![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
81 Cards in this Set
- Front
- Back
|
Thrill
|
A palpable murmur, usually due to vibrations that accompany loud murmurs
|
|
|
Lift (Heave)
|
When the cardiac impulse feels more vigorous than normal, and can be felt through the chest wall
|
|
|
Claudication
|
Achy leg pain when walking
|
|
|
Orthopnea
|
SOB when lying down
|
|
|
Paroxysmal Nocturnal Dyspnea (PND)
|
Sudden waking in the middle of the night with SOB
|
|
|
Palpation for Apical Impulse
|

Rt Hand on patients chest as shown
|
|
|
PMI
|
point of maximal impulse
|
|
|
Locations for Cardiac Palpation
|
Apical Impulse
PMI Left Sternal Border and Base |
|
|
Locations for Cardiac Auscultation
|
Aortic – 2nd ICS, RSB
Pulmonic – 2nd ICS, LSB Second Pulmonic – 3rd ICS, LSB Tricuspid – 4th & 5th ICS, LSB Mitral (apex) – 5th ICS, MCL |
|
|
Locations for Axillary Lymph Node Palpation
|
Anterior axillary line
Midaxillary line Posterior axillary line Medial upper arm |
|

Identify
|
Bisferiens Pulse
|
|
Identify
|
Pulsus Alternans
|
|
Identify
|
Bigeminal Pulse
|
|
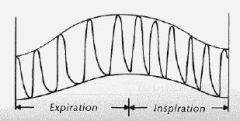
Identify
|
Paradoxical Pulse
|
|
|
Specialized Exam: Measurement of JVD
|
Elevate the head of the bed to 30 degrees.
Find internal jugular venous pulsations. Locate the highest point of pulsation. Measure from the sternal angle (sternal angle is considered to be 5cm above the right atrium). JVP higher than 4 cm above the sternal angle (9 cm above R atrium) indicates elevated right heart pressure. |
|
|
Specialized Exam: Hepatojugular reflux
|
Another test for fluid overload (heart failure).
Patient is supine, with head at 30 degree angle. Apply firm and sustained pressure to the abdomen in the RUQ over the liver region. – Use hand or mildly inflated blood pressure cuff. Observe the neck for an increase in JVP, followed by a decrease as the hand is released. JVP will increase in all patients with this maneuver, but it is exaggerated in right heart failure. |
|
|
Abnormal S1
|
First sound produced by closure of mitral and tricuspid valves.
S1 louder than S2 at apex; S2>S1 at base. Louder S1 due to diseased A-V valve or more forceful closure of A-V valve. – Eg. Mitral stenosis, tachycardia, fever, HBP. Softer S1 due to weak contraction of heart or reduced sound transmission from thick chest wall or emphysematous lungs. |
|
|
Where is S1 best heard
|
At the apex
|
|
|
Where is S2 best heard
|
At the base
|
|
|
Abnormal S2
|
Physiologic splitting during inspiration, heard at 2nd & 3rd left interspace (pulmonic area).
Wide splitting due to delayed closure of pulm. valve (pulm stenosis; RBBB). “Fixed splitting”--does not vary with respiration (atrial septal defect, RV failure). Paradoxical splitting present during expiration and gone during inspiration; A2 follows P2 – Occurs when there is a delay in contraction of the left ventricle due to a left bundle branch block (LBBB). |
|
|
Location where S3 and S4 are best heard
|
Low-Pitched, heard best with bell at apex
|
|
|
Pathologic S3
|
Ventricular Gallop
- over age 40, usually pathologic - Due to heart failure, anemia, volume overload of ventricle, decreased myocardial contractility |
|
|
Pathologic S4
|
Pathologic due to resistance to ventricular filling; stiffness of heart muscle (reduced compliance).
– HBP, CAD, AS, cardiomyopathy – Right-sided S4 from pulm HBP or pulm. stenosis |
|
|
Aortic or pulmonic ejection click
|
High pitched; indicates valve disease or dilated aorta or pulmonary artery, or pulmonary hypertension.
Heard best with diaphragm of stethoscope |
|

|
Left Lateral decubitus position (on left side)
|
|
|
Mitral Valve Prolapse
|
Due to ballooning of mitral leaflet(s) into the left atrium during systole.
Mid-late systolic click(s) often present. Variable pitch. Mitral regurgitation may also occur, with late systolic murmur. Common condition: over 5% of general population; usually benign. |
|
|
Gradations of Murmurs
|
Grade 1/6: barely audible in quiet room.
Grade 2/6: quiet but clearly audible. Grade 3/6: Moderately loud. Grade 4/6: Loud, associated with thrill. Grade 5/6: Very loud, heard with stethoscope partially off chest; obvious thrill. Grade 6/6: Very loud, heard with stethoscope entirely off the chest, obvious thrill. |
|
|
Systolic Ejection Murmur
|
Usually crescendo-decrescendo
Usually due to blood flow across semilunar valves **From high pressure to high pressure** - KNOW THIS |
|
|
Pansystolic (holosystolic) Murmur
|
Usually plateau
Usually regurgitation across A-V valves, or VSD **From High Pressure to Low Pressure System** - KNOW THIS |
|
|
Late Systolic Murmur
|
Typical of Mitral Prolapse
|
|
|
Innocent Systolic Murmur
|
Result from turbulent blood flow, but no valvular narrowing or obstruction
No evidence of cardiac disease Usually grade 1-2, rarely 3/6 Medium pitch May disappear with sitting |
|
|
Early Diastolic Murmur
|
Usually decrescendo
usually from regurgitant flow across leaking semilunar valve |
|
|
Mid Diastolic Murmur
|
from turbulent flow across atrioventricular valves
|
|
|
Late Diastolic Murmur
|
Usually continues up to S1
|
|
|
Opening Snap Diastolic Rumble
|
Mitral Stenosis
|
|
|
"To and Fro" Murmurs
|
Systolic/Diastolic murmurs
Severe aortic regurgitation Aortic stenosis/regurgitation |
|
|
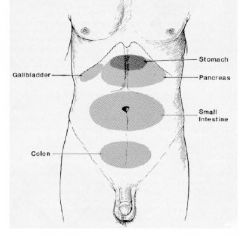
Nine Regions of the Abdomen
|
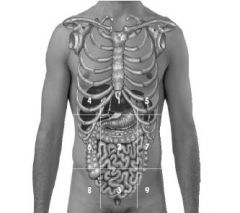
Epigastric
Umbilical Hypogastric (suprapubic) R hypochondriac L hypochondriac R lumbar L lumbar R inguinal L inguinal |
|
|
Correct Order for Abdominal Exam
|
Inspect
Auscultate Percuss Palpate |
|
|
Normal Span of Liver
|
6-12cm in MCL
Only 4-8cm in midsternal line |
|
|
Liver Palpation
|
Right fingers placed on RUQ a few cm below the costal margin (rib cage)
Left hand placed in R low back Fingers pointed toward patient’s right shoulder Fingertips near suspected lower edge of liver Have pt. take deep breath and feel for liver edge as it moves down with inspiration. – Exam is inadequate if you do not ask pt to take deep breath while you are palpating liver edge |
|
|
Spleen Examination
|
Stand on the patient’s right side and reach across
Right hand at LUQ, just below costal margin, with fingers pointing toward left lateral chest Left hand behind ribcage in low back Have patient take a deep breath; feel for spleen tip |
|
|
Kidney Examination
|
Sitting (check tenderness)
– Use gentle fist percussion at the R & L costovertebral angles Supine (palpate for size) – With your right hand on the anterior abdomen, palpate deeply to the right and left of the aorta in the kidney region. – Reach around the back with your left hand in the small of the back and lift forward so kidney is pulled slightly anteriorly. |
|
|
Pneumonic for Abdominal Pain (OLDCARTS)
|
Onset
Location Duration Character Aggrevators Relievers Treatment Symptoms (ROS) |
|
|
Pneumonic for Abdominal Pain (PQRST)
|
Provocative / Palliative
Quality Region and Radiation Severity Temporal pattern/associated symtoms |
|
|
Abdominal Vessels to Auscultate for Bruits
|
Aorta
Iliac & Femoral Arteries Renal Arteries |
|
|
Striae
|
Large purple-colored stretch marks (seen in Cushings disease and steroid use)
Large normal-colored stretch marks (seen with pregnancy, weight gain, and rapid growth) |
|
|
Linea Nigra of Pregnancy
|
Dark line of hyperpigmentation down midline of abdomen
|
|
|
Diastasis recti
|
Separation of rectus abdominus muscles
Obvious with flexion of neck |
|
|
Ascites
|
Free intraperitoneal fluid
|
|
|
Surgical Incisions
|
Subcostal incision
Median or midline Left paramedian Gridiron (muscle-splitting) - McBurney's point Transverse (abdominal) Pfannenstiel (suprapubic) |
|
|
Pfannenstiel Surgical Incision
|
Suprapubic
Generally used for C-Sections |
|
|
Hyperactive bowel sounds
|
Gastroenteritis
**Early intestinal obstruction Peritonitis (early) **Borborygmi - loud, active sounds |
|
|
High-pitched, tinkling bowel sounds
|
Obstruction
Intestinal fluid under pressure, with rushes of fluid moving through bowel |
|
|
Hypoactive bowel sounds
|
Listen for several minutes
Paralytic "ileus" - little to no bowel activity Peritonitis - may be hyperactive initially, but eventually becomes hypoactive due to progressively severe inflammation; may progress to an "ileus" |
|
|
Hepatomegaly
|
Hepatic Enlargement
Congestive heart failure Cirrhosis Hepatitis Abscess Tumor Cysts |
|
|
Shifting Dullness
|
With patient supine, percuss the border of tympany & dullness.
Have patient roll onto their side, then percuss the border again. An obvious shift in the location of the border suggests free intraperitoneal fluid. |
|
|
Palpation for Ascites
|
Check for "fluid wave"
|
|
|
Succussion splash
|
Testing for Ascites
Shake the abdomen to create a "splash" sound |
|
|
Splenomegaly
|
Enlargement of spleen
Mononucleosis Hematologic disorders Cirrhosis with portal hypertension Cysts Hypersplenism |
|
|
Palpation for Pain
|
|
|
|
Superficial Abdominal Reflexes
|
Upper abdomen
– T-7, 8, 9 Lower abdomen – T-11, 12 Cremasteric – T-12, L1, L2 |
|
|
Explosive, Excruciating Abdominal Pain
|
Coronary occlusion
Biliary colic Ruptured viscus Ruptured aneurysm Renal colic |
|
|
Severe, Constant Abdominal Pain
|
Acute pancreatitis
Bowel strangulation Mesenteric thrombosis |
|
|
Gradual-onset Steady Abdominal Pain
|
Acute cholecystitis
Acute appendicitis Diverticulitis Pelvic inflammatory disease (PID) |
|
|
Peritoneal Signs
|
Guarding
Abdominal wall rigidity Rebound / contralateral rebound tenderness |
|
|
Acute Appendicitis
|
Rebound
Psoas sign Obturator sign Rovsing's sign Rectal exam |
|
|
Psoas Sign
|
Two acceptable techniques:
1. Place your hand above patient’s right knee and have patient raise thigh against resistance 2. With pt on left side, gently hyperextend his thigh at the hip |
|
|
Obturator Sign
|
With patient supine and right knee bent, internally rotate the right leg at the hip
This stretches the internal obturator muscle which produces RLQ pain from obturator muscle irritation due to an inflamed appendix |
|
|
Rovsing's Sign
|
Press deeply and evenly in the LLQ, then quickly withdraw your fingers.
Sudden pain in the RLQ is a positive Rovsing’s sign; suggestive of appendiceal inflammation |
|
|
Murphy's Sign
|
Used to test for GB or liver inflammation
Position fingers of right hand under right costal margin, and ask patient to take a deep breath – OR -- Lay left hand flat against liver; use fist to percuss (Murphy’s punch) |
|
|
Alternate Murphy's Sign
|
Hook left thumb or fingers of right hand under right costal margin, and ask patient to take a deep breath.
– Sudden pain and an abrupt cessation of inspiration suggests cholecystitis or liver inflammation |
|
|
Grading of Pedal Pulses
|
0: Absent, unable to palpate
1+: Diminished, weaker than expected 2+: Brisk, normal 3+: Increased 4+: Bounding |
|
|
Patrick's Test
|
Patient Supine
Flex the leg to 90 degrees at hip and knee Hold knee with one hand Grasp ankle with other Swing ankle medially |
|
|
Straight Leg Raising Test (SLR)
|
Testing for impingement of sciatic nerve
Elevate Leg, dorsiflex foot |
|
|
"Flip Sign"
|
Seated SLR Test
Pt seated with pt's hands on table Extend leg Watch for pt to "flip back" when leg extends |
|
|
Bulge Sign
|
With leg straight, "milk" knee joint fluid down one side and up the other and observe for bulge
|
|
|
Lachman's Test
|
Flex pt's knee 15 degrees
stabilize thigh with one hand and pull upper tibia forward with other more sensitive sign of ACL tear than drawyer test |
|
|
McMurray's Test
|
For meniscal tear
Flex knee, place thumb and index finger on joint space Rotate foot laterally and extend leg Palpable click indicates medial meniscal tear |
|
|
Ballottement of Patella
|
Test for knee effusion
Apply downward pressure from above the knee to milk fluid down Push patella into joint space, feeling for fluid |
|
|
Stasis Dermatitis
|
Due to chronic venous insufficiency with incompetent valves and higher pressure in capillary bed
Tissue is damaged and inflamed "Brawny," non-pitting edema |
|
|
Homan's Sign
|
Test for DVT
Passive forsiflexion of the foot in a patient with calf pain, tenderness, and/or swelling Calf pain with dorsiflexion suggests DVT |

