![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
114 Cards in this Set
- Front
- Back
|
Classification of Muscle Relxants
|
1. Nondepolarizing
2. Depolarizing |
|
|
Nondepolarizing Muscle Relaxants
|
- Tubocurarine
- Atracurium - Rocuronium - Pancuronium |
|
|
Depolarizing Muscle Relaxants
|
Succinylcholine
|
|
|
Nondepolarizing Muscle relaxants
- Mechanism of Action - |
They are competitive blockers of nicotinic Ach receptors
2) Can enter ion channel so cholinesterase inhibitors (neostigmine) can antagonize them readily |
|
|
Depolarizing Muscle Relaxants
- Mechanism of Action - |
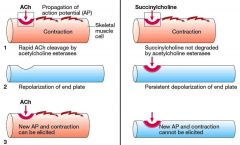
Works in two phases behaving like Ach, but with more of a prolonged action.
Phase I: prolonged depolariztion of muscle fibers. the Acetylcholinesterase inhibitors augment this phase. Phase II: the channel Desensitizes |
|
|
Clinical Application of Muscle relaxants
|
- Surgical Relaxation
- Control of ventilation - Treatment of Convulsions, however it has NO effect on the central processs involved in the convulsion. i.e. It doesnt affect the brain activity, just directly the movements associated with the spasms. |
|
|
Tubocurarine
|
- Nondepolarizing Muscle relaxant
- First it affects the Face, Foot, and Hand - Secondly the Abdomen and Trunk - Finally the Diaphragm. - Recovery occurs in the reverse order. |
|
|
Succinylcholine
|
- Depolarizing Muscle Relaxant
- First affects the Arms, Neck, and Legs - Secondly affects the respiratory Muscles within 60 sec - Finally the Face and pharynx - Recovery occurs in the reverse order. |
|
|
Adverse effects of Depolarizing Drugs
|
- Hyperkalemia. Patients with burns, nerve damage or neuromuscular disease, closed head injury and other trauma. the Problem is that it can result in CARDIAC ARREST.
- Increased Intragastric pressure. This is seen frequently in heavily muscled patients. - Muscle Pain. Also associated with "beefy" individuals. |
|
|
Splasmolytic drugs
|
- Diazepam
- Baclofen ( acts on GABA b receptors - Tizanidine , is a congener of clonidine - Dantrolene, Reduces skeletal muscle strength by interfering with the excitation-coupling reaction. Interferes with the release of Ca2+ through the sarcoplasmic reticulum. It's used in Malignant hyperthermia - Botulinum Toxin - Methocarbamol Robaxin |
|
|
General Anaesthetics
|
They are drugs which produce reversible loss of all sensation and consciousness.
Usually achieved through a combination of inhaled and I.V. drugs The Cardinal features are : - Loss of sensation - Sleep(unconsciousness) and amnesia - immobility and muscle relaxation - Abolition of somatic and autonomic reflexes |
|
|
Difference between local and General Anesthetics
|
General Anesthetics have a reversible loss of consciousness and loss of CNS activity - whereas; in Local Anesthetics- there is No loss of Consciousness and the Loss of Pain sensation is Reversible.
|
|
|
Inhalational Anesthetics
|
- Gaseous - N2O(Nitrous Oxide), and Cyclopropane
- Volatile anesthetics 1. Halogenated 2. Non Halogenated - Halothane - Ether - Enflurane - Chloroform - Isoflurane - Methoxyflurane - Sevoflurane - Desflurane |
|
|
Intravenous Anesthetics
|
- I.V. anesthetics have an onset of action faster than the fastest gaseous agent so they are used for induction of Anesthesia.
- Consist of : - Barbituates ( thiopental, methohexital) - Propofol - Etomidate - Ketamine ** |
|
|
Local Anesthetics
|
there are Esters and Amides. A way to remember it is that Ester's have only 1 letter "i" and the amides have two letter "i" 's.
|
|
|
Local Anesthetics
Esters |
1. Cocaine
2. Procaine 3. Chloroprocaine 4. Tetracaine |
|
|
Local Anesthetics
Amides |
1. Lidocaine
2. Bupivaciane 3. Mepivacaine 4. Dibucaine 5. Prilocaine 6. Etidocaine |
|
|
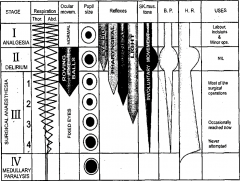
Stages of General Anestheisa
|
stage 1- Analgesia
stage 2 - Excitement/ Delirium stage 3 - Surgical Anesthesia ~plane I : regular breathing but loss of eye movement. ~Plane II : initiation of IC muscle paralysis ~Plane III : completion of ICM paralysis ~Plane IV : diaphragmatic paralysis - Stage 4 : Medullary Paralysis |
|
|
Stages of Anaesthesia
|
|
|
|
Ketamine
|
Ketamine Does not affect GABA-a, it antagonizes glutamic acid on NMDA receptors.
- Inhaled anesthetics also cause membrane hyperpolarization via activation of potassium channels. - Ketamine produces dissociative anesthesia, characterized by: catatonia amnesia, and analgesia, with or without loss of consciousness. - It is the only intravenous anesthetic that posses analgesic properties and produces cardiovascular stimulation. - Ketamine markedly increases cerebral blood flow and intracranial pressure. - Ketamine may produce postoperative sensory and perceptual illusions, disorientation and vivid dreams (emergence phenomena). - It is considered useful for poor-risk geriatric patients and in cardiogenic or septic shock. - It is also used in children undergoing painful procedures (eg, dressing changes for burns). |
|
|
Nitrous Oxide
|
- colorless inorganic, non-irritating
- sweet tasting. - Non-flammable - known as laughing gas. - Rapid induction and rapid recovery, and does not induce post-operative nausea and vomiting. However, it is not a potent anesthetic. - Ir requires pre-anesthetic medication, and can cause hypoxia. |
|
|
General Anesthetic's PHARMACOKENETICS
|
- Adds to the partial pressure in the brain, raising the tension in the tissue for induction and recovery.
- the principle objective is to achieve a constant and optimal brain partial pressure of the inhaled anesthetic. |
|
|
MAC
|
Minimum Alveolar anesthetic Concentration
- In a steady state, the partial pressure of an inhaled anestehtic in the brain equals that in the lung. - MAC is the concentration that results in immobility of 50% of patients when exposed to a noxious stimulant. |
|
|
Hepatotoxicity
|
due to halothane is 1/35,000. Obese peopel having several exposures to halothane are more susceptable
|
|
|
Malignant Hyperthermia
|
- an autosomal dominant genetic disorder of skeletal muscle that occurs by inhaled agents and muscle relaxants ( succinylcholine)
- consists of : rapid onset of tachycardia, hypertension, severe muscle rigidity, hyperthermia, hyperkalemia and acidosis. - Treatment consists of correction of metabolic distrubances and administration of Dantrolene |
|
|
Atropine
|
Atropine counters the "rest and digest" activity of glands regulated by the parasympathetic nervous system. This occurs because atropine is a competitive antagonist of the muscarinic acetylcholine receptors (acetylcholine being the main neurotransmitter used by the parasympathetic nervous system). Atropine dilates the pupils, increases heart rate, and reduces salivation and other secretions.
|
|
|
Serotonin Syndrome
|
Serotonin syndrome is a potentially life-threatening drug reaction that may occur following therapeutic drug use, inadvertent interactions between drugs, overdose of particular drugs, or the recreational use of certain drugs.
The excess serotonin activity produces a spectrum of specific symptoms including cognitive, autonomic, and somatic effects. The symptoms may range from barely perceptible to fatal. |
|
|
Ebstein's Anomoly
|
Ebstein anomaly is a congenital heart defect in which the septal leaflet of the tricuspid valve is displaced towards the apex of the right ventricle of the heart.
-Ebstein's cardiophysiology typically presents as an (antidromic) AV reentrant tachycardia with associated pre-excitation. In this setting, the preferred pharmacological treatment agent is procainamide. Since AV-blockade may promote conduction over the accessory pathway, drugs like beta blockers, calcium channel blockers and digoxin are contraindicated |
|
|
Thiopental
|
- can produce a state of hypnosis (loss of consciousness) in one circulation time
- Because of its rapid removal from brain tissue a single dose of thiopental is so short acting. - Large doses of thiopental decreases blood pressure and cardiac output and depresses respiration. - Cerebral blood flow is decreased. (A desirable drug for patients with head trauma or brain tumors). DECREASES INTERCRANIAL PRESSURE* THE ONLY ONE THAT DOES. |
|
|
Propofol
|
- It's onset of action is similar to thiopental but recovery is more rapid (similar to the shortest-acting inhaled anesthetics)
- Post-operative nausea and vomiting is less common because of propofol has antiemetic actions - Because of strong negative inotropic effects, propofol causes marked decrease in blood pressure and is a respiratory depressant. |
|
|
Ethomidate
|
- Causes Minimal Cardiovascular and respiratory depression.
- Produces a rapid loss of consciousness and rapid recovery (< 5 minutes). - Etomidate causes a high incidence of pain on injection, myocolonus, and postoperative nausea and vomiting. - Etomidate may cause adrenocortical suppression and decrease in hydrocortisone after a single dose. |
|
|
Adjuvant Drugs
|
Remifentanil (opioid) has an extremely short duration of action
Fentanyl and droperidol together produce analgesia and amnesia and are used with nitrous oxide. Midazolam is frequently given intravenously before induction of general anesthesia because it causes amnesia (> 50%) |
|
|
Narcotic
|
an imprecise term suggesting a state of narcosis - indicating a somnolent state
|
|
|
Opioid analgesic
|
analgesia (pain absence) without resulting in loss of consciousness/sleep
|
|
|
Opioids
|
all natural and semisynthetic opium alkaloid derivatives.
are blocked by naloxone- nonselective opioid receptor antagonist |
|
|
Opioid Constituents
|
- Morphine
- Codeine - Thebaine : nonanalgesic - Papaverine : nonanalgesic, vasodilator |
|
|
History of Opioids
|
- Comes from the greek God Morpheus : the god of Dreams.
- They act on Endorphin receptors that are assocaited with the sense of pleasure. (Mu- most important and Kappa) - derived from poppy seeds, they have been used for thousands of years to produce : Euphoria, Analgesia, Sedation, RELIEF FROM DIARRHEA, and Cough suppression. |
|
|
Opioid receptors
|
- Mu (1 and 2)
- sedation, cough suppressant, Nausea and Vomiting - increase Histamine - Kappa ( k1 and K3) - Only modest analgesia - little or no RESPIRATORY DEPRESSION - Dysphoric effects - Delta - unclear what its responsible for - May regulate Mu receptor |
|
|
Pure Agonist
|
Has affinity for binding plus efficacy
|
|
|
Partial Agonist
|
- Has affinity for binding but low efficacy.
- * in the absence of an pure agonist, the partial agonist will act as an Antagonist |
|
|
Pure Antagonist
|
Has affinity for binding but no efficacy; blocks action of endogenous and exogenous ligands
|
|
|
Mixed Agonist- Antagoist
|
- Produces an agonist effect at one receptor and an antagonist effect at another.
|
|
|
Pure agonist Examples
|
- Remember are agnostic on both Mu and Kappa receptors.
- Morphine - Codeine - Meperidine - Fentanyl - Remifentanil - Propoxyphene - Hydrocodone - Oxycodone |
|
|
Agonist-Antagonist examples
|
- * are Antagonists on Mu receptors
- * are Agonists on Kappa receptors - Nalbuphine - butorphanol - Buprenorphine |
|
|
Pure Antagonists Examples
|
- * Antagonists on both receptors
- Naloxone *** - Naltrexone *** |
|
|
Partial Agonist Examples
|
- Partial Agonist / Weak Antagonist on Mu receptors
- Agonist on Kappa - * Pentazocine |
|
|
Opioid Mechanism of Action
|

|
|
|
Opioid Pharmacological Actions
|
1. Euphoria
- Anxiolytic; plesant; floating sensation - individuals not in pain may experience dysphoria 2. Sedation -given as monotherapy, opioids produce sleep from which individuals can be easily awakened. - used in combination with sedative-hypnotics to induce very deep sleep. 3. Analgesia: Pain Components - CNS effects( mu 1 & 2 receptor mediated) for analgesia, sedation, euphoria, respiratory depression. - Affective emotionally - And Sensory |
|
|
Opioid Respiratory Depression
|
- inhibit's brian stem respiratory centers
- Respiratory depression is dose-related influenced by extent to sensory input - more needed for patients with opioid addiction - poorly or not tolerated in patients with respiratory problems ( Can cause death) with: - Asthma. - Chronic obstructive pulmonary disease (COPD). - Cor Pulmonale. - Increased interracial pressure. |
|
|
Opioid Cough suppression
|
- Opioids suppress the "cough center" in the brain
- Most effective is codeine - Management of pathologic cough - Management of patients with endotracheal tubes associcated with; Secretion accumulation- leading to atelectasis; airway obstruction. |
|
|
Opioid Miosis
|
- Pupillary constriction: commonly seen with opioid agonists
- Blocked by opioid antagonists - No development of tolerance - Mechanism : Edinger-Westphal nucleus of the oculomotor nuerve. Parasympathetic system may be blocked by atropine. |
|
|
Opioid Truncal rigidity
|
- Increased Large trunk muscle tone: Supraspinal action
- Most often seen with highly lipophilic Opioids, upon rapid IV administration (fentanyl, sufentanil, etc) - Revesal of truncal rigidity done by opioid antagonists - Maintenance of analgesia with reduced tuncal rigidity needs concurrent neuromuscular blocking drug use. |
|
|
Opioid Nausea and Vomiting
|
- Opioid analgesic: stimulate brain stem chemoreceptor trigger zone (CTZ)
- Vestibular component may also be present |
|
|
Acute Opioid Toxicity
|
- May result from clinical overdosage, accidental overdosage in addicts, or attempts at suicide.
- Occasionally, a delayed type of toxicity may occur from the injection of an opioid into the chilled skin areaas or in patients with low blood pressure and shock. - Symptoms and Diagnosis: the tirad of coma, pinpoint pupils, and depressed respiration strongly suggests opioid poisoning. |
|
|
Methadone
(Phenylheptylamines) |
- similar to morphine but longer acting
- reliable following oral administration - Compared to morphine, methadone tolerance and physical dependence develops more slowly. - Following abrupt methadone discontinuation withdrawl symptoms less severe than with morphine. - Useful drugs detoxification in maintenance of chronic, heroin addict. - Cross-tolerance with heroin (methadone prevents addiction-reinforcing heroin actions) |
|
|
Phenylpiperidines
|
- Meperidine
- Fentanyl group - Diphenoxylate - Loperamide |
|
|
Opioid agonist-antagonist
|
- Pentazocine
- Nalbuphine - Buprenorphine - Butorphanol |
|
|
Meperidine
|
- Significant anticholinergic (antimuscarinic) effects
- Contraindicated in the presence of underlying tachycardia - May have a negative ionotropic cardiac effect - Risk of seizures: due to accumulation of CNS active metabolite, normeperidine |
|
|
Fentanyl group
|
Fentanyl, sufentanil, alfentanil, remifentanil
- Sufentanil : 5-7 times more potent than fentanyl - Alfentanil less potent than fentanyl, more rapid acting and shorter duration of action - remifentanil: rapidly metabolized: tussue cholinesterases resulting in an extremely short half-life |
|
|
Diphenoxylate
|
metabolite (difenoxin)
- In management of diarrhea used in combination with atropine - Limited abuse potential |
|
|
Loperamide
|
- Management of diarrhea
- Limited abuse potential |
|
|
Pentazocine
|
- common: sedation + analgesia in therapeutic doses
- sweating, dizziness, Nausea : Common at higher doses - Respiratory Depression: significant respiratory depression less likely than with pure opioid agonist; reversible by naloxone. - Agonist antagonists(nalorphine) less likely to be effective in reversing respiratory depression. - Psychotomimetic effects: agonist-antagonists - Nightmares, Anxiety, Hallucinations |
|
|
Nalbuphine
|
- Kappa(k) agonist; Mu antagonist
- Parenteral administration - Possibly less respiratory depression than with morphine - When respiratory depression occurs: may be more difficult to reverse with naloxone. |
|
|
Buprenorphine
|
- Long acting, potent, partial Mu agonist
- Slowed dissociation form receptor hence relative naloxone-reversal resistant |
|
|
Butorphanol
|
- Analgesic equivalent to Buprenorphine and Nalbuphine, more sedation.
- Kappa (k) agonist |
|
|
Pharmacokinetics
|
- How a drug comes and goes
- Over the course of time how a drug is Absorbed, Distributed, Metabolized, and Excreted |
|
|
Liberation
|
- applies to drugs given orally
- where the drug is released from a pill, tablet, or capsule to dissolve at a different part of the GI system. |
|
|
Absorption
|
Movement from administration site into the circulation
|
|
|
Membranes and Absorption
|
- Only small uncharged particles can pass through the lipid bilayer. Thus, for a drug to be active it has to be uncharged to be lipid soluble.
|
|
|
Le Chatlier's Principle
|
- If a chemical system at equilibrium experiences a change in concentration, temperature, volume or partial pressure, then the equilibrium shifts to counteract the imposed change and a new equilibrium is established.
- A system will try to reach Equilibrium |
|
|
Environmental pH and Ionization
|
- Acidic drugs are best absorbed from Acidic Environments( because they will be uncharged). So, to increase absorption of an acidic drug, you acidify the environment. Or to decrease its absorption you can alkalize/ make more basic the environment
- Basic Drugs are best absorbed from basic environments (Because they will be uncharged). And likewise to acidic drugs. |
|
|
Bioavailability
|
the fraction of a drug absorbed into the systemic circulation.
|
|
|
First pass Effect
|
- that a drug ingested into the GI system will be absorbed in the intestines and then transported to the liver for metabolism. Then it passes into systemic circulation.
|
|
|
Protein binding
|
if a drug is bound to a protein than it is inactive, if its is free then it is capable of being active.
- competition between drugs = increases free portion of drug. |
|
|
Phases of drug metabolism (Bio-transformation)
|
- Biotransformation is the actual metabolism of a drug molecularly.
- Phase I ; consists of Oxidation/ Reduction/ Hydrolysis -Phase II ; conjugation |
|
|
Biotransformation
|

|
|
|
General Inducers
|
- Quinidine
- Barbiturates - St.Johns Wart - Phenytoin - Rifampin - Griseofulvin - Carbamazepine - Chronic alcoholism Queen Barb St.ole Phenand Refuses Greasy Carbs. |
|
|
General Inhibitors
|
- Sulfonamides
- isoniazid - Cimetidine - Erythromycin - Grape fruit juice - Acute alcohol intox - Ritonavir - Trimethoprim - SSRI's. Amiodarone |
|
|
Cytochrome- 450
3A4 |
- Biotransformation
- 60% of all drugs |
|
|
Zero Order Elimination
|
- A constant amount of drug is excreted per unit time
- rate of elimination is independent of plasma concentration. - No fixed halflife, its variable - examples are Alcohol, and phenytoin |
|
|
First Order Elimination
|
A constant fraction of the drug is eliminated per unit time.
- rate of elimination is directly proportional to the plasma level, - the half-life is constant - The rate of elimination is variable |
|
|
Renal Elimination
|
- rate of elimination = GFR + active secretion - reabsorption.
- CLearance (Cl) : the volume of blood cleared of drug per unit time - It is constant 1st order kinetics - Cl = GFR if there is no reabsorption, excretion and protein binding. - For protein bound drug, Cl= free fraction* GFR |
|
|
Plateau Principle
|
- Although it takes 7 half lives mathematically to reach a steady state; for clinical steady state is 4-5 half lives.
|
|
|
Rate of Infusion
|
- Rate of infusion (k0) does determine plasma level at steady state. If rate of infusion doubled, then the plasma level of drug at steady state is doubled.
- But time required to achieve steady state still remains the same. |
|
|
Antidepressants
|
four categories
1. MAO inhibitors 2. Tricyclic antidepressants (TCAs) 3. SSRI's 4. Atypical Antidepressants |
|
|
The monamine theory
|
Basically that depression is caused by a deficiency of NA or 5HT or both in the post synaptic region. And that in depressed individuals have more Monoamine oxidase enzymes, which cause the degradation leading to that deficiency.
|
|
|
MAO inhibitors
|
~MAO-A: Peripheral nerve endings, Intestine and Placenta (5-HT and NA)
~MAO-B: Brain and in Platelets and Mainly Serotonergic (Phenylalanine) ~Selective MAO-A inhibitors (RIMA) have antidepressant property Major drawbacks: Manic state or hypertensive crisis Cheese reactions Other drug interactions |
|
|
Tricyclic Antidepressants
|
TCA's
NA, 5 HT and Dopamine are present in Nerve endings Normally, there are reuptake mechanism and termination of action TCAs inhibit reuptake and make more monoamines available for action |
|
|
SSRI's
|
Serotonins also reuptaken by Nerve terminals
SSRIs inhibit the reuptake mechanism and make more 5 HT available for action |
|
|
MAO inhibitor examples
|
Irreversible:
Isocarboxazid, Iproniazid, Phenelzine and Tranylcypromine Reversible: Moclobemide and Clorgyline |
|
|
Hypertensive Crisis
|
caused by NE releasers: Tyramine ( Cheese, Red Wine), Cold Meds (Ephedrin), Amphetamines.
- TCAs - Alpha 1 agonists - Leva dopa |
|
|
TCA examples
|
NA and 5 HT reuptake inhibitors – Imipramine, Amitryptiline, Doxepin, Dothiepin and Clomipramine
NA reuptake inhibitors – Desimipramine, Nortryptyline, Amoxapine |
|
|
Imipramine
|
- Inhibit NE Transporter and SERT
- Interacts with variety of receptors – alpha, H1, 5HT1, 5HT2 and D2 - Sedation, and no other CNS effects - elevated mood after 2-4 weeks ***ANS: Dry mouth, blurring of vision, constipation and urinary hesitancy CVS: Tachycardia – NA and anticholinergic action Postural hypotension ECG – T wave suppression Arrhythmia |
|
|
SSRI examples
|
Fluoxetine, Fluvoxamine, Sertraline and Citalopram
- No seadation, so no cognitive or psychomotor function interference. - Interferes with ejaculation - Serotonin Syndrome: Mental confusion, hallucinations, sweating, hyperthermia, twitching of muscle, clonus and convulsion. |
|
|
Fluoxetine
|
SSRI
- Prototype of SSRIs - Slow action and not used for rapid effects - Longest acting – 2 days, t1/2 = 2 days - Used in depression and OCDs in adult and children |
|
|
Atypical Antidepressant examples
|
1. Trazodone
2. Venlafaxine 3. Mitazapine 4. Bupropion |
|
|
Bupropion
|
Inhibitor of DA and NA uptake (NDRI)
Non-sedative but excitant property Used in depression and cessation of smoking Seizure may precipitated |
|
|
Mitrazapine
|
NaSSA action (Noradrenaergic and specific serotonergic antidepressant) – enhancement of NA release and specific 5-HT1 receptor action
Blockade of 5-HT2 and 5-HT3 No anticholinergic or antidopaminergic action Alpha 2 antagonist. |
|
|
Trazodone
|
Weak 5-HT uptake block, α – block, 5-HT2 antagonist
No anticholinergic action No arrhythmia No seizure ADRs: Priapism, Postural Hypotension |
|
|
Venlafaxine
|
SNRI (Serotonin and NA uptake inhibitor)
Fast in action No cholinergic, adrenergic and histaminic interference Raising of BP |
|
|
Amantadine
|
An antiviral drug, moderately effective
Mechanism – unclear ; affecting D release and uptake, anti cholinergic. Used in early stages of parkinsons as a adjutant Antagonism at NMDA receptors might be involved |
|
|
Partial seizure
|
- consciousness preserved; manifested variously as convulsive jerking, paresthesias, psychic symptoms and autonomic dysfunction.
- Carbamazepines are used |
|
|
Tonic-clonic Seizrues
|
1. Phenytoin
2. Carbmazepine 3. Valproate |
|
|
Absence seizures
|
Impaired consciousness (often abrupt onset and brief), sometimes with automatisms, loss of postural tone, or enuresis; begin in childhood (formerly, petit mal) and usually cease by age 20 years
--> Ethosuximide |
|
|
Myoclonic seizures
|
single or multiple myoclonic muscle jerks
--> Valproate |
|
|
Status epilepticus
|
A series of seizures (usually tonic clonic) without recovery of consciousness between attacks, it is a life threatening emergency
|
|
|
Phenytoin
|
- Antiepileptic
- The oral bioavailability of phenytoin is variable because of differences in first-pass metabolism. - Phenytoin metabolism is non linear; elimination kinetics shift from first-order to zero-order at moderate to high dose levels. - Variable absorption |
|
|
Valproic Acid
|
- epilepsy and bipolar treatment
- anticonvulsant and mood stabalizer |
|
|
Na channel blockade
|
At therapeutic concentrations, phenytoin, carbamazepine,and Lamotrigine block voltage-gated sodium channels in neuronal membranes. Blocks Na+ channels in inactivated state.
This action is rate-dependent (ie, dependent on the frequency of neuronal discharge) and results in prolongation of the inactivated state of the Na+ channel and the refractory period of the neuron. Hence prevents propogation. Phenobarbital and valproic acid may exert similar effects at high doses. |
|
|
GABA-related drugs
|
Benzodiazepines interact with specific receptors on the GABAA receptor-chloride ion channel macromolecular complex.
In the presence of benzodiazepines, the frequency of chloride ion channel opening is increased; these drugs facilitate the inhibitory effects of GABA. Phenobarbital and other barbiturates also enhance the inhibitory actions of GABA but interact with a different receptor site on chloride ion channels that results in an increased duration of chloride ion channel opening |
|
|
Calcium channel blockade
|
Ethosuximide inhibits low-threshold (T-type) Ca2+ currents, especially in thalamic neurons that act as pacemakers to generate rhythmic cortical discharge.
A similar action is reported for valproic acid. |
|
|
Flumazenil
|
Non specific BDZ receptor antagonist
Used to treat CNS depression caused byBZ overdose. Can not reverse CNS depression caused by Barbiturates or alcohol. |
|
|
Buspirone
|
5-HT-1A mixed agonist-antagonist, weak DA block
Not a benzo, not hypnotic, no tolerance, no dependance, no withdrawal Anxiolytic, Used for GAD Non sedative Takes 1-2 weeks for effects No anticonvulsant activity, will not protect from withdrawal symptoms |
|
|
Antipsychotics
|
4 major groups
1. phenothiazines 2. THoxanthenes 3, Butyrophenones (haolperidol) 4. Heterocyclic AP |

