![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
52 Cards in this Set
- Front
- Back
|
What is anesthesia
|
State of the patient in which no movement occurs in response to a painful stimuli; often with loss of consciousness
|
|
|
What are the components of the anesthetic state?
|
- Amnesia - absence of memory during anesthesia
- Unconsciousness (not always necessary) - Analgesia - inability to interpret, respond to, and remember pain - Noxious (painful) stimuli do not evoke movement or autonomic responses |
|
|
How do you determine / measure anesthetic potency?
|
- Dose of anesthetic that prevents movements in response to pain in 50% of patients
- For inhaled anesthetics, defined as minimal alveolar concentration (MAC) |
|
|
What is the MAC? What is it a measure of?
|
- Minimal Alveolar Concentration
- For inhaled anesthetics, this is the dose of anesthetic that prevents movements in response to pain in 50% of patients |
|
|
How do you measure the Minimal Alveolar Concentration (MAC)?
|
Continuously monitored by concentration of anesthetic in the end-tidal expired air
|
|
|
What does the Minimal Alveolar Concentration (MAC) correlate to?
|
Concentration of drug at its site of action - the brain
|
|
|
What is an advantage to using the Minimal Alveolar Concentration (MAC) as a measure of anesthetic efficacy and potency?
|
Measuring the end-point (lack of movement to pain) is easy to measure and define
|
|
|
How do you measure the potency for intravenous anesthetics?
|
Free plasma concentration that produces a loss of response to surgical incision in 50% of patients (EC50)
|
|
|
What is the old understanding of the mechanism of action of anesthetics?
|
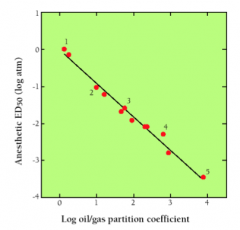
- Anesthetic potency correlates extremely well with lipophilicity
- Unitary Theory - anesthetics perturb membrane lipid ordering |
|
|
What is the Unitary Theory?
|
Anesthesia is produced by perturbation of the physical properties of the lipids of cell membranes
|
|
|
What is the current understanding of the mechanism of action of anesthetics?
|
- Anesthesia is a multi-component process (i.e., amnesia, unconsciousness, analgesia, immobility, attenuation of autonomic response)
- Each useful anesthetic produces the required components via multiple mechanisms - Increase inhibitory and/or decrease excitatory neurotransmission via membrane hyperpolarization and effects on synaptic function |
|
|
What are the likely molecular targets of anesthetics?
|
- GABA-a receptors (GABA-regulated Cl- channels)
- NMDA receptors - Many other channels and membrane associated proteins |
|
|
How are GABA-a channels affected by anesthetics?
|
- Anesthetics increase GABA-a opening via allosteric effects on the receptor protein (not a direct effect on GABA binding)
- Increases Cl- conductance results in hyperpolarization (membrane potential becomes more negative) |
|
|
How are NMDA recetors affected by anesthetics?
|
- Anesthetics that do not interact with GABA receptors (ketamine, nitrous oxide, and xenon) all inhibit NMDA receptors
- Reduced Na+ and Ca2+ influx - Some hyperpolarization of membrane potential |
|
|
How are other membrane-associated proteins affected by anesthetics?
|
- Anesthetics fill hydrophobic cavities in proteins
- Can alter the movement of proteins; alter transitions required for signaling and activation |
|
|
What are the stages of anesthesia?
|
1. Premedication
2. Induction 3. Maintenance |
|
|
What are the goals / characteristics of induction (stage 2) of the stages of anesthesia?
|
- Non-frightening, quick, painless
- Usually IV anesthetic (bolus) or other parental methods - Only pain is in establishing IV line - Emergency - via inhalational anesthetics |
|
|
What kind of anesthetics are used for maintenance (stage 3) of the stages of anesthesia?
|
Gaseous anesthetics because they have shorter half-lives; do not accumulate (allows patient to emerge quickly when it is over)
|
|
|
What are the two ways general anesthetics can be administered?
|
- Parenterally
- Inhalation / Gaseous |
|
|
What are the characteristics of parenterally administered anesthetics?
|
- Hydrophobic
- Intravenous bolus administration (leads to high conc. in brain and spinal cord) - Partition into brain and spinal cord from circulation during one pass --> rapid induction - Redistributes back out of brain as blood levels drop, ends up in other tissues where it is slowly released and metabolized - Half-life in body and duration of action not the same |
|
|
What are the parenteral anesthetics?
|
- Thiopental
- Propofol - Etomidate - Ketamine - Midazolam |
|
|
What is the usefulness and problems associated with Thiopental?
|
- Induction for in-patient surgery
- Hypotension and hangover |
|
|
What is the usefulness and problems associated with Propofol?
|
- Induction / maintenance for out-patient
- Hypotension and respiratory depression |
|
|
What is the usefulness and problems associated with Etomidate?
|
- Induction in patients at risk for hypotension
- Nausea and vomiting, adrenal suppression |
|
|
What is the usefulness and problems associated with Ketamine?
|
- Patients at risk for bronchospasm, peds patients (short procedures)
- Increased intracranial pressure, delirium |
|
|
What is the usefulness and problems associated with Midazolam?
|
- Conscious sedation; anti-anxiety
- Slow induction, respiratory depression |
|
|
What are the commonalities of all inhalational anesthetics?
|
- Very low therapeutic indices (LD50/ED50 can be as low as 2-4)
- Pharmacokinetics are unique and important (gaseous or readily vaporized at room temperature; partial pressure determines transmembrane movement; equilibrium reached when partial pressures are the same) |
|
|
What determines the transmembrane movement of inhalational anesthetics? When is equilibrium reached/
|
- Partial pressure of anesthetics determines movement
- Equilibrium reached when partial pressures are the same (not necessary equivalent to equal concentrations) |
|
|
What are the three important partition coefficients to consider for inhalational anesthetics?
|
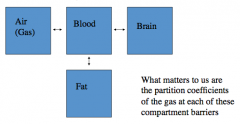
- Blood:Gas
- Brain:Blood - Fat:Blood |
|
|
What does the Blood:Gas partition coefficient determine?
|
- Ease of absorption at alveoli
- Measure of solubility of anesthetic in an aqueous vs. gaseous environment - Low coefficient --> rapid equilibration (fewer molecules are needed to raise partial pressure, but need high amount in air) - Rate of induction and recovery is inverse to blood:gas coefficient |
|
|
What does a low Blood:Gas partition coefficient mean?
|
- Need high amounts in inspired air
- Induction is quick (equilibrium is reached quickly) - Recovery will be quick (drug will move out of blood into gas readily) |
|
|
What does a high Blood:Gas partition coefficient mean?
|
- Need less in inspired air
- Induction and recovery are slow (equilibria are reached slowly) |
|
|
What does the Brain:Blood partition coefficient determine?
|
Anesthetic movement into brain
|
|
|
What does the Fat:Blood partition coefficient determine?
|
- Redistribution from fat and recovery from anesthetic effect
- The higher the coefficient, the longer the half-life and the hang-ver (slow release into blood) |
|
|
What does a high Fat:Blood partition coefficient mean?
|
Half-life will be long (hang-over) due to slow release into blood; enough gets into brain to make patient feel sleepy
|
|
|
What factors affect induction by gaseous anesthetics?
|
- Anesthetic concentration in inspired air
- Pulmonary ventilation - Pulmonary blood flow - Arteriovenous concentration gradient - Elimination (rate of recovery from anesthesia) |
|
|
How does the anesthetic concentration in the inspired air affect the induction of a gaseous anesthetic?
|
- Determines partial pressure of gas in air
- Affects partial pressure in blood - Also affects rate of movement of gas into blood (rapid induction can be achieved w/ higher concentration) |
|
|
How does the pulmonary ventilation (rate of respiration) affect the induction of a gaseous anesthetic?
|
Affects moderately blood soluble anesthetics more than low soluble agents
|
|
|
How does the pulmonary blood flow affect the induction of a gaseous anesthetic?
|
- Increased blood flow slows the rate of rise of arterial partial pressure (shorter time for equilibration)
- More important for moderate than low blood:gas PC |
|
|
How does the arteriovenous concentration gradient affect the induction of a gaseous anesthetic?
|
- Dependent upon rate and extent of tissue uptake
- Determined by partition coefficients between blood and tissue, rate of blood flow to organ or tissue, concentration gradient (relative partial pressures) - During induction, most highly perfused tissues have greatest effect on this parameter |
|
|
How does the elimination (Rate of recovery from aneshtesia) relate to the induction of a gaseous anesthetic?
|
- Reverse of induction - blood:gas partition coefficient is most important determinant (low solubility anesthetics are eliminated faster)
- Duration of exposure: because of tissue accumulation; longer the exposure the longer it takes to eliminate |
|
|
What does the brain partial pressure equal when anesthesia is achieved?
|
MAC = Minimum Alveolar Concentration
|
|
|
What is the relative speed of getting anesthetic into the brain? Why?
|
Relatively fast to get from alveolar gas to brain because brain is well perfused and anesthetics are lipophilic; so brain is anesthetized shortly after MAC is reached in alveoli
|
|
|
Clinically, how do they know when the patient has reached equilibrium?
|
Equilibrium occurs when the concentration of anesthetic in the inspired gas mixture is the same as the end-tidal (alveolar) concentration
|
|
|
How does the lipophilicity affect the rate at which equilibrium is reached for gaseous anesthetics?
|
More slowly for agents that are very fat-soluble; more quickly for agents with less fat solubility
|
|
|
What determines the rate of recovery for agents with low blood and tissue solubility?
|
Recovery is rapid and unrelated to length of anesthetic exposure
|
|
|
What determines the rate of recovery for agents with high blood and tissue solubility?
|
Recovery will be a function of duration of anesthetic administration (because of fat accumulation of anesthetic)
|
|
|
What are the gaseous anesthetics?
|
- Isoflurane
- Desflurane - Sevoflurane - Nitrous Oxide |
|
|
What is the usefulness and problems associated with Isoflurane?
|
- Induction and maintenance; inpatient
- Slower, airway irritant |
|
|
What is the usefulness and problems associated with Desflurane?
|
- Outpatient, maintenance only
- Coughing and bronchospasm |
|
|
What is the usefulness and problems associated with Sevoflurane?
|
- All types, induction and maintenance
- Fluoride ion toxicity |
|
|
What is the usefulness and problems associated with Nitrous Oxide?
|
- Dentistry, adjunct
- Oxygen dilution, abuse |

