![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
85 Cards in this Set
- Front
- Back
|
Name four main mechanisms for antibiotic resistance in bacteria
|
1. Gram Neg - altering porin stricture and preventing beta lactamases from entering
2. Gram +/- - Beta Lactamase enzymes cleave beta lactame rings of transpeptidase inhibitors 3. Gram+/- altering the molecular structure of transpeptidases 4. Gram+/- can actively pump out transpeptidase inhibitors |
|
|
What are the adverse effects of penicillins?
|
Because penicillins are made from fungal compounds, many can cause allergic reactions (IgE mediated) - bronchospasm, urtricaria, anaphylactic shock plus diarrhea by destroying the normal gut flora
|
|
|
What is the therapeutic spectrum for beta-lactamase sensitive penicillins?
|
Penicillin G and V -
Streptococci, Pneumococci (Strep pneumonia), meningococci (Neisseria meningititis) and Treponema Pallidium (syphillis) |
|
|
Best drug to treat Gram + enterococci
|
Ampicillin, Amoxicillin
|
|
|
Best drug to treat meningitis caused by Listeria Monocytogenes
|
Ampicillin, Amoxicillin
|
|
|
Best drug to treat peptic ulcers
|
To eradicate H Pylori, use Amoxicillin in combination with Clarythromyocin and PPI
|
|
|
Name common pathogens causing Otitis Media in children and the drugs that can treat it
|
H Flu, S Pneumoniae, Moraxella Cataralis
Treat with Amoxicillin or Augmentin (Amoxicillin plus Clavulanate) |
|
|
Drug of choice for Staph Aureus infections (endocarditis, cellulitis, sepsis)
|
Nafcillin (Treat Staph with Naf)
|
|
|
First line of choice for MSSA
|
Cloxacillin, Oxacillin, Methicillin and Nafcillin
|
|
|
Best treatment for MRSA
|
Vancomycin
|
|
|
Best treatment for Pseudomonas infections
|
Ticarcillin, Carbenicillin, Piperacillin (A Piper fixing a car carburator)
|
|
|
First generation cephalosporins
|
Most have PH in them - must get your PhD in PHarm first!: Cephalothin, Cephapirin, Cefazolin.
These treat PEcks (Proteus Mirabilis, E. Coli, Klebsiella Pneumonia) |
|
|
Second generation cephalosporins
|
Cefuroxime, Cefaclor, Cefoxitin (Foxy Fur Cefa)
Now treating HEN PEcKs (H Flu, Enterobacter, Neisseria, Proteus Mirabilis, E Coli, Klebsiella Pneumonia, Serratia Marcescens) |
|
|
Third generation cephalosporins
|
Have T in them for "Three": Ceftriaxone, Cefotaxime, Ceftazidime.
Treat serious Gram - infections resistant to other beta-lactams: Meningitis caused by H Flu and Pneumococcus, Ceftrizidime for Pseudomonas, Ceftriaxone for gonorrhea |
|
|
Forth generation cephalosporin
|
Cefepime - increased activity for Pseudomonas and Gram + organisms
|
|
|
Best drug to treat community acquired pneumonia
|
Strep Pneumonia and H Flu are the two most common causes of CAP. Also, H Flu and Moraxella Cataralis are common causes of sinusitis and otitis media.
Use Cefuroxime (you need to have some fur to cover you and prevent pneumonia or URI or otitis media) |
|
|
The first line for treating meningitis in neonates, children and adults
|
Ceftriaxone (third generation cephalosporine that can access axons through the BBB)
|
|
|
What drug can be used in Penicillin allergic patients to treat Gram Negative Aerobes
|
Ex. Pseudomonas
Aztreonam is a magic bullet for gram negative bacteria. Has little cross-reactivity with Penicillins. Can use in addition with Gram positive coverage (like Vancomycin + Aztreonam or Clindamycin + Aztreonam) |
|
|
What can be used to treat bacterial meningitis empirically?
|
Chloramphenicol - kills most clinically important Cram +/- and anaerobic bacteria (even Bacteroides Fragilis)
|
|
|
Side effects of Chloramphenicol
|
Bone marrow supression (from anemia to severe aplastic anemia)
Gray baby syndrome - neonates are unable to conjugate Chloramphenicol in their liver and excrete it through the kidneys -> toxicity causes vasomotor collapse, abdominal distension and cyanosis |
|
|
Gray baby syndrome
|
Chloramphenicol - because neonates cannot conjugate it in their liver and later excrete through the kidneys
|
|
|
Clindamycin
|
Inhibits bacterial 50S ribosomal subunit. Works against Gram + and anaerobes (including Bacteroides Fragillis)
Used in dental and general surgeries, for prophylaxis of bacterial endocarditis in dental surgeries. Used to treat aspiration pneumonia, abdominal and pelvic absseses. |
|
|
What causes Pseudomembranous Colitis?
|
Treatment with Clindamycin can lead to overgrowth of Clindamycin - resistant C. Difficile. Treat with Metronidazole (Preferr Metro as Choice PMC)
|
|
|
What is used to treat anaerobic aspiration pneumonia?
|
Clindamycin
|
|
|
What is the major side effect of Clindamycin?
|
Pseudomembranous Colitis
|
|
|
Treatments for Pseudomembranous Colitis
|
Oval Vancomycin or, the method of choice, is Metrodidazole
|
|
|
Linezolid
|
Godzilla Lizard - active against Gram + bacteria.
Often used in combination with broad spectrum beta-lactem for treating hospital aquired pneumonia and MRSA. Can be given orally, so can be used in outpatients |
|
|
Linezolid side effects
|
Thrombocytopenia and reversible neutropenia
|
|
|
What are macrolides used for?
|
Erythromycin (a wreath), Azithromycin, Clarithromycin are macrolides, used to treat many Gram +, some Gram - and atypicals, such as Legionella, Chlamydia and Mycoplasma (imagine a soldier from the French Legion of Honor who dies of Legionella indiced pneumonia. The tomb is in the shape of a cross with a wreath on it.
|
|
|
Name the first line drug for treating atypical phenumonia as well as the second line drug for treating Staph skin infections
|
Macrolydes: Erythromycin, Azithromycin. Block 50S bacterial subunit.
Treat Chalmydia pneumonia, Mycoplasma pneumonia amd Legionella Phenumonia. |
|
|
First line for Legionella Pneumonia?
|
Macrolydes: Erythromycin, Azithromycin. Block 50S bacterial subunit.
|
|
|
First line for Chlamydia Pneumonia?
|
Macrolydes: Erythromycin, Azithromycin. Block 50S bacterial subunit.
|
|
|
First line for Mycoplasma Pneumonia?
|
Macrolydes: Erythromycin, Azithromycin. Block 50S bacterial subunit.
|
|
|
Name the main side effects of tetracycline/doxycycline
|
1. GI disturbances: nausea, vomiting
2. Phototoxic dermatitis 3. Renal and hepatotoxicity 4. Discolered teeth and depressed bone growth in children due to chelated calcium |
|
|
First line for treating venerial chalmydial infections, walking pneumonia (caused by Mycoplasma), Brucella and Rikettsia diseases as well as acne treatment
|
Tetracycline and Doxycycline
|
|
|
Ghon focus
|
Primary TB
|
|
|
What is Disulfiram and what drugs can cause a disulfiram-like reaction?
|
Disulfiram is a antiabuse drug used in alcoholics. It inhibits Acetaldehyde Dehydrogenase --> acetaldehyde accumulates and causes nausea and vomiting, HTN and sweating.
|
|
|
Give examples of conjugation reactions (Phase II)
|
Glucoronidation
Sulfation Acetylation O- and S-Methylation Glutathionine conjugation |
|
|
Give examples of non-synthetic (Phase I reactions)
|
Hydroxylation
Oxidation Dealkylation Polarizing atom exchange |
|
|
Name several inducers of P450 activity
|
Phenobarbital
St. John's Wort Polycyclic aromatic hydrocarbons |
|
|
Name several inhibitors of P450 activity
|
Grapefruit juice
All azole drugs (eg Omeprazole) Cimetidine Macrolides |
|
|
Define Pharmacodynamics
|
What the drug does to the body.
Essentially, drug effects involve: - Receptor binding - Agonist, antagonist or partial agonist - Target effects (beta blocker, H2 antagonist,…) - Side effects |
|
|
Define Pharmacokinetics
|
What the body does to the drug. this concerns:
Absorption Distribution Metabolism Excretion |
|
|
Define Efficacy of a drug
|
The maximal effect that a drug can produce.
Determined mainly by the properties of the drug and its receptor/effector system Important clinical parameter |
|
|
Define Potency of a drug
|
The amount of a drug needed to produce a given effect (often as EC50 or ED50)
Determined mainly by the affinity of the drug for the receptor Potency affect drugs dosage |
|
|
Define Agonists, Antagonists and Partial Agonists
|

Drugs that bind to a receptor and mimic the effect of an endogenous ligand are called agonists.
There are other types of drug receptor interactions that can occur that are shown here graphically. If a drug produces less than a full effect even at doses that saturate the receptor, it is a partial agonist. Partial agonist are less efficacious. An antagonist is a drug that binds to a receptor but does not produce an effect. Antagonists produce a pharmacological effect by inhibiting the effect of an agonist. |
|
|
Describe the effects of competitive and non-competitive antigonists
|
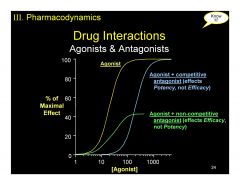
A competitive antagonist combines reversibly with the same binding site as the agonist or active drug and can be displaced from the binding site by an excess of the agonist. The maximal effect of the agonist can still be achieved if sufficient agonist is used. A competitive inhibitor lowers the potency of the agonist but does not alter its efficacy.
A non-competitive antagonist binds irreversible to the receptor binding site or interacts with other components of the system to decrease or eliminate the effect of the drug binding to the receptor. A non-competitive antagonist prevents the agonist, at any concentration, from producing its maximum effect. Typically, the dose response curve with this type of antagonist reveals reduced apparent efficacy, but the potency is not altered. |
|
|
Low efficacy partial agonists act as...
|
Low efficacy partial agonists (e.g. pindolol & other b- blockers with ISA) almost always act clinically as antagonists.
|
|
|
Moderate efficacy partial agonists act as...
|
Moderate efficacy partial agonists (e.g. xamoterol, a b1 partial agonist) act as agonists with low and moderate underlying (sympathomimetic) activity (e.g. moderate heart failure) BUT as antagonists with high underlying (sympathomimetic) activity (e.g. severe heart failure)
|
|
|
High efficacy partial agonists act as...
|
High efficacy partial agonists (e.g. buprenorphine) almost always act as full agonists except following excessive dose of agonist when they act as antagonists
|
|
|
What is Theraupetic Index?
|

Example:
The TD50/ED50 ratio for the drug shown on the previous graph is about 2.5, which means that about 2.5 times as much drug will cause a toxic effect in half the subjects as is needed to produce a therapeutic in the same proportion of subjects. However this ratio of toxic to therapeutic dose may not hold across the entire dose range if the dose-effect curves are not parallel. |
|
|
What is bioavailability and how is calculated?
|

Bioavailability (F) is the fraction of the administered drug that reaches the systemic circulation.
Drug bioavailability is a key factor in determining the onset of drug action F = 1 (100% absorption) for i.v. drug administration and usually <1 for oral drug administration. |
|
|
What is a Volume Distribution of the drug
|
Apparent volume of body water that drug appears to distribute into to produce a drug concentration equal to that in the blood.
Vd=Dose/Plasma Concentration |
|
|
What is a standard distribution of fluids within the body?
|

|
|
|
Loading Dose
|
LD = Vd x Cp
|
|
|
Name major routes of drug elimination
|
1. Renal excretion through urine is the major route
2. Glomerular filtration rate depends on size (<40kDa), charge, & protein binding Drugs not bound / reabsorbed cleared at creatinine rate (125ml/min) 3. hepatic (through bile) 4.Sweat, saliva are insignificant routes of elimination 5. Lactation is insignificant for maternal elimination, but may present a considerable ROA for a nursing infant 6. Coexisting pathology (kidney, liver, heart) can affect renal and hepatic drug elimination |
|
|
What is Clearance?
|
Clearance (CL) is the apparent volume (in liters) of blood that is cleared of a drug per unit time (min or h)
Predicts the rate of elimination in relation to the drug concentration CL = K x Vd where K is an elimination rate constant |
|
|
What is Half Life of a drug?
|
t1/2 (the time it takes for the concentration to fall to half of its previous value) is a ‘secondary’ pharmacokinetic parameter and depends on clearance (CL) and volume of distribution (Vd)
t1/2 = 0.693 x Vd/CL |
|
|
Penicillin G
|
Mechanism: inhibits cell wall synthesis by binding to and inhibiting transpeptidase (PBP)
Toxicity:well tolerated, allergic reactions are the major toxicity (can cause anaphylatic reactions - IgE-mediated). Complete cross alergenicity among other penicillins and 10% among other beta-lactams. Niche Therapeutics: Streptococci (except Penicillin resistant S. Pneumoniae) Spirochetes (T. Pallidum - syphilis) Cleaved by Beta-Lactamase |
|
|
Aminopenicillins (Ampicillin and Amoxicillin)
|
"AMPed up penicillins"
Mechanism: same as Penicillin but wider spectrum, penicillase sensitive). Can also combine these with Clavulanic acid to to enhance spectrum. Toxicity: hypersensitivity reactions, amphicillin rash Niche Therapeutics: like penicillin plus "wimpy aerobic gram negatives - Amoxicillin HELPS kill enterococci (Hemophilus Influenzae - pneumonia and accute meningitis, E. Coli - gastrointestinal infections, Listeria Monocytogenes - listeriosis, Proteus Mirabilis, Salmonella - thyphoid fever, salmonelesis,enterococci) |
|
|
What is the drug of choice in treating Bronchitis, Otitis Media and Sinusitis?
|
AmOxicillin - has greater oral availability than Amphicillin so it is frequently given to outpatients. Also drug of choice for infections caused by Listeria
|
|
|
What is the drug of choice for infections caused by Listeria?
|
AmOxicillin is the drug of choice! Listeria monocytogenes is a bacterium commonly found in soil, stream water, sewage, plants, and food. Gram-positive and rod-shaped. Responsible for listeriosis, a rare but potentially lethal food-borne infection.
|
|
|
What is the Amp-Gent combo and what is it used for?
|
AmOxicillin-gentomycin combo, used for treating serious urinary tract infections - used for broad gram negative coverage.
|
|
|
Nafcillin
|
Mechanism: same as Penicillin, but Penicillinase-Resistant because of bulkier R groups!
Toxicity: hypersensitivity reactions, methicillin - interstinal nephritis (no longer used in US) Niche: S. Aureus (except MRSA) Treat Staph with Naf! |
|
|
Piperacillin
|
Machanism: same as penicillin.
Antipseudomonal drug. Pseudomonas, which can cause devastating pneumonia and sepsis is so crafty and sneaky that we need James Bond's megaton pipe bomb to to help with its elimination. Toxicity: hypersensitivity reactions. Niche: Pseudomonias and gram negative rods. Piperacillin is susceptable to penicillinase - use with clavulanic acid. Most Stap Aureus are resistant to Piperacillin. |
|
|
Clavulanate
|

|
|
|
What is different about Cephalosporins?
|
Have two advantages over Penicillin:
1. the addition of a new basement makes the beta-lactam ring more resistant to beta-lactamases. 2. A new R-group side chain (another antenna cable TV) allows for broader spectrum. NOTE that MRSA and most ENTEROCOCCI (Including Strep Faecalis (E. faecalis causes many nosocomial infections such as endocarditis, bladder, prostate, and epididymal infections). Most are excreted in urine and some are metabolized by the liver. 3rd and 4th generations can cross blood-brain barrier. |
|
|
1st Generation Cephalosporins - Cefazolin
|
Cephazolin
Mechaism: beta-lactam drugs that inhibit cell wall synthesis but are less suseptible to penicillinases. Spectrum: gram positive cocci (including Staph Aureus and Strep Pneumoniae), as well as some gram negatives (Proteus Mirabilis, E. Coli, Klebsiella) Niche: Used as alternatives to Penicillin when it cannot be tolerated (allergy) - skin and bone infections, surgeons love to give it as profilaxis before surgery! |
|
|
What causes Community-Acquired Pneumonia (CAP)?
|
In infants: Listeria monocytogenes.
In adults: most common are Streptococcus pneumoniae and Hemophilus influenzae. Atypical bacteria that can cause it are Mycoplasma pneumoniae, Chlamydophilia pneumoniae and Legionella pneumophila. Since it takes few days to identify the exact agent in lab stdues (and often it cannot be identified) must use empirical therapy. In general, all therapies in older children and adults will include treatment for atypical bacteria. |
|
|
3rd generation of Cephalosporins - Ceftriaxone
|
Mechanism: same as all beta-lactams.
Spectrum: retain gram positive activity from 1st generation. Broad gram negative aerobic activity: used for serious gram negative rod infections that are resistant to other beta-lactam drugs - for treating community acquired pneumonia, meningitis and pyelonephritis (urinary tract infection that has gone to effect the kidneys) Ceftriaxone is the BEST for CSF penetration and is the BEST for treating Meningitis! |
|
|
3-1/2 generation of Cephalosporins - Ceftaizidime
|
Spectrum: resistant gram negative aerobic bacteria, but lost activity against gram plus.
The BEST for treating Pseudomonas - "Give Pseudomonas the TAZ!" |
|
|
Which Cephalosporin has the best CSF penetration?
|
Ceftriaxone - 3rd generation - used for treating all forms of meningitis in children and adults
|
|
|
Which drug/drugs is the best against Pseudomonas?
|
Ceftazidime, 3rd generation Cephalosporin - "Give Pseudomonas the TAZ!"
Cefepime - 4th generation Cephalosporine - good for broad range of nosocomial infections. |
|
|
4th generation Cephalosporins - Cefepime
|
Excellent activity against Pseudimonas and gram positive organisms
Niche: good for treating nosocomial infections. |
|
|
Carbopenems class - Meropenem
|
Meropenem is called "Decerebrate antibiotic" because you don't even have to think what bacteria it covers - it covers almots everything!
Toxicity: well tolerated Spectrum: Gram positive cocci, gram negative aeronic cocci (including Pseudomonas) plus anaerobs (enterococcus) Niche: nosocomial infections, febrile neutropenia, complicated intraabdominal infections. Alternative to 3rd and 4th generation Cephalosporins for CNS infections. |
|
|
Vancomycin
|
A glycopeptide - inhibits cell wall synthesis at the step earlier than beta-lactame drugs. It complexes with D-Ala-D-Ala to inhibit transpeptidation.
Given ONLY by IV. Spectrum: ALL GRAM POSITIVES! Including MRSA, Enterococcus Faecalis, Multi-Resistant Staph Epidermis. Can be used when allergic to beta-lactams, Also used to treat Endocarditis caused by Strep and Staph. (Remember Van+ being driven from an IV by an Indian (Red Man) and slamming into a wall of D-Ala peptidoglycan (p.190) Toxicity: infusion-related flushing (Red Man Syndrome), dose dependant ototoxicity and nephrotoxicity. |
|
|
Aminoglycosides - Gentamycin
|
Aminoglycosides - A Mean Guy
Mechanism: bactericidal - inhibit formation of initiation complex and cause misreading of mRNA. Require Oxygen for uptake, therefore ineffective against anaerobes. Used mainly against Gram Negative Rods. Synergistic with Beta-Lactam antibiotics (because penicillins can break down bacterial walls to facilitate diffusion). IV only! Toxicity: potentially severe and limits usefulness. Can cause CNVIII toxicity - vertigo and hearing loss. Renal toxicity Rare: complete neuromuscular blockage - curare-like effect. |
|
|
Tetracyclines - Doxycycline
|
Mechanism: inhibits 30S ribosomal subunit.
Spectrum: activbe against many gram positve and gram negative bacteria, mycoplasmas, chlamidiae and rikettsiaa (all the diseases you would expect a young soldier in a Tet Offensive to get): 1. Veneral diseases caused by Chlamydia Trachomatis 2. Walking pneumonia caused by Mycoplasma Pneumoniae (alternative to erythromycin) 3. Animal and tick-born diseases caused by Brucella and Rikettsia 4. severe acne Toxicity: 1. "Nervous souldier" - nausea,vomiting and diarrhea 2. "A blown up grenade" - phototoxic dermatitis 3. "Shrappnel strikes kidney and liver" kidney and liver toxicity. 4.Dark discolored teeth - doxycycline chelates Ca in the bones and teeth of babies under 7 - depressed bone growth and bown teeth. |
|
|
Macrolides - Azithromycin
|
Mechanism: inhibts 50S subunit. Bacteriostatic.
Spectrum: broad spectrum of activity against gram positive, some gram negative and atipicals such as Legionalla, Chlamydia and Mycoplasma (again, this is what you would expect a soldier from the French legion to get). Commonly used as a secod line agent against skin and soft tissue infections (not due to MRSA) as well as for upper respiratory infections. Toxicity: among the safest antibiotices out there. 1. Common and dose-dependant abdominal pain, resulting from increased intestinal peristalsis. 2. Rare cholestatic hepatistis ( imagine a wreath (from erythromycin) getting stuck inside the bile duct and blocking flow. 3. Rolonged QT syndrome. the drug of choice for Legionnaires disease |
|
|
What is drug of choice for Legionnaires disease?
|
Azithromycin (class of Macrolides). The heroic french legionnaire has died in a desert battle. In honor, a a wreath is laid on his grave placed on top of a tomb stone in the shape of a cross (Gram Positive organisms are mostly covered, but Legionella Pneumoniae is gram negative (odd ball)
|
|
|
Clindamycin
|
Mechanism: Blocks the peptide bond formation at 50S ribosomal subunit. Bacteriostatic.
Spectrum: many gram positive, NO gram negative and many anaerobes! Toxicity: assosiated with Clostridium Dificile Colitis. Spectrum: treats Clostridium Difficile infections. Surgeons use Clindamycin along with aminoglycosides for penetrating wound infections of teh abdomen. Also used in infections of femae genital tract (ex. septic abortions). Clindamycin can be given for months to patients with an anaerobic aspiration pneumonia. |
|
|
Oxazolidinones - Linezolid
|
Linezolid - Godzilla Lizard - newest antibiotic for stamping out gram positive resistant drugs.
Mechanism: inhibits 50S ribosomal subunit (can be either bacteriostatic or bactericidal). Can be intravenous or oral. Spectrum: ONLY Gram Pos. plus MRSA. Toxicity: dose-dependant thrombocytopenia. Very expensive. |
|
|
Sulfanamides - Trimethoprim, Sulfamethoxazole
|
Mechanism: inhibit bactrerial folic acid synthesis. Sylfonamides mimic PABA.
Trimethoprim resembles Folate - inhibits Dihydropholate Reductase. Synergistic and bactaricidal in combination. Can be oral or intravenous. Spectrum: broad against Gram Positive and Negative bacteria plus some protozoa. Clinical use: 1. Tree (Respiratory tree) - given in Pneumonia, otitis media, sinisitis, bronchitis 2. Mouth (Gastrointestinal tract) gram negatives that cause diarrhea like Shigella and Salmonella 3. Pee (Genitourinary tract) - urinary tract infections, prostatitis, urethritis 4. Syndrome (AIDS) - given as a prophilaxis covers Pneumocystis Carnii Pneumonia |
|
|
Fluoroquinolones: Ciprofloxacin
|
Mechanism: inhibit Topoisomerase II (DNA Gyrase) - inhibit DNA replication/bactericidal
Spectrum: Many Gram Negatives! 1. The multipe Resistant Pseudomonas Aeruginosa 2. Enterobacteriae 3. Complicated UTI's caused by Enterobacteriae, Pseudomonas etc 4. Gram Neg facultative intracellular organisms like Salmonella, Shigella and Brucella, Mycobacterium This is probably the BEST drug to use for Pseudomonas Aeruginosa. Toxicity: gastrointestinal, toxic to cartilage (don't give to children), QT prolongation and 'FluoroquiniLONES hurt attachments to your BONES |
|
|
Fluoroquinolones: Ciprofloxacin
|
Mechanism: inhibit Topoisomerase II (DNA Gyrase) - inhibit DNA replication/bactericidal
Spectrum: Many Gram Negatives! 1. The multipe Resistant Pseudomonas Aeruginosa 2. Enterobacteriae 3. Complicated UTI's caused by Enterobacteriae, Pseudomonas etc 4. Gram Neg facultative intracellular organisms like Salmonella, Shigella and Brucella, Mycobacterium This is probably the BEST drug to use for Pseudomonas Aeruginosa. Toxicity: gastrointestinal, toxic to cartilage (don't give to children), QT prolongation and 'FluoroquiniLONES hurt attachments to your BONES |

