![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
43 Cards in this Set
- Front
- Back
|
RECAP: describe the structure of the ANS |

•Projections from spinal cord to ganglia•Presynaptic cells release acetylcholine andactivate postsynaptic (postganglionic) cells. •Postganglionic cells form junctions withsmooth muscle cells, endocrine cells, cardiac cells, hepatocytesetc. etc. |
|
|
Describe signal propagation in the ANS |

•Fast electrical propagation along axons(action potentials) •Chemical transmission at synapses andterminals (neurotransmitter release) •These steps in the relay system can beblocked pharmacologically |
|
|
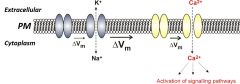
What does excitability refer to?
|
“Excitability” refers to the ability todynamically alter the electrical potential (voltage) across the plasmamembrane. |
|
|
How does a potential difference arise? |
Any difference in the concentration of charged molecules |
|
|
What is the resting membrane potential for cells?
|
-50 to -90 mV |
|
|
What are ion channels? |
•Membrane-spanning proteins that open aselective pore, allowing ion entry •Change cell excitability (mainly Na+ and K+) •Allow an influx of “signalling” ions – e.g. Ca2+ |
|
|
What is meant by membrane depolarisation? |
Inside the cell becomes more positive |
|
|
What does membrane depolarisation cause? |
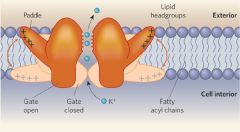
Structural re-arrangements in the ion channel protein Voltage gated potassium channel opens inresponse to depolarization |
|
|
What happens during action potential generation 1? |
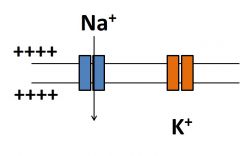
•Depolarization opensNa+ channels (fast)•Na+floods into the cell down its electrochemical gradient •This depolarizes the membrane even more (goes more positive) |
|
|
What happens at action potential generation 2? |
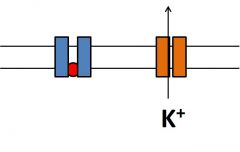
•K+ channels open(more slowly than Na+channels) •K+floods out of the cell down itselectrochemical gradient •Na+channels inactivatepreventing further depolarization •This repolarizesthe membrane |
|
|
What happens during action potential generation 3? |
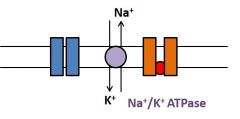
•K+ channels inactivate. •Ion pumps and transporters use energyfrom ATP or counter-transport to re-establish resting membrane conditions |
|
|
What does a graph of the changing membrane potentials look like? |

|
|
|
What is saltatory conductance?
|

•Mechanism for increasing speed andreliability of conduction •Glial cells coat axons in insulatingmyelin sheets •Ion channels are clustered at unmyelinated“Nodes of Ranvier” •Action potential “jumps” between nodes |
|
|
What happens when the action potential reaches the synapse or terminal?
|

Once the action potential reaches asynapse (neuron to neuron junction in the ganglion) or terminals to other celltypes (e.g. smooth muscle, endocrine cells), chemical transmitter is released. |
|
|
How are transmitters synthesised and stored?
|
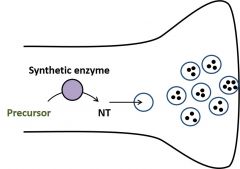
•Synthetic enzymes make transmitter fromprecursors •Transmitter is transported into vesiclesin the presynapticnerve terminal Synthetic enzymes generate NT frominactive precursors. Vesicular transporters use activetransport to concentrate NT within the vesicle. |
|
|
How are vesicles released?
|

•An incoming action potential depolarizesthe terminal •Voltage-gated calcium channels open •Calcium triggers vesicle fusion andtransmitter release |
|
|
How are the postsynaptic receptors activated? |

•Receptors for the transmitter on thepostsynaptic cell are activated. •Ligand-gated ion channels open. |
|
|
What opens ligand-gated ion channels? |
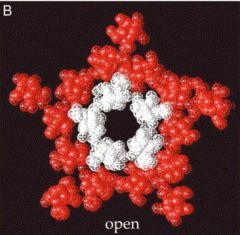
•Binding of an agonist to the receptoropens an ion channel •This depolarizes the postsynaptic cell e.g Nicotinic acetylcholine receptornAChROpen pore lets Na+ and K+ (andsome Ca2+ ) ions through. |
|
|
How are NT's cleared from the intermembrane space? |

•The synaptic “signal” must be turned off •Enzymatic degradation or active uptake oftransmitter eliminates it from the extracellular space |
|
|
What happens when the NT reaches the target cell (terminal cell)? |

•Boutons to smooth muscle, endocrine cellsetc. activate G protein coupled receptors (GPCRs)•Activation or inhibition of secondmessenger pathways |
|
|
What happens for sympathetic innervation (stimulation)? |

•Noradrenalineacts on alpha and beta adrenoceptors •a and b receptors have variable effectsdepending on cell type |
|
|
What happens for parasympathetic innervation? |

•Acetylcholineacts on muscarinic(M) receptors •M1,M2 and M3 receptors have variable effects depending on cell type |
|
|
RECAP: Describe synaptic transmission |

•Incoming action potential triggersvesicle fusion •Activation of postsynaptic receptorspropagates AP •Clearance terminates signal |
|
|
What would blocking the voltage gated Na+ channels do? |
Prevent excitation of both pre-and postsynaptic cells |
|
|
What are some drugs which block the Na+ channels? |
–Lidocaine (local anaesthetic) –Lamotrigine(antiepileptic) |
|
|
What does lidocaine do? |
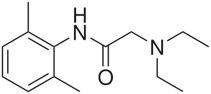
Blocks the pore of the Na+ channel after opening, preventingpassage of ions |
|
|
How can you interfere with NT synthesis? |
A false substrate competes for enzymecatalytic site Build up of inert product anddepletion of transmitter |
|
|
What is a drug which inhibits the synthetic enzymes? |
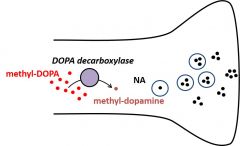
Methyl-DOPAis a false substrate for DOPA decarboxylase. Methyl-dopaminecannot be converted to noradrenaline |
|
|
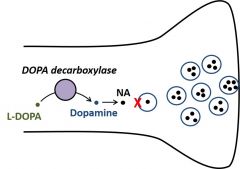
What does L-DOPA do? |
L-Dopa is the precursor to dopamine, it is used to increase dopamine concentration. It can be used as a therapy in Parkinson's disease |
|
|
What does interference with vesicle loading do?
|
Vesicles fail to load Stores depleted by on-goingactivity |
|
|
What is an example of a drug which interferes with vesicle loading? |
Reserpineblocks NA uptake (and other monoamines) |
|
|
What are some drugs which interfere with vesicle release? |
•Calcium triggers vesicle fusion andtransmitter release - Conotoxin blocks calcium channels - Botulinumtoxin (Botox)degrades vesicle release machinery |
|
|
What do antagonists of ionotropic receptors (ligand gated ion channel) do? |

Antagonists of ionotropicreceptors prevent depolarization of the postsynaptic cell Several mechanisms: occupyNT binding site, prevent channel opening,or block the open pore |
|
|
What do antagonists of metabotropic receptors do? |

•Antagonists of metabotropicreceptors prevent target cells from responding to released NT•Occupy binding site (red) orinhibit G protein (green) |
|
|
Examples of antagonists
|
–Tropicamide (mAChRblocker) –Atenolol (bR blocker) –Tamsulosin (aR blocker) |
|
|
Examples of agonists |
–Salbutamol (bR agonist) –Pilocarpine (mAChRagonist) –Nicotine(nAChRagonist) |
|
|
What does inhibition of transporters or degradation of enzymes do? |
Inhibition of transporters or degradationenzymes prolongs activation of post synaptic cell |
|
|
Name some drugs which inhibit the clearance of transmitters |

- Amitriptylineinhibits NA uptake (blue) - Neostigmineblocks acetylcholinesterase (red) |
|
|
Examples of B-blockers (antagonists), their indictations, contra-indications, and side effects |
•Atenolol, propranolol,acebutolol •Indications: –Hypertension,angina, arrythmias •Contra-indications: –Asthma,bradycardia,severe peripheral arterial disease, etc. •Side effects: –Bronchospasm, GIdisturbances, hypotension, bradycardia, visual disturbances, headache,dizziness, etc. etc. |
|
|
What is the B-blocked mechanism of action? |
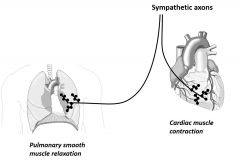
•Counteracts sympathetic input •Reduce cardiac output •Risk of pulmonary side effects |
|
|
Examples of B-blockers (anti-muscarinics), their indications, contra-indications, and side effects |
•Muscarinic acetylcholine receptor antagonists: •Hyoscine, atropine, oxybutynin •Indications –Premedicants todry bronchial and salivary secretions (during surgery), bradycardia, GIdisorders, urinary incontinence, cycloplegia •Contra-indications –Glaucoma,myasthenia gravis, urinary retention •Side effects –Drymouth, blurred vision, constipation, tachycardia, palpitation, arrythmias |
|
|
What is the antimuscarinic mechanism of action? |
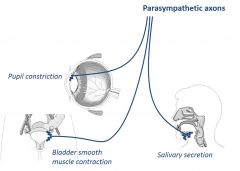
•Counteracts parasympathetic input •Inhibits glandular secretion •Blocks smooth muscle contraction |
|
|
What are clinical signs of poisoning or defects in autonomic control? |
•Pupil dilation –Mydriasis(pupil dilation) –Miosis(pupil constriction) –Lightreflex •Heart beat rate –Bradycardia(decreased rate) –Tachycardia(increased rate) •Sweating/salivary outflow –Profusesweating –Drymouth |

