![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
78 Cards in this Set
- Front
- Back
|
Papaverine (source and use) |
Opium extract, vasodilator and GI muscle relaxant (colics) |
|
|
Digoxin (source and use) |
Foxglove extract, increases cardiac contractility (manage heart failure) |
|
|
Atropine source and class |
Atropa belladona, cholinergic muscarinic antagonist |
|
|
Lovastatin and Simvastatin source and use |
Asperigillus terreus, lowers cholesterol |
|
|
Cyclosporine use |
Immunosuppressant |
|
|
to filter through normal renal capillaries, how small must the object be? |
below 59-69 kDa. Albumin is around 67,000 Da, should not cross in healthy individuals |
|
|
To undergo passive diffusion (water soluble) through aquaporins, how small must the object be? |
Under 150-200 Da, or less than 8-10 A (0.8-1nm). Note connexins are like two aquaporins |
|
|
Which allows more passage of liposoluble products- stomach or intestine? |
Stomach. Intestine is lined with hydrophilic sugars |
|
|
In the stomach milieu, are acidic drugs or basic drugs more easily absorbed into blood stream? |
Acidic drugs, like COO- which are protonated in stomach acid to COOH and are now neutral and lipid soluble |
|
|
In the intestinal milieu, are acidic drugs or basic drugs more easily absorbed into blood stream? |
Basic drugs, which are non protonated/neutral |
|
|
pKa = |
pH at which 50% of ionization occurs |
|
|
T/F: Protein-bound drug fraction depends on the concentration of drug |
F |
|
|
T/F Acidic and neutral drugs bind to albumin or lipoproteins |
T |
|
|
T/F Basic drugs bind to Alpha-1 acidic glycoprotein |
T |
|
|
Intravascular body water percentage |
4% |
|
|
Most body water found in... |
intracellular water (40-44%) |
|
|
Extracellular water made up of... |
Intravascular (4%) and Interstitial (12-16%) |
|
|
What is volume of distribution? |
Mass (amount of drug / concentration drug in plasma) |
|
|
High Vd indicates.... |
highly distributed to tissues. Thus, higher lipid solubility, lower rates of ionization, or low plasma binding |
|
|
Assumptions made in apparent Vd |
Assumes drug distributed uniformly throughout body, distributed uniformly in a single compartment, concentration in plasma is representative |
|
|
Drugs that reach the brain have a high or low Vd? |
High |
|
|
Clearance = |
Biotransformation + Excretion |
|
|
Phase 1 drug biotransformation |
Usually transforms drug into polar metabolite (water soluble). Unmasks functional group through oxidation/reduction/hydrolysis. Inserts OH. The enzymes that regulate this are CYP450 family. Substrate specific. Metabolites usually inactive, but sometimes active or even toxic! CYP3A4/5 most abundant- takes care of 50% of drugs. |
|
|
CYP2D6 metabolizes what? |
Codeine, Fluoxetine. Codeine is transformed in the body into morphine (10%). Codeine is a prodrug. St. John's Wort is an inducer of 2D6, which means more codeine will be transformed to morphine. |
|
|
CYP2E1 metabolizes what? |
Ethanol, acetaminophen. Ethanol is also an inducer of 2E1, which can result in more Acetaminophen being broken down and releasing metabolite NAPQI (toxic). |
|
|
What biotransformation process does alcohol deplete |
Alcohol depletes glucoronidation and sulfation (Phase II). This shunts acetaminophen into Phase II, which produces NAPQI! PLUS, alcohol inhibits gluthione, which neutralizes NAPQI. |
|
|
Infants have higher/lower body water |
Higher body water. Less lipophilic drug in in fatty tissue. |
|
|
Liver metabolism of drug capability highest in what age group |
Young adults |
|
|
Renal drug elimination capability highest in what age group |
Young adults |
|
|
How is clearance measured |
Volume of body fluid from which compound is removed, per unit of time (mL/min) |
|
|
What do we use to measure GFR? |
Measure creatinine (small) in urine or blood. 6000 Da. Eliminated very easily. Should be same in urine as in blood. |
|
|
What drugs are eliminated by tubular secretion? |
Penicillin, PAH. Higher in urine than in blood. |
|
|
What compound is reabsorbed in the tubules? |
Glucose. Should be lower in urine than in blood. |
|
|
IV sodium bicarb (alkalize urine) will help eliminate what kind of drugs? |
Acidic drugs, like herbicides, fluoride, phenobarbital, salicylates. DECREASES their half life |
|
|
Ammonium chloride accelerates elimination of what drugs? |
Weak basic drugs- amphetamine, morphine, propanolol, atropine |
|
|
Zero order kinetics, rate of elimination is saturable/not saturable |
saturable. Prototypical example- alcohol |
|
|
T/F. Most drugs fall into first order kinetics |
True, because given at low doses |
|
|
Drug half life usually follows what order kinetics? |
First order, and drugs decreases exponentially over time |
|
|
What is an allosteric activator (noncompetitive activator)? |
Drug that doesn't do anything by itself, but potentiates agonist effect. Binds to other site on receptor. |
|
|
What is an allosteric inhibitor (noncompetitive inhibitor)? |
Drug that doesn't do anything by itself, but decreases the agonist effect. Binds to other site on receptor. |
|
|
Benzodiazepines (Diazepam, Valium) and barbiturates (Phenobarbital) are non competitive agonists (allosteric activators) where? |
At GABA-A receptors. Increase GABA activity. GABA slows down neurons. |
|
|
Memantine (Ebixa) is an allosteric inhibitor at what site? |
Glutamate NMDA receptors. Inhibits glutamate's excitatory effect, so prescribed to prevent epilepsy, in dementia. Binds to a different site on the NMDA receptor than glutamate does. |
|
|
Opening of ion channels does what to the cell? |
Depolarize it (ion go from high concentration to low concentration) |
|
|
How many subunits does ion channel have? |
2 alpha and 2 beta units (4). Each is one long coiled chain of AA with 6 transmembrane units. |
|
|
Lidocaine blocks what channels? |
Sodium channels. Prevents depolarization of neurons (no pain felt) |
|
|
Dihydropyridine mechanism? |
Allosteric antagonist to decrease opening of Ca++ channels. Slows heart and decreased contraction. Dilates vessels. For CV disease |
|
|
Fluoxetine (Prozac) and Loop diuretics (furosemide) both work how? |
Block symport |
|
|
Digoxin and ouabain both work how? |
Inhibit antiport (Na+/Ca++ exchange inhibitors). Manage heart failure |
|
|
Difference between pump and transporter? |
Transporter and energy independent. |
|
|
Examples of energy dependent transporters (pumps) |
ATP-binding cassette (ABC) transporters, Na+-K+ ATPase (sodium pump inhibitors), MDR transporters |
|
|
What do false substrates do? |
Keeps enzyme busy. Produces abnormal metabolite. |
|
|
Why do azoles and penicillins interact ith Warfarin? |
CYP2C9 is supposed to break down Warfarin. Penicillin and azoles inhibit CYP2C9. Too much free warfarin, risk of bleeding out. |
|
|
Why do Phenytoin, Alcohol, and Ginseng interact with Warfarin? |
Those three induce CYP2C9, which breaks down warfarin. Too much warfarin broken down -> not enough warfarin, risk of stroke. |
|
|
How does Viagara work |
? |
|
|
What are the 4 types of receptors? |
Ligand gates channels (ionotropic- ex. nicotinic) GPCRs (adrenergic, muscarinic) enzyme-linked receptors intracellular receptors (bind steroid hormones) |
|
|
What unit has the binding site in a ligand-gated channel? |
The alpha subunit. There are two of them (5 units altogether) so you really need two of the same molecule to bind at the same time to open the receptor. |
|
|
Where is the binding site on the alpha subunits of an ROC? |
The amino terminus |
|
|
What kind of receptor is a GABA-A receptor? |
ROC (ligand gated channel). Lets in Cl- through channel, to hyperpolarize neuron and decrease activity. |
|
|
Where is the binding site in a GPCR |
inside the pore (not outside). Ligand must be very small. In 3rd transmembrane unit (counting from n-term) |
|
|
Which receptor type is most abundant in humans? |
GPCRs |
|
|
What kind of receptor are adrenergic receptors? |
GPCR |
|
|
A stimulatory G protein (Gs) sets off what transduction pathway? |
When agonist binds receptor, G protein UNCOUPLES and activate AC in membrane. More cAMP, which activate kinases. Those kinases can either activate proteins, or activate an ion channel. It's more complex than potential-regulated ion channels. |
|
|
Describe the G(q) protein transduction pathway |
PLC cleaves the membrane phospholipid PIP2 into DAG and IP3. DAG diffuses in membrane to activate PKC which phosphorylates proteins. IP3 stimulates the release of Ca++ from ER. Calcium release also stimulates protein phosphorylation events. |
|
|
What are enzyme linked receptors? |
One transmembrane domain. N-term is ligand recognition site (external, so accomodates large ligands), catalytic domain at C-term. Example: Tyrosine kinase receptors (RTKs), which bind large hormones such as GFs and insulin |
|
|
What is unique about isulin receptor dimerization? |
It occurs even before ligand binding, unlike other RTKs |
|
|
Example of serine-threonine receptor? |
Cytokine receptors |
|
|
Example of Guanylyl receptor cyclase? |
nitric oxide receptors (blood vessels) |
|
|
Differences between Class I and Class II intracellular receptors? |
Class I are in cytosol at rest (need chaperone); Class II are bound to DNA. CLass I are homodimers; Class II are heterodimers. Class I examples: estrogen, corticosteroid receptors Class II examples: Vitamin D3, thyroid hormone receptors |
|
|
Difference between efficacy and potency |
Efficacy has to do with effect of drug; potency with the amount. |
|
|
How do we measure potency? |
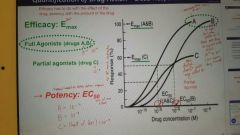
EC50. On a dose-response curve, find 50% of max response, report what drug concentration was at that point
Less potent = higher EC50 = line shifted to the right (higher drug concentration needed) |
|
|
How do you measure efficacy |
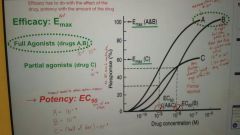
Emax- find the highest response on the dose-response curve, report drug concentration |
|
|
Describe a partial agonist in terms of efficacy and potency |
Efficacy- the dose response curve with be short, because Emax cannot reach 100% response. Potency- the EC50 will not be 50% response, but half of whatever the maximum response is (Emax) |
|
|
How do you measure therapeutic index (ratio)? |
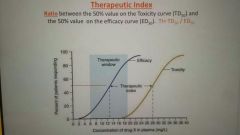
TD50/ED50 ( |
|
|
What is considered a low therapeutic index (ratio)? |
if TI <= 2. If taking double the median effective concentration (ED50) is the median toxic concentration (TD50) |
|
|
What does a graph of agonist + increasing doses of irreversible antagonist look like? |
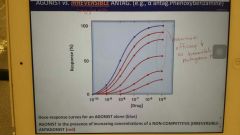
With each increase in irreversible antagonist, Emax (efficacy) decreases |
|
|
List 3 mechanisms of decreased response to drug action NOT targeting receptors (pharmacokinetics) |
Increased metabolism of drug (barbiturates) decreased biotransformation of prodrug (nitrates) physiological adaptation (which do not change [drug] in plasma. Ex: thiazides- diuretics) |
|
|
List 3 mechanisms of decreased response to drug action targetting receptors? (Pharmacodynamics) |
Desensitization: phosphorylation (seconds or minutes)
Internalization- fewer receptors available (minutes)
Downregulation- destruction of receptors- absolute decrease in receptor # (hours/days). This is relevant to opioid, amphetamine, THC tolerance. |
|
|
How is bioavailability calculated? |
Fraction of unchanged drug (fu = fraction unbound) reaching systemic circulation, after administration by any route. (Unchanged circulating dose / administered dose) |

