter includes high spatial frequencies (small objects). This creates better spatial resolution (bone algorithm) but also includes all those “little dots” that make the bone windows look grainy. In other words, the noise goes up. Low pass filters increase smoothing, decrease noise, and increase sensitivity for low contrast tumors (think liver window).
|
|
|
|
112. Something about Tc99m MDP
|
Don't know - here is some shit on it anyway.
Methylenediphosphonane MDP localization occurs primarily by adsorption in the mineral phase of the bone. MDP concentrations are significantly higher in amor phous calcium than in mature hydroxyapatite crystalline structures, which helps to explain its concentration in areas of increased osteogenic activity. Here is some more crap I didn’t know about mdp and effective half life Ideally, a radiopharmaceutical's effective half¬life equals approximately 1.5 times the duration of the diagnostic procedure. This provides a good compromise between our desire to minimize radiation dose to the patient and to maximize the dose to be injected so counting statistics are good and image quality is optimal. With the sole exception of Xe¬133 or another noble gas used for a ventilation study, there is no other procedure in which images are acquired and the radiopharmaceutical is expelled from the body almost quantitatively within a few minutes of completing the study. Most compounds exhibit exponential clearance patterns so their effective half-life is moderately long (measured in hours or days as opposed to seconds or minutes). The relationship between effective half-life, biological half-life, and physical half-life is shown in the equation below: 1 / t(eff) = 1 / t(biol) + 1 / t(phys ) In the special case where the biological half-life of a particular compound is very long compared to the physical half-life (e.g., Tc¬99m sulfur colloid in the liver), 1 / t(biol) is a very small number, approximating 0, and the effective half-life therefore equals the physical half-life. Similarly, where the physical half-life is very long compared to the biological half-life (e.g., Xe¬133 gas in the lungs), 1 / t(phys) is a very small number, approximating 0, and the effective half-life equals the biological half-life. The classical example of an ideal effective half-life is that of Tc¬99m MDP, which has an effective half-life = 6 hr; since bone imaging is a 4 hr procedure, the ratio of effective half-life to duration of the test is 1.5:1, considered ideal. On the other hand, Tc¬99m sulfur colloid has a effective half-life of 6 hr in the liver, but the procedure takes only 1 hr. This 6:1 ratio doesn't mean that a liver scan is a bad procedure to perform, but rather that the compound has a residence time in the liver that is longer than desirable, resulting in an increase in the radiation dose to the target organ. In this particular case, simply switching from Tc¬99m sulfur colloid to Tc¬99m microaggregated albumin decreases the teff from 6 hr to approximately 3 hr, lowering the ratio of effective half-life to procedure length to 3:1 and decreasing the radiation dose by 50%. adsorption in the mineral phase of the bone. MDP concentrations are significantly higher in amor phous calcium than in mature hydroxyapatite crystalline structures, which helps to explain its concentration in areas of increased osteogenic activity. |
|
|
|
113. A new positron emitting radiopharmaceutical is developed for PET imaging. The energy of the positron emitted is 100 keV. What is the approximate energy of the photon absorbed at the surface of the detector?
A. 80 keV B. 100 keV C. 140 keV D. 512 keV E. 1.02 MeV |
Answer: D - This is PET so you get two 511 keV photons regardless of the other info. The detected photons are due to the annihilation reaction of the positron and an electron.
|
|

