![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
19 Cards in this Set
- Front
- Back
|
What is the mechanism of action of dantrolene? |
Not understood. Direct skeletal muscle relaxant. Blocks calcium release from the intracellular store in the SR. Debatable whether it is due to dihydropyridine or RYR1 receptor. Does not prevent calcium efflux from RYR2 receptors in the heart Less affinity for RYR3 receptors (implicated in NMS) |
|
|
What is the dosing regimen of Dantrolene? |
2 - 2.5mg / kg IVI up to max 10mg/kg/24hrs to control symptoms Then 1mg/kg 6hrly for 4doses OR Infusion 4-6mcg/kg/min to prevent recurrence. |
|
|
How many vials of dantrolene would a 72kg patient require initially? |
2.5 x 72 = 180mg Each vial has 20mg 180 / 20 = 9vials for initial dose. Diluent 9 x 60mls sterile water = 540mls. |
|
|
List four side effects of dantrolene. |
Acute SE 1. Muscle weakness 2. Phlebitis 3. Respiratory failure 4. GIT: N&V, diarrhea, 5. Drowsiness, dizziness, confusion 6. If during C/S: floppy child syndrome, uterine atony Chronic SE 1. Muscle weakness longer than 48hrs 2. Respiratory insufficiency 3. Liver dysfunction 4. Rarely: gastric irritation, abdo cramps, constipation, dysphagia, enuresis, Visual disturbances & acne-type rash |
|
|
List 4 metabolic effects that are likely to be seen in malignant hyperthermia and their management. |
Early *1. Elevated EtCO2, Tachypnea if on spontaneous Respiration *2. Increased oxygen consumption *3. Mixed metabolic and respiratory Acidosis 4. Profuse Sweating 5. Mottling of skin
Later *1. Hyperkalaemia *2. Rapid rise in core body temp 3. Elevated creatine kinase 4. Elevated myoglobin 5. Myoglonuria
Mx Hyperventilation Oxygen 100% Sodium bicarbonate Insulin, dextrose, calcium gluconate Cooling measures Fluids, fluids |
|
|
What is a single-nucleotide polymorphism? |
The most common type of genetic or allelic variation. This is called the point of mutation |
|
|
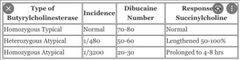
Describe the genetic basis of inherited suxamethonium apnoea. |
It is the presence of genetically determined variants of the enzyme pseudocholinestarase. The genotypes are Normal enzyme Atypical enzyme ‐ Jews in Iran & Iraq. Flouride sensitive ‐ Huntingtons chorea Silent gene - south africa Patients with normal enzyme have a normal duration of action Pts with a herozygous abnormal gene have a prolonged duration of action And homozygous have a greatly prolonged duration of action |
|
|
Describe the genetic basis of malignant hyperthermia. |
Autosomal dominant Chromosome 19 - RYR1 Mutation & Chromosome 17 - dihydropyridine receptor Mutation. This causes a channelopathy of the above receptors leading to calcium induced release of Calcium from the SR instead of DIRC when the alfa subunit of the dihydropyridine receptor binds to ryanodine receptor to open & release calcium.
|
|
|
Briefly discuss the clinical impact of variations in pharmacogenetics on ondansetron and suggest an alternative therapy in the same drug class that avoids this effect. |
Some pts do not respond to ondansetrone. The mechanism being ultra-rapid drug metabolism by CYP2D6. Leading to 5x more incidence of vomiting, but no difference in incidence of nausea. Ganisetrone is broken down by CYP3A4 & is not ultra-rapidly metabolised. |
|
|
Briefly discuss the clinical impact of variations in pharmacogenetics on codeine. |
When the enzyme CYP2D6 is non-functional or non-existent, the pt is more susceptible to pain due to ffg reasons. 1. Defective synthesis of endogenous opioids 2. CYP2D6 converts codeine to morphine. Abnormality results in varied pain relief to codeine. (Affects 6-7% Caucasians) 3. Tramadol slightly affected via the same mechanism
|
|
|
What is the significance of a dibucaine number of 45? |
|
|
|
List 5 causes of an increased duration of neuromuscular block after suxamethonium administration. |
1. Physiological: 3rd trimester pregnancy, neonates 2. Acquired: Liver dx, carcinoma, debilitating conditions, collagen dx, renal dx, malnutrition, myxoedema 3. Drugs: echothiophate, neostigmine, chlorpromazine, cyclophosphamide, MOAI, pancuronium, bambuterol, contraceptives, organiphosphates, hexaflourenium 4. Other causes: plasmaphoresis, tetanus, burns, extracorpereal circulation, radiation therapy |
|
|
List the basic post-operative management strategies in a patient with suspected “scoline apnoea”. |
1. Mechanical ventilation until adequate muscle tone returned 2. IVI midazolum or low dose Anaesthesia to arrest awareness 3. Exclude other causes of apnea 4. Monitor muscle function with peripheral nerve stimulator 5. Draw blood sample for pseudocholinestarase activity and dibucaine number 6. If tests are positive, medic alert bracelet & test relatives |
|
|
Define the term: Pharmacogenetics. |
Hereditary basis for differences in a single gene that influences the response to a specific therapeutic agent. |
|
|
Define the term: Pharmacogenomics. |
Explains how the entire genome (all genes) can influence the interindividual variation/response to a drug. |
|
|
Define the term: Gene. |
The sequence of DNA that occupies a specific position on the Chromosome and encodes a particular protein which contributes to particular functions and characteristics of an organism |
|
|
Define the term: Allele. |
One of two or more forms of a gene that occupies a specific position on a specific Chromosome. Humans have two alleles at each gene locus, one inherited from each parent. |
|
|
Briefly describe the clinical implications of pharmacogenomic effects on codeine metabolism. |

|
|
|
Which class of anaesthetic drugs are affected by pharmacogenomic variation in the CYP2E1 enzyme system? |
Anaesthetic gases Sevoflourane: sole catalyst for deflourination Methoxyflurane: principal but not sole enzyme for metabolism Isoflurane and enflurane: responsible for a significant fraction of metabolism |

