![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
46 Cards in this Set
- Front
- Back
|
- Adults age 65 years and older currently comprise approximately _____ % of the
US population but consume ____% of all RX drugs and ____ % of all OTC meds. - Medication use steadily increases with age in older adults because of ______________________________________. |
- Adults age 65 years and older currently comprise approximately 13% of the
US population but consume 30% of all RX drugs and 40% of all OTC meds. - Medication use steadily increases with age in older adults because of INCREASING COMORBIDITY |
|
|
What is polypharmacy
|
Administration of of several drugs concurrently
|
|
|
What are age-related pharmacokinetic changes that may influence drug therapy?
Absorption: Outcome? |
-Decreased gastric emptying rate.
-Decreased intestinal motility -Decreased intestinal blood flow -Decreased intestinal surface area -nonsignificant decreased gastric acid output and increased gastric pH Outcome: No significant change in quantity absorbed; time to onset or peak may be delayed. |
|
|
What are age-related pharmacokinetic changes that may influence drug therapy?
Distribution: Outcome? |
-Increased body fat,
-Decreased muscle mass -Decreased body water -Decreased cardiac output -Altered regional blood flow Outcome: INCREASED Vd of lipid soluble meds(allow sufficient time for ss.) DECREASED Vd of water soluble meds(LOWER doses) |
|
|
What are the pharmacokinetics of concern in older pts?
|
Absorption, Distribution(protein binding), metabolism, metabolism, Clearance(Renal, hepatic, etc)
|
|
|
What are age-related pharmacokinetic changes that may influence drug therapy?
Distribuiton(Protein binding): Outcome? |
-Decreased serum albumin
-Decreased protein affinity -almost same but Increased Alpha1-acid glycoprotein(AAG) Increased free fraction of highly protein bound meds(phenytoin, warfarin) |
|
|
What are age-related pharmacokinetic changes that may influence drug therapy?
Metabolism: Outcome?(PI,PII, CYP 450 activity enzyme induction/inhibition) |
-Decreased hepatic mass
-decreased hepatic blood flow Outcome: Phase 1(oxidation,reduction): decreased Phase 2(conjugation): unchanged CYP450 activity: unchanged enzyme induction/inhibition: controversial |
|
|
Cancer of the Bone - primary - adults
|

Multiple Myeloma
|
|
|
|
|
|
a. What are age-related pharmacodynamic changes that may influence drug therapy?
b. when are p-dynamic changes assumed? |
a. Homeostatic mechanisms
Receptor and postreceptor mechanisms b. P-dynamic changes are assumed when p-kinetic changes do not explain alterations |
|
|
What are age-related pharmacodynamic changes that may influence drug therapy?
Homeostatic mechanisms: |
Homeostatic mechanisms provide the means by
which the body can adjust or counteract a particular drug effect. For example, in a young adult taking mor- phine, the expected depression of the respiratory center is counteracted by reflex stimulation of the respiratory system. In older patients taking morphine, however, blunted homeostatic mechanisms predispose to respira- tory depression; sedation and constipation may also result if the drug is given at doses meant for younger patients. Less active baroreceptor reflexes may predis- pose geriatric patients on antihypertensive drugs to pos- tural hypotension, and an impaired thermoregulatory response to cooling may predispose those taking barbi- turates or phenothiazine to hypothermia. 13 |
|
|
Which is better understood, p-dynamics or p-kinetics? Why?
|
P-kinetics are more understood. There are more variables in p-dynamics because changes are seen in: # of receptors, sensitivity of receptors, counter reulatory mechanisms
|
|
|
PHARMACODYNAMICS:
Increased or decreased. 1. receptor sensitivity(benzos, CNS depressants) 2. receptor sensitivity( Beta-adrenergic receptors) 3. baroreceptor sensitivity(OH with vasodilators, TCA's antihypertensives) 4. risk of tardive dyskinesia and parkinsonism with antipsychotics 5. sensitivity to anticholinergic effects 6. sensitivity to warfarin 7. sensitivity of Na+, K+ ATPase- increased toxicity to digoxin, esp, w/ hypokalemia. 8. renin and aldosterone levels- -response to ACE inhibitors and beta-blockers -INCREASED risk of _?__ a with NSAIDs, ACE inhibitors and K+ sparking diuretics |
1. INCREASED receptor sensitivity(benzos, CNS depressants)
2. DECREASED receptor sensitivity( Beta-adrenergic receptors) 3. DECREASED baroreceptor sensitivity(OH with vasodilators, TCA's antihypertensives) 4. INCREASED risk of tardive dyskinesia and parkinsonism with antipsychotics 5. Increased sensitivity to anticholinergic effects 6. Increased sensitivity to warfarin 7. INCREASED sensitivity of Na+, K+ ATPase- increased toxicity to digoxin, esp, w/ hypokalemia. 8. DECREASED renin and aldosterone levels- -DECREASED response to ACE inhibitors and beta-blockers 9. INCREASED risk of hyperkalemia with NSAIDs, ACE inhibitors and K+ sparking diuretics |
|
|
What are age-related pharmacodynamic changes that may influence drug therapy?
REceptor and postreceptor mechanisms(A-adrenergic, B-adrenergic, opiod receptors) |
It is theorized that changes in the sensitivity of recep-
tors occur with aging. Sensitivity of receptors may decrease, increase, or remain unaltered. For example, the activity of β- adrenergic receptors diminishes with age; the observed diminution in activity may be from changes in receptors or post-receptor sites. 13 Therefore, a larger dose of β- agonist or antagonist agents may be required to produce a given response. On the other hand, increased sensitivity of receptors is noted with opioids and benzodiazepines, with a resultant increase in side effects. Lastly, no change in activity is noted with α-receptors; α-blockers and agonists are expected to produce the usual response in geriatric patients. |
|
|
Which classes of medications should be used with caution in older adults?
|
-Oral hypoglycemic agents: avoid sulfolyurea chlorpropamide, renal, hypoglycmia.
-Antidepressants(some anticholinergic and sedative). all may cause hyponatremia. -Anxiolytics. avoid long acting, avoid falls. -Antipsychotics-as needed only -Antiepileptic drugs - phenytoin -Cardiac meds - decrease digoxin. -Anticoagulant and ANtiplatelet Meds-3x more likely to bleed from heaprin, hyperkalemia, thrombocytopenia -Analgesia-Tylenol appears safe. Anithistamines anticholinergic and CNS effects -Diuretics-HCTZ is hyponatremia, hypokalemia, and delirium |
|
|
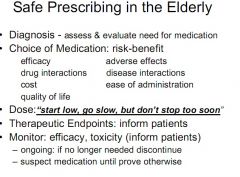
Key principles of prescribing in older adults? 8
|
1. Know the diagnosis
2. Conduct med review regularly 3. Do not prescribe when in doubt 4. Empower pts and caregivers by education 5. Know well the drugs you prescribe 6. Start low, go slow 7. Be neither the firs tnor the last to use a new drug. 8. Write legibly |
|
|
In what ways can you encourage compliance among older adult pts? (6)
|
1. Educate pt and/or caregiver
2. SImplify drug regimin 3. Provide clear dosing instructions 4 Encourage use of pillboxes 5. consider cost when prescribing 6. monitor for compliance |
|
|
What are some example of dosing circumstances that pose challenges in prescribing for the older adult?
|
Not enough dosing options. No support RCTs for lolder adults. Start low but dont be subtherapeutic. Titrate up to reach levels
|
|
|
ADEs would be ranked?
|
number 5 cause of death in US
|
|
|
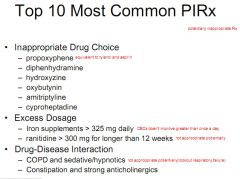
How might the beers list be used or how has it been used
|
list of medications that are generally considered inappropriate when given to elderly people. Widely used over the past 10 years for studying prescribing patterns w/in populations, educating clinicians, and evaluating healthy outcomes, cost, and utilization data.
|
|
|
What are some weaknesses of the Beer's list?
|
with the continuous arrival of new drugs on the market, icnreased knowledge about older drugs, and removal of older drugs, and removal of older drugs from the market, these criteria must be updated on a regular basis to remain useful. Lack of studies done on older pts.
|
|
|
Elderly account for __% of total annual Rx Spending in the US
|
42%. $43 billion of $102 billion.
|
|
|
It is now ____ that poses a threat to our nation's health and economic well-being
|
Chronic diseases
|
|
|
look at High Severity in Beers list Table 1 and 2.*
|
look at High Severity in Beers list Table 1 and 2.
|
|
|
Order these from greatest to least prevalent:
Stroke, Cancer, OP, AD, HTN, arthritis |
HTN, Arthritis, Osteoporosis, Cancer, Stroke, AD
|
|
|
___ are probably the single most important health care technology in preventing illness, disability, and death in the geriatric population.
|
Medications
|
|
|
An undesireable event experienced by a patient
-Involves or is suspected to involve drug therapy -Actually or potentially interferes with a desired patient outcome |
Medication Related Problems
|
|
|
What is the Highest cost of MRP?
|
Ambulatory cared, followed by nursing and hospitals
|
|
|
What are the 8 categories of MRPs? Which is number 1?
|
1. Untreated indication(winner)
2. Drug use without indication 3. Failure to receive drugs 4. Drug interaction(potential/actual). 5. Adverse drug reaction 6. Correct drug, dose too low. 7. Correct drug, dose too high 8. Improper drug selection |
|
|
What are some risks for MRPs?
|
• Multiple chronic diseases
• Multiple prescribers • Multiple medications • Types of medications prescribed • Under-representation in clinical trials, particularly those over age 75 • Shortage of trained professionals in geriatric pharmacotherapy |
|
|
These are all examples of which MRP?
• Depression in the nursing home Lebowitz BD. JAMA 1997. • Osteoporosis in the nursing home Bellantino S. JAGS 2001. • Atrial Fibrillation/Anticoagulation Bungard TJ. Arch Intern Med 2000. • Hypertension DiBari M. J HTN 1999. • MI primary/secondary prevention DiBari M. J HTN 1999. • Opioids: fear of addiction AGS Guidelines. JAGS 1998. ective 11, 13 |
Untreated indication(enough info to indicate a condition but they are not being treated)
|
|
|
This MRP is really common with transitional care
|
Drug Use without indication
|
|
|
a. What is estimated % of noncompliacne and what is noncompliance associated with?
|
26-59% assoicated with Higher socioeconomic status, Greater number of prescribed medications, higher psychological stress
|
|
|
These are all reasons for what MRPs?
• Lack of understanding or misinterpretation of directions. • Sensory impairments • Drug regimen interferes with daily activities. • Drug regimen is too complex.* • Lack of understanding why the medication is important or the goals of therapy. • Doesn’t believe the medication will work or is even necessary. (or too expensive) • Numerous providers. |
noncompliance
|
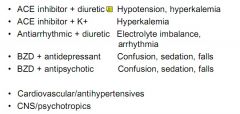
|
Place:
Confusion, sedation, falls(2) Hyerkalemia(2) Hypotension Electrolyte imbalance Arrythmia |
|
|
|
% of hospitilization of elderly due to ADR(%) and Non-compliance(%)
|
28%
17% 11% |
|
|
% ADEs predictable
|
95%
|
|
|
% serious. life-threatening. Fatal
|
ADEs
|
|
|
Female gender and small body size RF for...
|
ADRs
|
|
|
Any symptom in an elderly pt should be considered __ until proved otherwise
|
drug side effect
|
|
|
Prevent ADE by ALWAYS considering this as possible consequence of current drug tx
|
S/S
|
|
|
Symptoms of MRP(10)
|
• Confusion
•Depression • Delirium • Insomnia • Parkinson’s-like symptoms • Incontinence • Weakness or lethargy • Loss of appetite • Falls • Changes in speech |
|
|
What drug would:
1. Start low then adjust up until ADRs, then go down? 2. Start low, get to goal 3. Start low, stay low |
1. Beta-blockers
2. Warfarin 3. THiazide |
|
|
Beers List
|
Pentazocine (Talwin) Flurazepam
(Dalmane) TCAs Long half-life psychotropics Digoxin > 0.125mg QD Methyldopa (Aldomet) Dicyclomine (Bentyl) All barbiturates except phenobarbital |
|
|
|
|
|
|

