![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
67 Cards in this Set
- Front
- Back
|
Pharmacology?
|
science dealing with the interactions between drugs and biological systems. pharmacologically speaking, a drug is a chemical substance that has an effect on a biological system.
|
|
|
Pharmacodynamics?
|
Study of the biological activity of a drug, including mechanisms of action and processes affected by it and structure-activity relationship.
|
|
|
Pharmacokinetics?
|
Study of how a drug enters the body, circulates within the body and leaves the body, and what factors influence its movements. has 4 major steps
|
|
|
4 majors steps of pharmacokinetics?
|
absorption, distribution, metabolism (biotransformation) and excretion.
|
|
|
pharmacotheraputics?
|
Deals with the proper selection and use of a drug for prevention, diagnosis and treatment of disease. It includes the consideration od indication, dosage, duration pf therapy, contraindications, drug-interactions and side effects.
|
|
elaborate.....
|
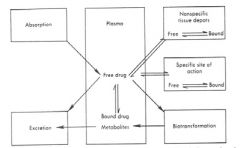
Absorption: accumulation of a drug in the body tissues.
3 areas of effect in the body- Plasma: mainly interacts with plasma proteins. Free drug: produces pharmacological action. Bound drug: metabolites 3 actions for free drug: non specific effects: AKA "side effects" does not produce the desired effects. specific site of sction: produces the desired effect, then pharmacokinetics takes place. biotransformation: metabolism. two phases. phase I: breaking down of the drug phase II: when the drug is combined with endogenous bodily molecules and a larger drug molecule is produced. drug metabolites are then excreted from the body. |
|
|
pharmacy?
|
a practice primarily dealing with the preparation and despensing of medicines,
|
|
|
toxicology?
|
Aspect of pharmacology involving poisons, their actions, their detection and treatment.
|
|
|
the two actions of drugs?
|
receptor mediated and non-receptor mediated
|
|
|
Receptor mediated drug action?
|
involves interactions between
drug and receptor; applies to most drugs |
|
|
Non-receptor mediated drug action:
|
involves physiochemical
interactions between drug and a biological system |
|
|
Receptors for drugs?
|
specialized target macromolecules present on cell surface or intracellularly that binds to a drug and mediates its pharmacologic actions
|
|
|
Drug receptor interaction?
|
For an agonist, this leads to the biologic response and the magnitude of the response is proportional to the number of drug-receptor complexes, according
to the occupation theory ( which follows the Law of Mass Action) Drug + Receptor <-> Drug–Receptor complex → Effect Drug that complexes/interacts with receptors may be classified as either agonist or antagonist drug and receptor have complementary structure and form some type of bond (covalent, hydrogen.....etc.) |
|
|
Agonist?
|
Has both affinity and intrinsic
activity/efficacy. (produces its own effect) can be either full or partial agonist. |
|
|
Antagonist?
|
Has affinity but not intrinsic activity.
- competitive, non-competitive (cannot produce its own effect) |
|
|
Competitive antagonist?
|
Interacts with the same receptor site as the agonist and competes with the agonist to block its action. This causes a parallel shift in the dose-response curve of the agonist to the right, without altering the maximum response.
|
|
|
non-competitive antagonist?
|
Either prevent the binding of the agonist to receptors OR somehow prevents the agonists from activating the receptors. It decreases the maximum response of the agonist.
|
|
|
partial agonist?
|
partially blocks the agonist's binding, causing less response than a full agonist.
|
|
|
Dose response quantitation:
|
When a drug exerts an effect on a biological system the effect can be
related quantitatively to the dose of the drug given. From this, a plot of dose-response curve or log dose response curve can be obtained. |
|
|
potency?
|
This is a measure of how much drug (dose) is required to elicit a given response or effect. It
can be shown by the location of its curve along the log-dose axis (X-axis). It is also termed effective dose concentration. The lower the dose required for a given response, the more potent the drug. It is most often represented as the dose that gives 50% of the maximum response, effective-dose 50 (ED50). A drug with a low ED50 is more potent then a drug with a larger ED50. The affinity (kd) of the receptor for a drug is an important factor in determining the potency. |
|
|
efficacy?
|
Is maximum response produced by a drug. It depends on the number of drug-receptor
complexes formed and the efficacy with which the activated receptor produces a cellular action. The efficacy of any drug is a major descriptive characteristic indicating its action |
|

elaborate
|
relationship between the amount of drug administered and the effect seen.
once the curve hits 100% intensity it is at its max dose. any dose administered above this will produce undesired side effects. |
|

explain? Dose response curves of 3 drugs showing potency and efficacy
|
the x axis shows the potency of the specific drug. the lower the dose needed to achieve the desired intensity of response the more potent the drug is.
efficacy is seen on the y-axis and shows the max amount of intensity that can be achieved with the specific drug. a drug that does not reach as high of an intensity response is said to have lower efficacy. |
|
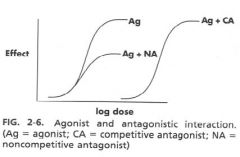
explain? Effects of competitive and Non-competitive antagonists.
|
with a competitive antagonist you have to have a higher dose in order to take over the competitive antagonist in the binding site of the receptor. this will lower the POTENCY of a drug
the non-competitive antagonist shuts down some of the binding affinity of the receptor OR does not allow action of the agonist. this lowers the effect that a drug will have. so this will lower the EFFICACY of the drug. |
|
|
Absorption?
|
Refers to transfer of a drug from the site of administration to the circulation. The process requires the drug passing through biologic membranes. Major factors influencing absorption: physiochemical factors, route of administration and solubility of the drug.
Drugs that are weak electrolytes dissociate in solution into a nonionized (uncharged) form and ionized (charged) form. Nonionized is lipid soluble and readily pass membrane. The ionized form is less lipid soluble. Thus the more ionized the compound, the less absorption that will occur and visa versa. The pH of the tissue at the site of administration and the dissociation characteristics (pka) of the drug will determine the amount of drug present in the ionized or unionized state. This amount will determine the ease with which the drug will penetrate or travel through tissue. The absorption of a drug from a solid dosage form administered orally (e.g. tablet) requires several steps: disruption, disintegration, dispersion, dissolution and absorption. Absorption from site of injection depends on the solubility of the drug and the blood flow at the site. If these factors are enhanced, absorption increases. |
|
|
Distribution?
|
The manner in which a drug is distributed in the body will determine how rapidly it produces a response, and the duration of that response. The distribution of a drug is determined by several factors such as the size of the organ, the blood flow, the solubility of the drug, plasma protein binding capacity and the presence of unique barriers (blood-brain barrier, placenta barrier).
Plasma site: - Drug in plasma can be free or bound to proteins (albumin and globulin). Biological action is related to the concentrations of free drug. Drugs are bound reversibly to plasma proteins and the bound drug is considered a non-active storage site. This can be displaced and released by another drug (eg., warfarin displaced by aspirin). This is important in drug-drug interactions. Tissue sites: - Nonspecific sites elicit either no response or undesirable effects, as opposed to specific sites. The process of distributing drugs to the tissues from plasma involves the passage of drugs across cell membranes. The biological half-life (t ½) of a drug is the time necessary for the body to eliminate half of the drug present in the circulation. It is an indication of the duration of drug action. The longer the half-life, the longer the action of the drug. Blood-brain barrier (BBB): - For a drug to have CNS effect should pass the BBB. Lipid-soluble drug easily penetrate the barrier and produces CNS effect. Placenta barrier: - Most drugs pass the placenta barrier. However, lipid soluble drugs penetrate more easily. Enterohepatic circulation/cycling: - Applies only to certain drugs with relatively high molecular weights. Redistribution of drugs:- Movement of drug from site of action to other nonspecific sites. This can affect the duration of action. |
|
|
Metabolism (biotransformation)?
|
Refers to the change of drugs by the body to be excreted. Most drugs are metabolized in the liver and the metabolic products are usually more polar and inactivee. This reduces renal tubular reabsorption of the drugs (kidney is major organ of excretion). Metabolites are less likely to bind to plasma or tissue proteins and less likely to be stored in fat tissue.
Drugs taken orally are absorbed from the GIT and pass directly into the liver. If susceptible, they are metabolized in the liver before they pass into the systemic circulation and this is known as the first-pass effect. This process decreases the amount of the active drug available to the systemic circulation.Metabolism of drugs may be divided into nonsynthetic (phase I) and synthetic (phase II) reactions. Phase I: Lipid molecules (less polar) are transformed/metabolized into polar molecules by oxidation, reduction and hydrolysis. Phase I reactions are mostly carried out by the microsomal or cytochrome P-450 enzymes (mixed function oxidase) in the liver. The cytochrome P-450 can be induced (e.g., by phenobarbital) or inhibited (eg., by cimetidine) by drugs. Phase II: Involves conjugation of drugs with endogenous substances such as glucuronic acid (glucuronidation), sulfuric acid, acetic acid or an amino acid. By this process molecules become bigger and more polar. This mechanism either alone or in combination with phase I reaction, allows the body to convert a lipid soluble drug to a more polar compound. This facilitates excretion. |
|
|
Excretion?
|
Renal excretion is the most important route of excretion. Others routes include the lungs, bile, GIT, sweat, saliva, gingival cervical fluid, and milk. While most drugs are excreted as metabolites (more polar), some drugs may be excreted unchanged. It is possible to promote or inhibit excretion of drugs using other drugs. Elimination of substances in the kidney can occur by three routes: glomerular filtration, active tubular secretion and passive tubular diffusion.
|
|
|
location of action on diuretics?
|
carbonic anhydrase inhibitors: proximal tubule
loop diuretics: loop thiazides: distal tubule K+ sparting diuretics: collecting duct |
|
|
Adverse reactions to drugs?
|
Every drug has more than one action, and the clinically desirable actions are termed therapeutic effects while the undesirable reactions are termed adverse effects which are potentially harmful. Often adverse effects are divided into the categories: toxic reaction, side effects, idiosyncratic reaction, drug allergy, interference with natural defense mechanisms, teratogenicity.
|
|
|
Toxicology Evaluation of drugs?
|
determination of lethal dose (LD50), ED(50) and theraputic index
|
|
|
Lethal Dose (LD50)?
|
Dose of a drug that kills 50% of the treated animals
|
|
|
Median effective dose (ED50)?
|
A dose required to produce a specified intensity of effect in 50% of the
animals. |
|
|
Therapeutic index (TI)?
|
Ratio of toxic dose to effective dose or LD50/ED50. It is the measure of the drug’s safety. If the value of the TI is small (narrow TI), then toxicity may be reached easily and visa
versa. A TI of greater than 10 is usually needed to produce a therapeutically useful drug. |
|
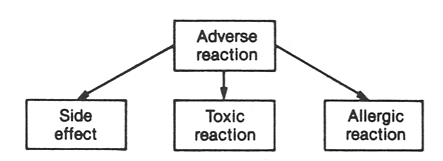
explain...
|
side effect:
predictable dose related acts on non target organs toxic reaction: predictable dose-related acts on target organs Allergic reaction: NOT predictable NOT dose related |
|

explain....?
|
large therapeutic index= safe
small therapeutic index= not safe TI of 10 or more= safe TI less than 10= not considered safe. TI= (LD50)/(ED50) |
|
|
Routes of drug administration?
|
Routes can affect both the onset and duration of response, and are broadly classified as enteral, parenteral and other routes.
Enteral (via GIT): Oral, sublingual, rectal Parenteral (by injection): Intravenous (IV), intramuscular (IM), subcutaneous (SC) Other routes: Inhalation, intranasal, intrathecal, topical, transdermal, etc. Many types of dosage forms are available but the most commonly used ones in dentistry are the tablet and capsule, which are administered by the oral route. |
|
|
Fate of drug?
|
Administered drug interacts with a membrane at various levels in order to reach its sites of action and
produce effects, and also to be acted upon by the body to be excreted. Membrane lipids make drug relatively impermeable/less permeable to ions and polar molecules. |
|
|
Major classes of cardiovascular medications?
|
cardiac glycosides, antiarrythmic agents, antianginal drugs, antihypertensive agents, antihyperlipidemics and anticoagulants.
|
|
|
common cardiovascular diseases?
|
Hypertension, angina pectoris, cerbrovascular accident (stroke) and
heart failure. CV disease is the leading cause of death in US and drugs used consist of more than 25% of the top 200 drugs. |
|
|
cardiac glycosides?
|
These are drugs mainly used for congestive heart failure (CHF).
ex: digoxin |
|
|
Digoxin (Lanoxin)?
|
Increases the force and efficiency of contraction of the myocardium allowing the heart to do more work without increased oxygen utilization.
Reduces edema that occurs in CHF. Slows AV conduction, prolongs refractory period of the AV node and decreases the rate of the SA node (useful in treating arrythmias). **more beneficial in treating patients with atrial fibrillation and CHF** has a narrow margin of safety. has many toxic effects including GI and CNS disturbances. had common drug interactions. |
|
|
Antiarrhythmic drugs?
|
Many of these drugs are used for a variety of CV diseases.
Ex: Quinidine and Lidocaine |
|
|
Quinidine?
|
Decreases myocardial excitability, conduction velocity and automatcity, and increases time of refractory period. (consequently depresses myocardium).
Used as a broad spectrum antiarrythmic effect and has atropinelike (anticholinergic) action. Clinically also used for treatment and prevention of supraventricular tachyarrhythmias and ventricular tachycardia. Oral doses of quinidine can cause nausea and vomiting. Large doses cause cinchonism. It also causes hypersensitivity reactions and hypotension. |
|
|
Lidocaine?
|
Common dental local anesthetic useful in the treatment of ventricular premature beats and tachycardia. Potent inhibitor of sodium channels and normalizes conduction velocity in ischemic tissues. Commonly employed in emergency situations (e.g., after cardiac surgery). Has short duration of action and given iv. Has several CNS and cardiac adverse effects.
|
|
|
Propanol?
|
Non-selective beta-blocker
Used primarily in sinus tachycardia, atrial flutter or fibrillation and digoxin induced arrhythmias. |
|
|
Calcium channel blockers?
|
Mainly used as antihypertensive
agents. Verapamil has significant cardiac effect making it more useful as an antiarrhythmic Has direct effect on SA node, decreasing heart rate. Produces a certain degree of hypotension and reflex tachycardia Particularly effective for superaventricular arrhythmias Major side effect is hypotension |
|
|
Antianginal drugs?
|
reduce the workload of the heart, thereby lowering the oxygen requirements of the myocardium, which in turn relieves the painful symptoms of angina.
Ex: nitrites/nitrates, Ca channel blockers and Beta-adrenergic blockers |
|
|
Organic nitrates and nitrites?
|
highly lipid soluble drugs used to terminate anginal attacks.
adverse effects: headache, postural hypotension and methemoglobin. Nitroglycerine is the most frequently used nitrate. It acts by relaxing the blood vessels. Nitroglycerine can be used sublingually for acute attack. Amyl nitrite is a volatile agent that can be used by inhalation to treat angina emergency situations. |
|
|
Beta-adrenergic blockers?
|
include propranolol, nadolol which are non-specific antagonists. act by blocking the beta-receptors to catecholamine stimulation, thereby reducing the heart activity and oxygen demand.
**particularly effective in reducing exercise and stress-induced anginal attacks. propanolol increases oxygen supply Adverse effects include bradycardia, CHF, headache, dry mouth, blurred vision and unpleasant dreams. |
|
|
Calcium channel blockers (antianginal use)?
|
includes verapamil, diltiazem and nifedipine.
inhibit calcium entry into cells during contraction. They can also be used in cardiac arrhythmias and hypertension. Adverse effects include dizziness, weakness, headache, flushing, nasal congestion, constipation and hypotension. Nifedipine has greatest vascular effect while verapamil has the greatest myocardial effect. Oral adverse effects include gingival enlargement (particularly with nifedipine), dysgeusia and some xerostomia |
|
|
Antihypertensive agents?
|
used to manage elevated BP in patients. pharmacological management involves a stepped-care approach.
step1: stop smoking, lose weight, exercise and behavioral modification step 2: diuretics, ACE inhibitors, CCB, B-adrenergic blockers. step3: increase dose, mix agents, vasodilators, step4: use 2-3 drugs, mix agents |
|
|
Diuretic agents?
|
consist of three major types: Thiazides and thiazide-like diuretics, the loop
diuretics and the potassium-sparing diuretics. Thiazide diuretics: Hydrochlorothiazide is the most commonly used thiazide. It is used for mild hypertension. These agents act mainly by inhibiting sodium reabsorption primarily in the distal convoluted tubule of the kidney. This leads to diuresis and reduction in fluid volume.Thiazides also cause increase in potassium excretion. Adverse effects include hypokalemia, hypercalcemia, anorexia, hyperuicemia, and hyperglycemia. loop diuretics: furosemide and bumetamide. These are high potency diuretics that can be used when rapid diuresis is required, or in emergency. They act primarily on ascending limb of Henle’s loop. These agents also inhibit the reabsorption of sodium with a concurrent loss of fluids, and produce hypokalemia and hyperuricemia. NSAIDS interfere with effect. Potassium-sparing diuretics: Spironolactone is aldosterone antagonist causing sodium excretion and loss of fluid. However, potassium is conserved by reabsorption in the distal tubule. Triamterene acts directly on the kidney tubule. The diuresis and potassium conservation that occurs resembles that of spironolactone. |
|
|
Adrenergic blocking drugs (antihypertensive agents)?
|
Beta adrenergic blockers: selective (atenolol and metoprolol) and non-selective (propanolol) beta blockers.(lower BP primarily by decreasing cardiac output and renin secretion). effects include lowering the plasma renin levels, a reduction in plasma
volume and venous return, a decrease in sympathetic outflow from the CNS and a reduction in peripheral resistance. Side effects: Exacerbation of asthma, bradycardia, peripheral vascular disease, CNS depression, impairment of insulin-induced hypoglycemia, and lipid profile. With sudden withdrawal, arrhythmia, severe angina and myocardial infarction. Alpha-adrenergic blockers: most common one is prazocin. It lowers b.p. by a peripheral blocking action on the alpha-1 receptor. It is often used in combination with thiazide diuretic. Common side effects include diziness, headache, weakness, and nausea. Dry mouth, orthostatic hypotension and fluid retention can also occur. lebetalol (alpha and beta blockers): Blocks beta-1, beta-2 and alpha receptors, reducing peripheral resistance. It also reduces plasma renin and aldesterone levels. |
|
|
Calcium channel blockers (antihypertensive drugs)?
|
Verapamil, nefedipine and diliazem
are also used in HT Act by decreasing the entry of calcium into cells and causing a reduction in peripheral resistance. |
|
|
ACE inhibitors (angiotensin converting enzyme)?
|
captopril, enalopril and lisinopril. Mechanism involves inhibition of the conversion of angiotensin I to angiotensin II. Angiotensin II acts to increase peripheral resistance by vasoconstriction and stimulates the release of aldosterone which also increases water retention. Side effects for these drugs include blood cell disorders, allergy, hypotension and loss of taste. Used especially in refractoryconditions either alone or in
combination with beta blockers, diuretics or calcium channel blockers |
|
|
Angiotensin II antagonists?
|
Bond to Ang II receptors and block the effect.
Ex: lasartan Has fewer side effects than ACEIs but NSAIDs may antagonize the antihypertensive effect. |
|
|
Clonidine (antihypertensive)?
|
Acts on postsynaptic alpha-1 receptors in vasomotor center, and on hypothalamic alpha-2 receptors in the CNS. CNS-acting antihypertensive. It acts primarily on the alpha-2 (a-2) receptors in the CNS to inhibit sympathetic outflow and reduce peripheral resistance. Adverse effects clonidine include sedation, dizziness and xerostomia.
|
|
|
Guanethidine?
|
Blocks norepinephrine (NE) release and depletes NE stores, resulting in reduced sympathetic neurotransmission and BP
Has delayed onset and prolonged duration of action decreases nonepinephrine release and sympathetic tone. It causes severe postural, impotency and exertional hypotension. Adverse effects include diarrhea, interference with ejaculation, and cardiac problems |
|
|
Reserpine?
|
Prevents NE from being stored in
sympathetic nerve ending, thus depleting stores. causes hypotension • Adverse effects include sedation, bad dreams, diarrhea, aggravation of peptic ulcer, and even psychotic depression that may lead to suicide |
|
|
Hydralazine?
|
Produces a more direct relaxation of
arterioles to reduce peripheral resistance Causes a rise in heart rate and output. Often used in combination with other antihypertensives Common side effects: cardiac arrhythmias, angina, headache and dizziness. |
|
|
Antihyperlipidemics?
|
directed primarily at lowering the levels of LDL cholesterol in patients
at risk for the complications of atheroselerosis. Ex: cholestyamine, niacin, HMG-Co-A-reductase inhibitors. |
|
|
HMG-Co-A reductase inhibitors?
|
Often referred to as “statins”
Act primarily by lowering cholesterol due to inhibition of HMG-Co-A reductase, rate limiting enzyme in cholesterol synthesis Examples: Atorvastatin (Lipitor)- most potent with long t1/2; another one is lovastatin |
|
|
Anticoagulants?
|
reduce blood clotting
Ex: heparin, warfarin and streptokinase. |
|
|
Heparin?
|
most commonly used anticoagulants. It is used in myocardial infarction or thrombophlebitis, among others. It is classified as a parenteral anticoagulant and, thus, is given by injection.
Common side effect is hemorrhage. Protamine sulfate is the antidote |
|
|
Warfarin?
|
aka "coumadin". Is an oral anticoagulant. It acts as vitamin K antimetabolite and is considered as an indirect acting anticoagulant. It has slow onset and prolonged effects. It is used in longterm
treatment of thromboembolic diseases such as thrombophlebitis and myocardial infarction. A common side effect associated with oral anticoagulants is hemorrhage. has a narrow theraputic index and also has common drug interactions. |
|
|
streptokinase and alteplase?
|
streptokinase:a clot-buster enzyme
alteplase: recombinant tissue type plasminogen activator. Also called thrombolytic drugs Promote conversion of plasminogen to plasmin, the natural clot resolving enzyme Usually administered by direct vessel perfusion to clot site Used primarily for deep vein thrombosis, pulmonary embolism, acute coronary artery thrombosis associated with myocardial infarction |

