![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
100 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
List the steps leading to "Phase 1 Platelet Plug"
|
1. Vessel damage
2. Vasospasm 3. Platelet adhesion 4. Platelet aggregation 5. Viscous metamorphosis 6. Temporary Hemostasis |
|
|
|
Upon damage, what do endothelial cells release to cause Vasospasm (vessel constriction)?
|
Endothelin
|
|
|
|
Platelets bind to damaged vessels via __1__, which binds to __2__; and __3__, which binds __4__
|
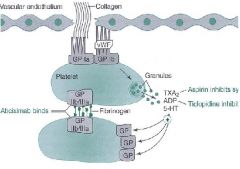
1. GP 1a
2. Collagen 3. GP 1b 4. von Willebrand factor Platelets: GP 1a and 1b Endothelial cells: Collagen and von Willebrand factor |
|
|
|
In platelet aggregation, platelets bind to themselves via __1__, which also bind __2__ and other macromolecules
|
1. GP IIb / IIIa
2. Fibrinogen |
|
|
|
What is "Viscous Metamorphosis" of platelets?
|
loss of individual platelet membranes to form a gelatinous mass
|
|
|
|
Thrombin formation induces these 3 events in platelets
|
1. release of ADP = further platelet aggregation
2. Serotonin release 3. Prostaglandin synthesis from platelet AA |
|
|
|
Phase 2 Fibrin Plug:
Increased __1__ synthesis in platelet with decreased __2__ synthesis in damaged vessel wall |
1. Thromboxane (TXA2)= platelet aggregation and vasoconstriction
2. Prostacycline (PGI2) - vasodilator and platelet inhibitor - but is decreased in damage |
|
|
|
What induces the conversion of Fibrinogen to Fibrin?
|
Thrombin
|
|
|
|
Activation of both the intrinsic and extrinsic coagulation systems leads to teh conversion of ________ to ________
|
Prothrombin (factor II)
Thrombin (Factor IIa) |
|
|
|
Prothrombin is bound by __1__ to __2__ on the platelet surface, whereas thrombin is __3__
|
1. calcium
2. phospholipids 3. released into circulation |
|
|
|
What initiates the Intrinsic Coagulation Pathway?
|
Collagen from the damaged blood vessel
|
|
|
|
What measures the Intrinsic system of coagulation?
|
Partial Thromboplastin time (PTT)
|
|
|
|
What is PTT used to monitor?
|
Heparin therapy
|
|
|
|
Extrinsic Coagulation system:
1. Requires these factors for initiation 2. These Factors are limiting (why?) 3. What is it measured by? 4. What is it used to monitor? |
1. Tissue Factor (Tissue Thromboplastin or Factor 3
2. Factors 2, 7, 9, and 10 3. Prothrombin time 4. Warfarin therapy |
|
|
|
What are the 3 groups of things that are risk factors for Thromboembolism?
|
1. abnormalities of blood flow (anything that slows the blood)
2. abnormalities of surface in contact with blood 3. abnormalities of clotting factors |
|
|
|
List 6 examples of things that cause abnormalities of blood flow
|
1. Left ventricular dysfunction
2. Ischemic cardiomyopathy 3. CHF 4. Bed rest/immobilization 5. Venous obstruction from tumor/obesity/pregnancy 6. Atrial fibrillation |
|
|
|
List 6 things that can cause abnormalities of surface in contact with blood (risk factors for thromboembolism)
|
1. Vascular injury
2. Heart valve disease 3. Heart valve replacement 4. Atherosclerosis 5. Acute myocardial infarction 6. Indwelling catheters |
|
|
|
List 3 Endogenous Anticoagulant deficiencies that can lead to Thromboembolism
|
1. Protein C ***
2. Protein S *** 3. Antithrombin III *** Vitamin K - dependent |
|
|
|
What syndrome could lead to Thromboembolism?
|
Antiphospholipid antibody syndrome
|
|
|
|
What 3 things lead to an increase in clotting factors and increase the risk for Thromboembolism?
|
1. Estrogen therapy -> affects the synthesis of coagulation factors
2. Pregnancy -> increased estrogen 3. Malignancy |
|
|
|
Arterial Thrombosis:
__1__ > __2__ = __3__ thrombus |
1. Platelets
2. Fibrin 3. White |
|
|
|
What 4 events/things can cause Arterial Thrombosis?
|
1. Local ischemia
2. MI 3. Unstable angina 4. Stroke |
|
|
|
What is a prophylaxis for Arterial Thrombosis?
|
Antiplatelet therapy (aspirin)
* b/c platelet are more prominent than fibrin in arterial side |
|
|
|
Venous Thrombosis:
__1__ > __2__ = __3__ thrombus |
1. Fibrin
2. Platelets 3. Red |
|
|
|
Prophylaxis for Venous Thrombosis
|
Anticoagulant therapy
- Heparin - Warfarin |
|
|
|
Chemical name for Aspirin
|
Acetylsalicylic Acid
|
|
|
|
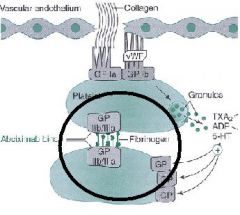
Aspirin inhibits the synthesis of __1__ by IRREVERSIBLE __2__ of __3__ in Platelets
|
1. Thromboxane (TXA2)
2. acetylation 3. COX-1 |
|
|
|
TXA2 increases the __1__ pathway in platelets causing __2__
*reduced by aspirin |
1. PIP2 -> increases expression of Gp IIb/IIIa
2. aggregation -TXA2, ADP, and Serotonin cause expression of Gp IIb/IIIa |
|
|
|
TXA2 is a potent stimulator of __1__ and __2__
|
1. Platelet activation
2. Vasoconstriction |
|
|
|
COX-1 is in __1__ and is inhibited by low doses of aspirin
COX-2 is in __2__ and produces __3__ |
1. Platelets
2. Endothelial cells 3. Prostacyclin (PGI2) |
|
|
|
COX-2 is inhibited by high or low doses of aspirin?
|
High
|
|
|
|
Aspirin is useful in preventing or reduing the risk of __1__ and __2__ due to its antithrombotic effects
|
1. MI
2. transient ischemic attacks |
|
|
|
Aspirin's antithrombotic effects on platelets are seen __1__ days after administration and lasts for the duration of the platelets life-span, usually __2__ days
|
1. 1-2
2. 7-10 |
|
|
|
Stop Aspirin __1__ before surgery
Stop other NSAIDs __2__ before surgery |
1. 1 week
2. 2-3 days |
|
|
|
What is Ticlopidine's mechanism of action?
|
1. inhibits platelet activation by irreversibly blocking ADP receptors
2. Inhibits Fibrinogen binding by preventing GP IIb/IIIa expression = blocks platelet-platelet binding *ADP antagonist |
|
|
|
What 3 things is Ticlopidine used as?
|
1. alternative to Aspirin to prevent initial or recurrent thromboembolic stroke
2. Post-MI reinfarction prophylaxis 3. Unstable angina |
|
|
|
How is Ticlopidine administered?
|
Orally
*rapidly and well (>80%) absorbed *extensively metabolized |
|
|
|
Why is Ticlopidine only given to patients who are intolerant or unresponsive to aspirin?
|
b/c in rare cases it causes SEVERE BONE MARROW TOXICITY
*also increases Liver Functional Enzymes |
|
|
|
Ticlopidine causes increased bleeding when given with these drugs
|
1. Warfarin
2. Heparin 3. other antiplatelet drugs 4. NSAID drugs |
|
|
|
Ticlopidine:
__1__ decreases its clearance It decreases the clearance of __2__ |
Cimetidine
Theophylline |
|
|
|
T or F: Usually Clopidogrel is preferred over Ticlopidine as an ADP antagonist
|
True
**Clopidogrel has lower incidence of adverse skin, GI, or HEMATOLOGIC rxns |
|
|
|
Clopidogrel or Ticlopidine:
Which has less drug-drug interactions? |
Ticlopidine
|
|
|
|
Clopidogrel trade name
|
Plavix
|
|
|
|
Clopidogrel has a similar mechanism to Ticlopidine but has a lower incidence of these 3 adverse effects
|
1. Cutaneous rxns
2. GI effects 3. HEMATOLOGIC rxns |
|
|
|
Clopidogrel is used to reduce ______ in patients with a history of recent stroke, recent MI, or established peripheral vascular disease
|
Atherosclerosis
|
|
|
|
Clopidogrel inhibits the activity of ______ and therefore increase the plasma concentrations of drugs
|
CYP 2C9
|
|
|
|
Clopidogrel may increase the plasma concentrations of these 6 drugs
|
1. Fluvastatin
2. Phenytoin 3. Tamoxifen 4. Tolbutamide 5. WARFARIN 6. many NSAIDS |
Eric Clopidogrel inhibits 2C9. His gf TAMMI has the FLU and she wears a PHENY-pack with her NSAIDS in it. Their country goes to WAR with the TOLBUT's
|
|
|
Abciximab is a new class of drugs called _________?
|
Platelet-receptor glycoprotein inhibitors
|
|
|
|
What is the mechanism of actions of Abciximab?
|
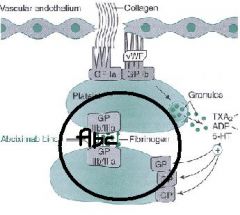
monoclonal antibody that binds to glycoprotein receptor IIb/IIIa on activated plates preventing platelet aggregation
- inhibits fibrinogen, vWF, and others from cross-linking platelets |
|
|
|
How, what for, and with what is Abciximab given?
|
How = IV
What for = Angioplasty, atherectomy, stent placement What with = Clopidogrel |
|
|
|
What is the most common adverse effect of Abciximab?
|
Bleeding
|
|
|
|
Non-peptide Platelet-receptor glycoprotein inhibitor similar to Abciximab, but not a monoclonal antibody
|
Tirofiban
|
|
|
|
Cyclic peptide platelet-receptor glycoprotein inhibitor similar to Abciximab, but not a monoclonal antibody
|
Eptifibatide
*Circular peptide Epithet inhibits of Gp IIb/IIIa |
|
|
|
What is the main use of Dipyridamole?
|
In combo with Warfarin -> inhibits embolism from prosthetic heart valves
|
|
|
|
What 2 things does Dipyridamole do?
|
Coronary vasodilator
Inhibits platelet aggregation |
|
|
|
Why is Dipyridamole not used to treat angina?
|
Even though it is a coronary vasodilator, it dilates healthy vessels instead of diseased ones and makes angina worse
|
|
|
|
Dipyridamole's mechanism is not clear, but it is in part due to increase in _____ because of inhibition of _____
|
cAMP
Phosphodiesterase |
|
|
|
In combination with aspirin, Dipyridamole reduces __1__ in patients with __2__ disease
|
1. thrombosis
2. thrombotic |
|
|
|
Antithrombotic, antiplatelet, and vasodilatory drug that inhibits Phosphodiesterase III and thereby increases cAMP levels which prevents platelet aggregation
|
Cilostazol
|
|
|
|
What is Cilostazol used for?
|
Intermittent claudication and peripheral vascular disease
*Buerger's disease |
|
|
|
Drug that reduces elevated platelet counts in patients with essential thrombocytosis (too many platelets)
|
Anagrelide
|
|
|
|
What is Anagrelide's mechanism of action?
|
inhibits Megakaryocyte development in the late postmitotic stage = inhibits formation of platelets
|
|
|
|
Anagrelide is approved for the treatment of __1__ secondary to __2__ disorders, such as __3__ and __4__ to reduce the risk of Stroke and MI
|
1. Thrombocytosis
2. Myeloproliferative 3. Polycythemia vera 4. Chronic Myelogenous leukemia |
|
|
|
Give 3 examples of Calcium chelators
|
1. Oxalic acid
2. Sodium Citrate 3. Disodium edetate *inhibit blood coagulation IN VITRO, not in humans!!! |
|
|
|
Accelerate the action of Antithrombin III to neutralize thrombin and other coagulation factors
|
Heparins
|
|
|
|
Direct thrombin inhibitors
|
Rudins
|
|
|
|
Interfere with the hepatic synthesis of functional Vitamin K-dependent clotting factors
|
Coumarin derivatives = Warfarin
|
|
|
|
What is the source of Heparin?
|
Pig intestinal mucosa
Bovine lung |
|
|
|
What is the chemical structure of Heparin?
|
Sulfated mucopolysaccharide = acidic = negatively charged
|
|
|
|
What are the routes of administration of heparin?
How is it never given and why? |
Continuous IV drip or Intermittent Subcutaneous
Never Intramuscular due to risk of hematoma at injection site Oral lacks absorption |
|
|
|
What is the advantage of Heparin over Warfarin?
|
Heparin's action is IMMEDIATE
|
|
|
|
What is the problem with Heparin and its pharmacokinetics?
|
Large charged molecule -> sticky -> binds extensively to endothelial cells and plasma proteins
|
|
|
|
Is Heparin clearance Dose-dependent or dose-independent?
Why? |
Dose-dependent b/c plasma levels of heparin increase considerably once binding sites are saturated
*most drugs are Dose-INDEPENDENT |
|
|
|
What is the Therapeutic goal of Heparin?
|
to prolong the Partial Thromboplastin Time (PTT) to 1.5-2.5 times normal
*measured just before the next dose for intermittent therapy |
|
|
|
-The protease inhibitor, __1__, forms a 1:1 complex with clotting factor proteases
-This interaction is slow, but is stimulated 1000-fold by __2__, which binds to Antithrombin III |
1. Antithrombin III
2. Heparin |
|
|
|
-The heparin-antithrombin complex inactivates __1__ (main mechanism)
-The heparin-antithrombin III complex also inactivates __2__, which occurs earlier in the cascade |
1. Thrombin (IIa)
2. Xa |
|
|
|
During active thrombosis, the anticoagulant effect of heparin is primarily due to inactivation of __1__
With little or no thrombosis, the anticoagulant effect is largely due to inactivation of __2__ |
1. Thrombin (IIa)
2. Factor Xa |
|
|
|
What are the Contraindications for Heparin use? (4)
|
1. Bleeding disorders and disorders that predispose to bleeding (hemophilia, thrombocytopenia)
2. Patients with advanced liver or kidney disease 3. Severe HTN -> bleeding into brain 4. Infections -> active TB, infective endocarditis |
|
|
|
Heparin is preferable to other anticoagulants during __1__ due to lack of __2__
|
1. pregnancy
2. placental transfer *in contrast to Warfarin |
|
|
|
With bleeding as an adverse effect of Heparin, what can be done to minimize it?
|
Careful monitoring of PTT and Platelet counts
|
|
|
|
1. Since Heparin is an animal product, what adverse can happen?
2. Long-term use of Heparin can cause this adverse effect |
1. Allergic reaction
2. Osteoporosis |
|
|
|
Describe Type I Thrombocytopenia caused by Heparin
|
-Immediate, transient, and reversible heparin-induced platelet sequestration
-heparin binds to platelet and causes them to lyse |
|
|
|
Describe Type II Thrombocytopenia caused by Heparin
What is the name for it? |
IgG develops to Heparin bound to Factor 4 on Platelets
Heparin-induced Thrombocytopenia (HIT) |
|
|
|
What is a paradoxical effect related to Heparin-induced thrombocytopenia (HIT)?
|
Thromboembolism
*paradoxical b/c Heparin is an anticoagulant **caused by IgG/Heparin/Platelet complex |
|
|
|
What is the antidote to Heparin?
|
Protamine Sulfate
|
|
|
|
Protamine sulfate is a __1__ peptide that binds to Heparin
Excessive antidote must be avoided b/c protamine itself is an __2__ |
1. basic (acid/base or anion/cation interaction)
2. Anticoagulant |
|
|
|
Administer __1__ protamine sulfate IV for each __2__ units of heparin remaining in the patient
|
1. 1 mg
2. 100 units |
|
|
|
What is the disadvantage of Low Molecular Weight Heparin (LMWH)?
|
Protamine is much less capable of reversing its effects
|
|
|
|
What are the 3 Low Molecular Weight Heparins (LMWH)?
|
Enoxa-parin
Dalte-parin Tinza-parin |
|
|
|
LMwH's were first approved for primary prevention of __1__ after __2__ therapy
|
1. deep vein thrombosis
2. hip replacement |
|
|
|
When are LMWH's contraindicated?
|
in Heparin-induced Thrombocytopenia
|
|
|
|
How are LWMH's monitored?
When are they more often monitored? |
-anti-Xa activity assay
-when used in pregnancy *more expensive than PTT |
|
|
-
|
-
|
|
|
|
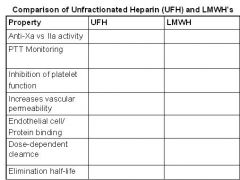
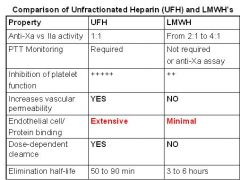
What is an advantage of LMWH's over Unfractionated Heparin (UFH)?
|
Pharmacokinetics = dose-independent = are not sticky to endothelial cells or plasma proteins
|
|
|
|
What do LMWH's have more activity against, Factor Xa or IIa?
|
Xa
|
|
|
|
Is a synthetic pentasaccharide anticoagulant that only exerts antithrombotic activity as a result of ATIII-mediated selective inhibition of Factor Xa
*Has no effect on Thrombin (IIa) |
FondaPARINux
Fondles Factor 10a |
|
|
|
How is Fondaparinux different from Heparin and LMWH?
|
Selectively inhibits Factor Xa
*does not affect Thrombin (IIa) |
|
|
|
What is the elimination half-life of Fondaparinux?
How is it administered? |
18 hours = allows once-daily dosing
Subcutaneously ***Fondles factor 10a for 18 hours under the skin |
|
|
|
Clinical trials are needed to determine if Fondaparinux is a safe alternative to heparin in patients at risk for what?
|
Heparin-induced Thrombocytopenia
*does not bind to Platelet Factor 4 |
|
|
|
What 3 things is Fondaparinux being used for?
|
1. Venous thromboembolism prophylaxis following orthopedic surgery
2. Treatment of Pulmonary Embolism 3. Treatment of Deep Vein Thrombosis |
|

