![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
78 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
.
|
. |
|
|
|
V |
M |
|
|
|
. |
. |
|
|
|
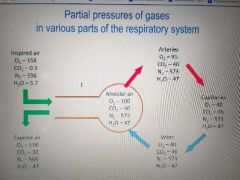
O2 co2 h20 in air alveolar air and arteries capillaries veins |
|
|
|
|
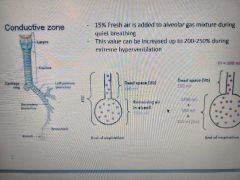
Percent of fresh air added to alveolar gas mixture in quuiet brathing and Vd FRC remaining air in alveoli and Va Vt |
Va= (Vt- Vd)* ventillation rate |
|
|
|
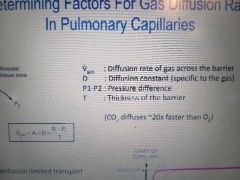
Det factors for gas diffusion rate in pulm cap |
N2oand o2 perfusion limited transport while CO diffusion limited Under special: o2 is diffusion limited as high flow rate if vlood in pcaps or fubrotic pulmonar6 wall Also there is a very long shoukser for O2 |
|
|
|
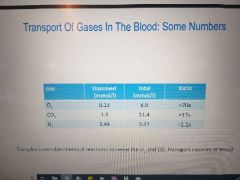
Gas3s in blood for o2 co2 n2 |
|
|
|
|
Oxygen transport |
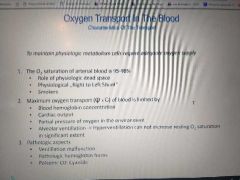
Myoglovin>fetal hb > alkalosis>hemoglov> acidosis Ordwr of sat for same Po2 hgmm |
|
|
|
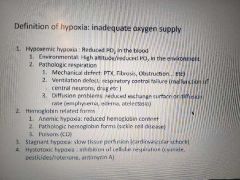
Insufficent o2 transport |
|
|
|
|
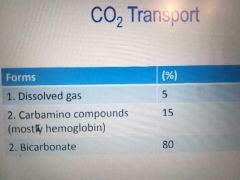
Co2 transport |
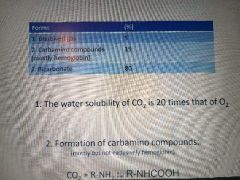
3. Formation of bicarbonate in blood as part of chloride shift Uses carbonic anhydrase to make H2CO3 from co2 and water but gives proton and HCO3 which is exchanged for chloride HbH+ dissociate to Hb K |
|
|
|
O2 and CO2 transport interactions |
Bohrs(acidosis reduces hemoglobin affinity for O2) and haldane effect(binding of O2 to hemoglobin reduces affect of CO2) PH and PCo2 |
|
|
|
Vagal afferent receptors + other |
SlowAdaptinfStretchR SARS located in smooth m of large and small bronchial airways and may be responsible for resp sinus arrhythmia: inspiration-> stretch -> afferent vagal discharge -> medullary Cv center > parasymp decreased snd symp increased so hesrt rate increases Myelinated vagal afferent fibres Rapidly adapting stretch receptors SARs rapidly adapting or irritant receptors Loc: among airway epithelium close to mucosal Respond to overinflation witj rapid adapt irritants Myelinated aff Irritant > stim irritant receptors in upper airway > n. X bronchi IX larynx and V nose > respiratory centre > coughing or sneezing and bronchoconstriction i believe gradient u get more response that just "louder" stimulus Unmyelinated C fibet endings (J receptors) loc adj to pcap (juxtacap receptors) or bronchial airways Inn by vagal fibres Respond ro chrmical and mechanical irritantsMyelinated aff Irritant > stim irritant receptors in upper airway > n. X bronchi IX larynx and V nose > respiratory centre > coughing or sneezing and bronchoconstriction i believe gradient u get more response that just "louder" stimulusUnmyelinated C fibet endings (J receptors) loc adj to pcap (juxtacap receptors) or bronchial airwaysInn by vagal fibresDischarge (weak) with changed in lung volume. PulmC: within wall ofpcap sens to products of inflammation and cause rapid shallow breathing. Also sens to pulm vascular congestion and pedema so dyspnea BronchialC: in conducting airways anf sensitive to products of inflammation and cause bronchoconstriction and increased mucus productionTemp hyperthermia increases resp ratePain long increases resp rate while susden decreasesDysnea causes stim of chest wall mechanoreceptors6ps of dysnpea: pneumothorax, pump failure pneumonia pulmonary embolsim possible foreign body pulm bronchial constriction Discharge (weak) with changed in lung volume. PulmC: within wall ofpcap sens to products of inflammation and cause rapid shallow breathing. Also sens to pulm vascular congestion and pedema so dyspnea Irritant > stim irritant receptors in upper airway > n. X bronchi IX larynx and V nose > respiratory centre > coughing or sneezing and bronchoconstriction i believe gradient u get more response that just "louder" stimulusUnmyelinated C fibet endings (J receptors) loc adj to pcap (juxtacap receptors) or bronchial airwaysInn by vagal fibresDischarge (weak) with changed in lung volume. PulmC: within wall ofpcap sens to products of inflammation and cause rapid shallow breathing. Also sens to pulm vascular congestion and pedema so dyspnea BronchialC: in conducting airways anf sensitive to products of inflammation and cause bronchoconstriction and increased mucus productionTemp hyperthermia increases resp ratePain long increases resp rate while susden decreasesDysnea causes stim of chest wall mechanoreceptors6ps of dysnpea: pneumothorax, pump failure pneumonia pulmonary embolsim possible foreign body pulm bronchial constriction BronchialC: in conducting airways anf sensitive to products of inflammation and cause bronchoconstriction and increased mucus production Temp hyperthermia increases resp rate Pain long increases resp rate while susden decreases Dysnea causes stim of chest wall mechanoreceptors 6ps of dysnpea: pneumothorax, pump failure pneumonia pulmonary embolsim possible foreign body pulm bronchial constriction |
|
|
|
Voluntary control of breathing |
Cns overides automstic reg If lost like via a stroke then ondines curse or palemon |
|
|
|
Mechanical feeback loop via vagal reflex |
Nasal receptors Pharyngeal receptoes Larygneal receptors Myelinated pulmonary R(slow adapting stretch or rapidly adapting/ irritant) Non-Myelinated pulmonary receptors: bronchial C fiber or Juxtacapillary J receptor |
|
|
|
Hering breur inflation reflex |
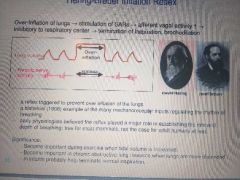
Over infl of lung > stim SARs > afferent vagal activity increases > inhibitory to respiratory centre > termination of inspiration , bronchodilation bronchodilation |
|
|
|
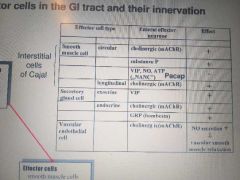
Local reflex arc in in gi |
Seratonin (on mechano chemo osmo receptors) SP CGRP (sensory neuron feeds here) to distributing neuron To either effector neuron or distributing neuron (both nAChR + ACh). Fotmer goes to longitudinal muscle thru ACh mAChR Latter goes to inhibitory and stimulitary effector neurons via nAChR+ACh to circ smooth m via NO VIP ATP or mAChR respectively |
|
|
|
Effector cells in gI and their inn. |
|
|
|
|
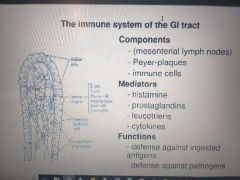
Immune system gi component mediators and functions |
|
|
|
|
Gi function and types of contractions |
Mixing, propulsion and storage (stomach and large intestine act as reservoir) Contractions: phasic (alt contraction/relaxation) in esophagus(not) and gastric antrum SI (slow wave) tonic : orad stomach and sphincters (low esophag) ileocecal and internal anal caused by continuous repetitive spike potentials Hormonal effects and Ca entry |
|
|
|
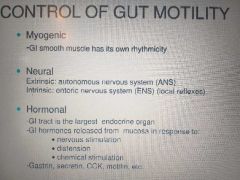
Control of gut motility |
|
|
|
|
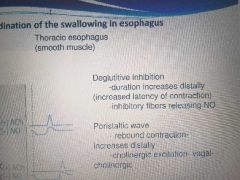
Coordination of swallowing in eso |
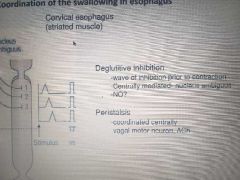
The thoracic smooth m with hint note that it was 3 nucleus ambiguus centres to c and rDMN of vagus Coordination of intrinsic and extrimsic of smooth m Primary peristalisis(forces bolus doen) initated by swalling from swallowing centre and central and intrinsic control while secondary peristalisis(if food stuck or slower than primary and are indefinite) triggered by distension if eso involuntary Nd intrinsic (indep of vag) in smooth m and causes contractions above and relaxagion below |
|
|
|
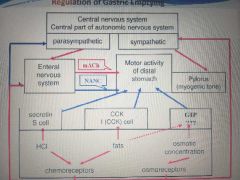
Motor activity of distal stomach and pylorus (reg of gastric emptying) |
|
|
|
|
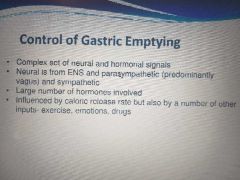
Control of gastric emptying |
|
|
|
|
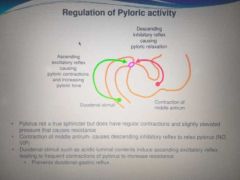
Regulation of pyloric activity |
|
|
|
|
Migrating motor complex |
Only during fasting(interdigestive) Origin midpoint of stomach and props thru SI Every 75 90 minutes Housekeeping function as fascil trans of indigestible substances past iliocecal sphin into colon Also trans bacteria from SI toLI and inhibits inti twrminal ileum Increased gastric biliary pancreatic secretion accomp by MMC(overriden by ingestion of meal) Blood levels of drugs thats why intake b4 ir after |
|
|
|
Motilin and mmc |
Former by M of SI and major reg of MMC between meals and assoc with PHASE 3 Increase at reg interval maybe due to luminal pH and bile. May involvr serotonin release in duodenum M3 receptor Vagotomy doesnt inhibit Motilin receptors in ENS and smooth M. Erythromtxin antibiotic is motilin agonist useful in patients with Decreases GI motility |
|
|
|
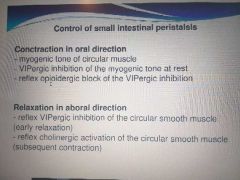
Control of intestinal peristalisis |
|
|
|
|
Control of SI motility |
Slow wave Freq highest in duodenum and lowest ilium Amplitude and frequency by neural and hormonal via parasymp stim increase motility and sympth decrease motility Enteric n. both stim and inhib Luminal contents affect intestinal contractility to maximise |
|
|
|
Motility of LI |
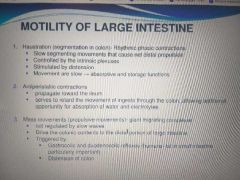
|
|
|
|
Opoids effect on GI motility |
Mu opioid receptors in gut Myenteric SM plexus opioids inhibit both inh and exc n to inhibit peristalisis and elevate resting tone Delay gastric emptying Slow intestinal transit In sm plexus inhibit wayer ans electrolye secretion and increase abs Central mechanisms:intracerebral or intrathecal inj of opioids can inhibit GI motility |
|
|
|
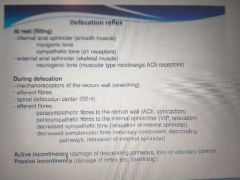
Defecation reflex |

|
|
|
|
Vomiting |
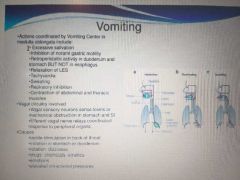
|
|
|
|
Control of gall bladder emptying |
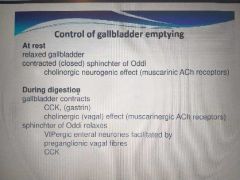
Oddi closed by myogenic tone of mAChR and ipened by CCk and vagal n thru nAChr on enteric n that gives VIP and NO |
|
|
|
Functional anatomy vs Physiological anatomy |
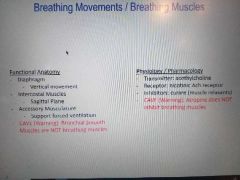
|
|
|
|
Surfactant components |
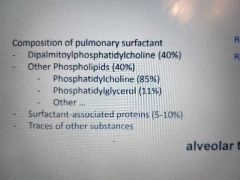
|
|
|
|
V-P graph for lung chest and the net forces |
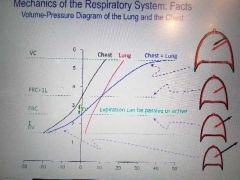
From negative so net pressure is out then equL then lung in then botj in |
|
|
|
Pressure changes in ventilation cyclr |
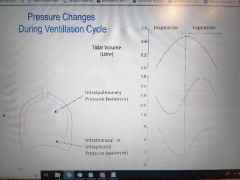
First its in watercm TV 0 to 0.5 then 0 Intrapulmonary 0 to negative 1(mid of ins) to 0 then 1(mid of exp) to 0 Intrathoracal or intrapleural pressure is from -5 to -7 then rapid to slow to -5 |
|
|
|
Lung volumes |
Only 1/6 used 0.5 fresh to 2.5(ERV)from normal exhale to deepest + RV 1.5(RV) to deepest exhale 0.5TV is from inhale to exhale IRV is from deepest inhale to inhale and its 2.5 so till 5.5 VC is from deepest exhale to deepest inhale |
|
|
|
Flow volume loop |
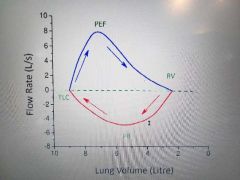
TLC is VC(vital cap) or total lung capacity Obstructivr asthamtic vs restrictive emphysema i think is thay in restrictive we dont maintain width but higher tjsn obstructive |
|
|
|
Dynamic parameters of lung |
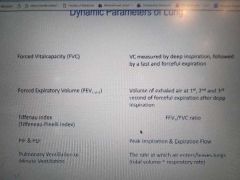
Tiffenaeu shoulnt br lower than 80 |
|
|
|
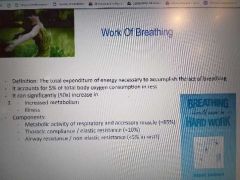
Composition of the work for breathing and when does it significantly increase What percentage of total oxygen consumption at rest? |
|
|
|
|
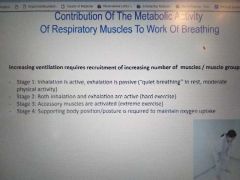
4 levela of breathing |
|
|
|
|
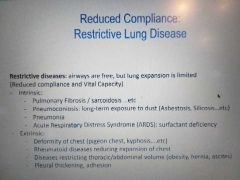
Reduced compliance |
|
|
|
|
Laminar flow,turbulent flow and reynolds number equations |
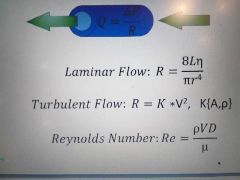
Flow is delta p over R |
|
|
|
Determinants of airway resistance |
As vol increases the total lung resistanxe in watercm per l per s decreases in an 1/x fashion Airway resistance however increases from trachea all the way to bronchus and RAPIDLY decreases to terminal bronchioles |
|
|
|
Distribution of airway resistance |
|
|
|
|
Importance if Reynolds number |
Determines airway resistance Decreasing diameter decreases Re and increasinf longitudinal velocity increases R Increased ventillation extends the turbulent flow zone |
|
|
|
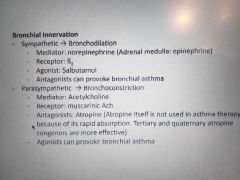
How inn determines airway resistance |
|
|
|
|
Rate dep kf work of breathing at constant minute vol |
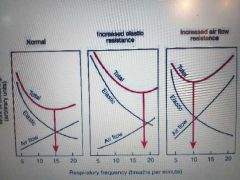
Y axis is work of breathing |
|
|
|
Increased airway RESISTANCE |
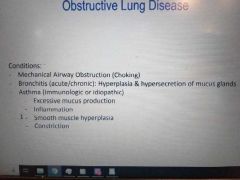
|
|
|
|
Fresh air and FRC |
15 percent in quite breathing Increases to like 200 to 250 percent in extreme hyperventilation Functional residual capacity: ERV + RV and its also equal to Vd of 150 + remaining air in alveoli of 2350 |
|
|
|
Relationship between alveolar ventiliation and Partial p of gases in alveolar air |
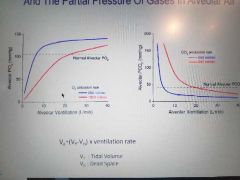
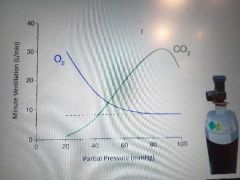
As Alv vent rate increases the Lveolar PO2 increases rapidly then slowly with a low O2 utilization rate reaching "shoulder" much earlier. For CO2 same concept but production. Normal is 110 and 40 approximately respectively. |
|
|
|
Vgas |
|
|
|
|
Time along capillary which gases reach alveolar partial pressures first |
N2 rhen o2 if normal with both really long shoulder reserves while O2 i diffusion limited doesnt. CO is diffusion limited so never reaches. |
|
|
|
CO2 transport contribution percentages |
|
|
|
|
Relationshio between plasma pH and bicarbonate concentrations |
The siggaar-Andersenn Acid-Base chart Normal to chronic resp alkalosis(least) is via less pCO2 (and plasma HCO) then acute resp alkalosis(most alkaline) if technically only less pCO2 and lowest H+ then metabolic alkalosis if really high pCO2 and HCO Then chronic acidosis if less pCO2 but mainly HCO and increase H+ Acute resp acidosis and metabolic acidosis botj have highest pH and H+ but metabloic has lowest pCO2 and HCO So metabolic seem to be associated with HCO and CO2 but acute with H and CO2 (tiniest change) while chronic with CO2(highest change) HCO and tiny but visivlr H |
|
|
|
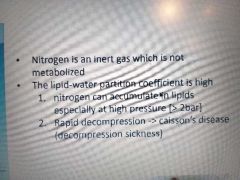
Nitrogen transport |
|
|
|
|
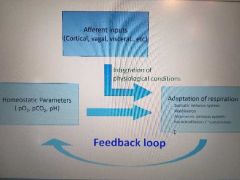
Afferent inputs vs Homeostatic parameters, feedback loop and how resp is adapt |
|
|
|
|
Components of Vent feedback loop reflex arc |
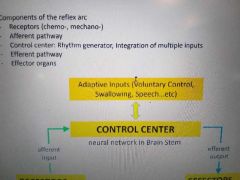
Effectors being insp and exp m while receptors being chrmo anf mechano receptor |
|
|
|
Peripheral chemoreceptors |
In multiple locations and detect hypoxia which inhibits potassium channels cause depol so calcium enters and fascilitates vesicle and neurotrans and stims mitochondria to increase amp atp ratio to give mote AMPK THAT INHIBITS POT Aortic via vagal Carotid body via glosso |
|
|
|
How Partial p of O2 and CO2 affect minute ventillation |
|
|
|
|
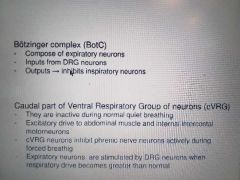
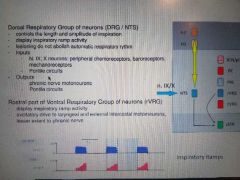
Expiratory premotor groups |
|
|
|
|
Inhibitory premotor groups |
|
|
|
|
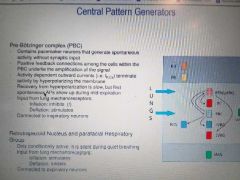
Central pattern generators and inputs! |
|
|
|
|
Pontine circuits |

Eupnea is 0 apneu is max long and gasping is maz short Aupneustic centre inhibited by vagal |
|
|
|
Characteristics if phrenic activity during eupnea |
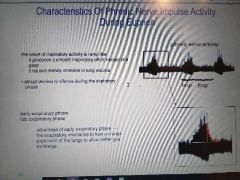
|
|
|
|
Physiological cs pathological breathing patterns |
Normal 12 to 20 Slower then bradynpea Faster then tachypnea Hyperpnea is faster + deeper Kussmaul is REALLY RAPID DEEP AND LABORED LIKE BARCODE Sighing is 1 deep + n shallow Air tapping increasing difficulty in getting breath out Cheyne stokes is varying periods of increasing depth but regular + apnea Biot is irregular apnea with irregular but same depth Ataxic is irregular depth and raye with irregular apnea |
|
|
|
Mechanical and chemical functions and abs of MOUTH PHAR ESO CAR STOM PYL SI ILIOCECAL VALVE LI RECTUM |
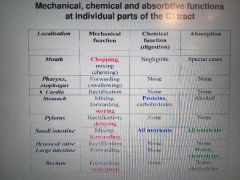
|
|
|
|
Coordination of mech and chem + how neuron coung of ent n sys affects |
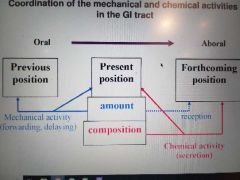
More n mainly control neuron Fewer n control secretion and absorption |
|
|
|
Connections of autonomoc NS and GI + reflexes |
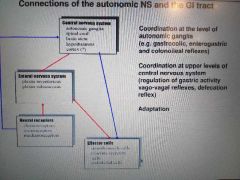
|
|
|
|
Parasym effect on GI |
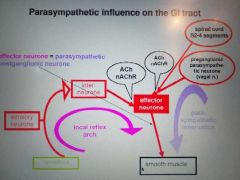
|
|
|
|
Symp influencr on GI |
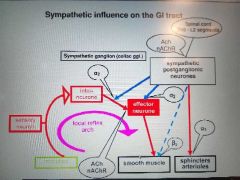
|
|
|
|
Properties of signalling molecules of GI |
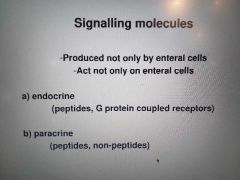
|
|
|
|
Fundic gland cell secretions and mechanism of enteroendocrine |
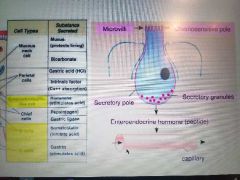
|
|
|
|
Principles of own regulation- GI and how CCK levels change after food intake |
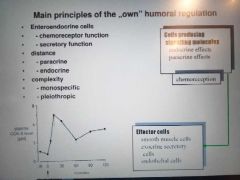
|
|
|
|
Most significant GI hormones : D L(A) F ... etc |
D Localised: stomach closed to parietal and ECL + Pancreas Peptide: somatostatin Effect: paracrine inhibition of neighbouring secretory cells Stim: low pH in stomach cuz i think we want less H released
L: pancreas(A) SI (L) Peptide: glucagon GLP etc Main effect: carbohydrate metabolism to elevate plasma glucose Increase insulin secretion and prolif of intestinal mucosa( GLP)
F stim by ACh and low vlood sugar because i think it allows mofe glucose to be abs? SI and pancreas PP Slows abs and inhibits pancreas function
S DUODENUM by food and H+ cuz it wants to neutralise acid i think Secretin Secretion of panc juice and bile
M SI Motilin Increasing motility of stomach and tract during interdigestive
gip or k Intestinal mucosa GIP Inhibit HCL sec Facilitate insulin sec
ECL stomach by gastrin Histamine Fac HCL sec
Enterochromaffin Gastric and intestinal mucosa 5 HT ? G antrum SI oral segments stim by aa GRP and stress I in duodenun and jejenum stim by food |
|
|
|
Processing if proglucagon |
The L/A cells peptides are all formed from proglucagon by diff cleavages in 2 locations Pancreas gives GRPP Glucafon and heavy proglucagoj fragment Si: glicentin (further broken to GRPP and oxynto modulin) GLP1 and 2 |
|
|
|
Gastrin and CCK |
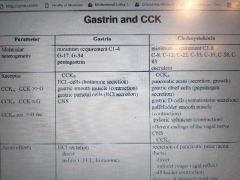
Molecular heterogeneity Recsptor Acute effects hcl sec directly and indirectly via ecl his VS ____ secretion of panc juic direct and indirectly via vagovagal reflex, gall bladder contraction and slow stomach empty anx increase intest motility and decreased food intake SO IT FEELS LIKE IT PROMOTES UTILIZING WHAT IT HAS WITH PATIENXE Long lastinf effects BOTH PROLIF TARGET CELLS (GROWTH FACTORS) |
|

