![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
39 Cards in this Set
- Front
- Back
|
Inotropic Drugs: what do they do?
|
Alter the force of cardiac contraction
positive: increase cardiac contraction negative: decrease cardiac contraction Increased cAMP causes increased Calcium in the cytosol which increases cardiac contractility |
|
|
Adrenergic Drugs: what do they do?
|
Work at adrenergic receptors and primarily modulate the function of SNS
They're Adrenomimetics: promote effects of norepinephrine and epinephrine, dopamine at adrenergic receptors in SNS |
|
|
Adrenergic Recptors: which ones are there?
|
A1, A2, B1, B2, D1-5
|
|
|
Alpha 1 receptors and their properties, antagonists, and agonists.
|
A1 agonists cause vasocontriction and increase BP
Agonist: Phenylphrine-causes increase in IP3 and DAG Antagonist: Prazosin Signal Transduction: binding causes increase in IP3 (thereby causing an increase in cytosolic Ca) and an increase in DAG (which activates PKC) all of this stimulate downstream kinases, and the release of Ca from SR leads to smooth muscle contraction |
|
|
Alpha 2 Receptors and their properties, agonist, and antagonist
|
Three types: 1-C
Agonists: Clonidine for all types, Oxymetazoline for type A Agonists will decrease cAMP Antagonists: Yohimbe Agonists will decreasse cAMP levels and inhibit PKA on the presynaptic terminal where they will be bound by norep in a negative feedback loop decreasing further secretion of norep and inhibit the SNS stimulatory response |
|
|
Beta Receptors and their properties, agonists and antagonists
|
Three types 1-3
Agonist: isoproterenol is for all three types, dobutamine for B1, Albuterol for B2 Antagonists are propranolol for all three types, Betaxolol for B1, Butoxamine for B2 Agonists will cause an increase in cAMP producing muscle relaxation. Signal Transduction: accumulation of cAMP wil cause activation of PKA via cAMP |
|
|
Dopamine receptors and their types and agonists, and antagonists and their properties
|
Five types of receptors 1-5
Agonists: General Agonist is Dopamine, Fenoldopam for D1 D1 and D5 cause increased cAMP and smooth muscle contraction D2-4 cause decreased cAMP and smooth muscle relaxation |
|
|
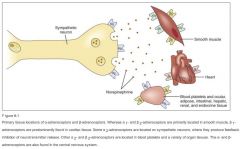
Common locations of receptors: word form
|
A1 and B2 on smooth muscle
B1 on cardiac tissue A2 on sympathetic neurons (prod inhibition of NT rel) other A2 and B2 on blood platelets and organs other A and B on CNS |
|
|
Common locations of receptors: PICTURE FORM
|
|
|
|
Locations of A1 receptors and their function at these locations
|
vascular smooth muscle-contraction
radial muscle of iris - contraction prostate- contraction |
|
|
Locations of A2 receptors and their function at these ocations
|
platelets: aggregation
adrenergic and cholinergic nerve terminals-inhibition of NT release some vascular smooth muscle: contraction Fat cells: inhibition of lipolysis |
|
|
location of b1 receptors and their functions
|
heart: increased force and rate of contraction
|
|
|
B2 receptor location and function
|
respiratory uterine and vascular smooth muscle: promotes smooth msucle relaxation
|
|
|
D1 and D2 locations and functions
|
D1 smooth muscle: dilate renal blood vessels
D2 nerve endings: modulates transmitter release |
|
|
Tolerance and Tachyphylaxis
|
Tolerance: progressively reduced response to a specific drug requiring an increase in concentration to achieve desired effect
Tachyphylaxis: acute decrease in the response to a drug after admin |
|
|
Mixed Alpha and Beta Agonists: which drugs are these?
|
Epinephrine, norepinephrine
|
|
|
epinephrine (adrenalin): what does it affect and what are it's effects
|
Affects A1=A2 and B1=B2
Secreted by adrenal medulla and potent agonist at all B and A adrenoceptors CV effects: B1 stim: increased chronotropy (HR) and increased myocardial contractility: increase coronoary O2 demand and systemic BP B2: stim: peripheral vasodilation, decreased PVR, decreased diastolic BP A1 stim: increases vascular smooth muscle contraction, increased PVR and BP B-AR stimulation causes bronchial smooth muscle relaxation, increased blood glucose, increase lipolysis, increased RENIN and RAS activation VARIABLE EFFECT ON BP due to opposing actions of epi |
|
|
Clinical indications of epinephrine
|
First choice drug for acute bronchospasm and respiratory manifestations of anaphylaxis
-hypotension and cardiac arrest |
|
|
Adverse effects of Epinephrine
|
Cardiac: tachycardia, arrhythmias, hypertension, palpitations, precipitations of myocardial ischemia and stroke,
Tremor and restlessness |
|
|
What does norepinephrine affect and what are it's effects?
|
A1=A2 and B1>>B2, endogenous sympathetic NT
Has a greater effect for B1 adrenoreceptors than epinep: will constrict all blood vessels POTENT CARDIAC STIMULANT AND VASOCONSTRICTOR SIGNIFICANTLY increases peripheral vascular resistance and BP |
|
|
Clinical Indications of NOREPI
|
USED FOR ACUTE MI or ACUTE HYPOTENSIVE STATES
As an often adjunct therapy for cardiac arrest |
|
|
Adverse effects of NOREPI
|
bradycardia, arrhythmias, hypertension, palpitations, precipitation of myocardial ischemia and stroke
If the BP is very high, carotid bodies sense the increased BP and send signal to the vasomotor center which comes back through the vagus nerve to cause severe inhibition of HR leading to Bradycardia ischemic injury due to constriction and hypoxia, severely reduced renal blood flow and reduced glomerular filtration and oliguria |
|
|
Alpha Adrenergic Agonists: which ones exist?
|
Phenylephrine, Clonidine,
|
|
|
Phenylephrine: where does it work, what are its effects, what are it's clinical indications, and what are the adverse effects?
|
A1>A2>>>>B
Not a catechol and thus has a long duration CV effects: increased PVR and BP, reflex decrease in HR from too much which is reversed by ATROPINE no direct inotropic or chronotropic activity A1 eye dilation, A1 stim: vascoconstriction and reduction of mucosal edema/congestion Clinical Indication: hypotension, nasal and sinus congestion, Adverse effects: reflex bradycardia and elevated BP |
|
|
Clonidine: where does it work and what are it's effects?
|
REDUCE PVR, HR, and CO
SELECTIVE A2 agonist A2>A1>>>>>B DOMINANT Central Effect: decrease sympathetic outflow, increase parasymp outflow, lower BP and induce bradycardia NONDOMINANT Peripheral effect due to decrease in cAMP: vascular smooth msucle contraction, platelet aggregation inhibition |
|
|
clinical indications of clonidine?
|
hypertension
offlabel indications; withdrawal from addictive substances, menopausal hot flashes, ADHD, psychoses, pts underoing anesthesia |
|
|
Mechanism of Action for clonidine
|
Activate A2 receptors in vasomotor center causing reduction in sympathetic nervous system which will overcome the peripheral effects of the drug
|
|
|
Adverse Effects of clonidine and drug interactions
|
sedation, dry mouth, depression
withdrawal can cause life threatening hypertensive crisis drugs with A2-Adrenergic blocking activity will inhibit action of clonidine (ticyclic antidepress and alpha lblockers)...lead to hypertension due to lack of sympathetic actions being blocked |
|
|
Beta Adrenergic Agonist: what is it, what does it do, clinical indications and adverse effects
|
DOBUTAMINE
B1>B2>A negative isomer is A1 antag and positive is A1 agonist, both are B agonists with the positive being 10x potent. Induces poisitive inotropy and minimal increase in HR BP changes are variable Clinical indication: acute heart failure and rarely exacerbation of chronic heart failure Adverse effect: tachycardia, arrhythmias, tachyphylaxis, increased O2 demand, more angina |
|
|
Dopamine Agonists: what are they?
|
Intropin/dopamine, Fenoldopam, bypyridines
|
|
|
What does Dopamine/intropin do, where, clinical indications, adverse effects?
|
D1=D2>>B1>>A1
D1 stim causes vasodilation important for renal flow D2 stim (presynp) suppresses NE release B1 stim occurs in hi doses A1-adrenergic stim even higher doses req and will cause vasoconstriction COUNTERING D1 therapeutic effect Clinical Indic: CHF, need for renal perf, shock via poor perfusion in MI sepsis and trauma Adverse eff: Tachycardia, arrhythmias, hypertension, palpitations |
|
|
What does fenoldopam do, where, and what's it for?
|
D1>>D2 causing peripheral vasodilation and used for SEVERE HYPERTENSION
|
|
|
Bipyridines: Inamrinone and Milrinone : what are they, what do they do, where, how, clinical indications, and adverse effects
|
inhibit PDE3: increase cAMp levels cos it can't be cleaved to make AMP), leading to increased Ca and increased contractility in heart and vasodilation in smooth muscle, decreasing preload and afterload, and not changing HR
Clinical: acute heart failure/exacerbation of CHF Adverse: Inamrinone-thrombocytopenia, liver damage, nausea vomitting Milrinone-less tox but can cause arrhythmias |
|
|
Cardiac Glycosides: which drug and what is the mech
|
DIGOXIN
MECH: 1. inhibit cellular sodium pump 2. intracellular sodium increases 3. inhibition of na ca exchange 4. rise in intracellular ca 5. more ca ready to interact with heart cells |
|
|
Mechanical effects of Digoxin
|
increased cytosolic Ca
Increased rate of contraction and relaxation Increased amplitude of contractions |
|
|
Parasympathetic effects of DIGOXIN
|
Observed when doses cause central vagus stimulation
SA node: decrease HR AV: decrease conductivity and increase refractory |
|
|
Clinical indications and adverse effects of Cardiac glycosides
|
Used for CHF
Adverse effect: LOW MARGIN OF SAFETY, cardiac arrhythmias, premature ventricular beats, bigeminy, AV block, ventricular tachycardia, ventricular fibrillation diarrhea, vomiting, anorexia aberrations in color perception, disorientation, hallucinations |
|
|
Drug interactions and toxicity
|
Hyperkalemia will inhibit effects of digoxin:
Ka sparing diurectics: don't use ACEi, ARBS, Renin Inhibitors hypokalemia will increase effects: thiazide and loop diurectics: don't use Ca-exacerbate effects of digitalis while magnesium does the opposite Give antidigoxin antibody DIGIBIND AND POTASSIUM SUPPLEMENTATION |
|
|
CHART about cardiac glycoside
|

|

