![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
142 Cards in this Set
- Front
- Back
|
What are the therapeutic uses of Quinidine and what is its class?
|
Therapeutic Use: PAT, PSVT and Ventricular tachycardia
Quindine is a class Ia drug |
|
|
What are Adverse Effects of Quidinine?
|
Cinchonism, hypotension (alpha-adrenergic blocking effect) and torsades de pointes. Also can cause nausea, vomiting and diarrhea
|
|
|
How is Procainamide metabolized?
|
Dependent on hepatic N-acetyltransferase and renal function. There are rapid(t1/2=2.5-3hrs) and slow(t1/2>5hrs) acetylators.
Also, 70% of procainamide is unchanged in the urine. |
|
|
What are adverse effects of Procainamide?
|
Can cause SLE-like syndromes.
- Arthralgia, pericarditis, fever, weakness, skin lesions, lymphadenopathy, anemia and heptaomegaly Also, causes GI nausea and vomitting, decreased renal functions may be prodysrhythmic, mental confusion and torsade de pointes |
|
|
What is the MoA of Lidocaine and what is its class?
|
Inhibits the reentry mechanisms in ventricular tissue: suppresses spontaneous ventricular depolarizations
|
|
|
What is special about Lidocaine, why would it be used after an MI?
|
Works preferentially to block ischemic tissue and activate normal cardiac tissue
|
|
|
How is lidocaine administered?
|
IV administration only
|
|
|
What class is flecainide and when should it be used?
|
Class Ic. It should be used in the treatment of refractory life-threatening ectopic ventricular dysrhythmias cases because of marked cardiac depression and prominent prodysrhythmic effects
|
|
|
What class is propranolol and what are its effects?
|
Class II. It is a Beta antagonist: Lowers HR/CO (increasing ERP), lowers conduction in Atria, AV nodes and ventricles.
|
|
|
What is propranolol used for?
|
Excellent use for atrial flutter and fibrillation. PAT and digoxin-induced dysrhythmias
|
|
|
What are adverse effects of propranolol?
|
Hypotension, asytole, brochospasm with non-selective antagonists and rebound w/drawal effect due to recepto up-regulation
|
|
|
What do Class III drugs do?
|
Alters K+ flux during phase 3: increase ERP and APD
|
|
|
What class of drug is amiodarone? And how is it useful?
|
Class III.
purported less prodysrhythmic potential. It is useful in refractory ventricular dysrhythmia |
|
|
What are the adverse effects of amiodarone?
|
There is a 75% incidence rate in chronic, oral administration.
GI nausea and vomiting, pulmonary toxicity (10-17% pneumonitis/ARDS), photosensitivity and thyroid disorders/tumors |
|
|
What class of drug is verapamil and how is it used?
|
It is a Class IV drug.
It is used with supraventricular tachycardia, angina and hypertension(need a higher dose for hypertension) |
|
|
What does verapamil do?
|
It is a cardo depressant: decrease HR, SA automaticity and AV conduction, while increasing PR
|
|
|
What do class IV drugs do?
|
Class IV drugs are CCB (ca channel blockers). Affect slow inward Ca channels
|
|
|
How should you use verapamil?
|
If you want a rapid conversion administer it through IV.
If you want to maintain normal rhythms and prevent SVT administer drug orally. |
|
|
Is verapamil lipophilic or hydrophilic? Does that matter?
|
It is lipophilic and can cross the BBB. Hemodialysis is ineffective in the event that you need to remove it.
|
|
|
What are adverse effects of verapamil?
|
GI constipation, hypotension, exacerbate CHF and AV heart block in combination with Beta Blockers
|
|
|
What is adenosine used for?
|
adenosine is comparable to verapamil, but it has a much SHORTER half-life. It is used to convert PAT, PSVT, WPW to NSR.
|
|
|
What is the MoA for adenosine?
|
It hyperpolarizes the membrane by opening K+ channels. It produces a complete AV nodal block--allows heart to "re-set" itself.
|
|
|
How is Adenosine administered?
|
Rapid bolus, close to the heart (brachial vein or jugular)
|
|
|
What is digoxin used to treat?
|
It treats chronic atrial fibrillation (but CCBs are clinically preferred at this time)
|
|
|
What is the MoA of digoxin in CHF?
|
Blocks Na/K ATPase
|
|
|
What is the MoA of digoxin in Atrial Fibrillation?
|
vagal stimulation effect resulting in a neg dromotropic effect at the AV node: prolonged ERP.
Slow ventricular rate by decreasing the number of P-wave depolarizations that reach the ventricles. Sympathetic stimulation may over-ride this effect. |
|
|
What are the adverse effects of Digoxin?
|
highly dysrhythmogenic due to the effects on plasma K+
|
|
|
How can you overcome digoxin-induced ventricular dysrhythmia?
|
Administer MgSO4 therapy: facilitates K+ distribution
Also, ClassIB and Class II agents appear to be affective. |
|
|
How can you manage Bradycardia?
|
Atropine (vagal block to increase HR)
isoproterenol (Beta-1 stimulated increase in HR) Pacemaker (morphologic AV nodal block) |
|
|
How can you manage a Sinus Tachycardia manually?
|
Vagal stimulation through carotid sinus massage or Valsalva maneuver
|
|
|
What causes Heart Failure?
|
MI, chronic untreated hypertension, chronic dysrhythmia, CAD, etc.
|
|
|
What characterizes Heart Failure?
|
Reduction in SV(and CO) at any given end diastolic volume (EDV)
|
|
|
How is the Frank-Starling curve affected by +/- inotropic agents
|
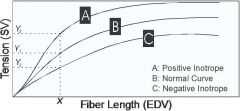
+ inotropic increases contractility, while - inotropic decreases contracility
|
|
|
Low Output congestive heart failure results from what?
|
decreased contractile capacity
|
|
|
What are the three main characteristic symptoms of CHF?
|
ventricular hypertrophy, edema, and weak, rapid pulse(baroreflex activation)
|
|
|
What is the goal of treatment with CHF?
|
The goal is to reverse the three symptoms: ventricular hypertrophy, edema and weak, rapid pulse
|
|
|
Clinical tx of CHF involves what tools?
|
Diet and Na+ restriction
exercise diuretics, AChEIs and vasodilators positive inotropic agents |
|
|
Digoxin (digitalis) is found in what plant?
|
foxglove
|
|
|
Foxglove is classified as what type of agent?
|
Cardiac Glycoside
|
|
|
If a pt is in atrial fibrillation, what drug could you give that would inhibit the Na/K ATPase?
|
Digoxin
|
|
|
If you give Digoxin to your pt, what should you be worried about?
|
prodysrhythmia
|
|
|
What are some side effects that most pts will have with each dose of digoxin?
|
nausea and vomiting caused by CTZ stimulation
|
|
|
What are common side effects of Digoxin?
|
enhanced morbidity/mortality when combined with diuretics (depletes the K+)
dysrhythmia, visual and neurological disturbances |
|
|
Why does digoxin cause nausea and vomiting?
|
It stimulates the CTZ
|
|
|
When you give digoxin to your pt, what should you always monitor?
|
Electrolytes! Changes in K+ and Ca++ may lead to dysrhythmias
|
|
|
Why does inhibiting Na/K ATPase cause greater contracitlity?
|
The increase in intracellular NA causes an increase in Na/Ca exchange: More Ca++ is available for muscle fiber contraction.
|
|
|
How can you correct for too much plasma digoxin?
|
Administer Cholestyramine or digoxin immune Fab (binds to the free and bound cardiac glycoside where it is sequestered in extracellular fluid: renally eliminated.
|
|
|
If you eliminate Digoxin, will there be lasting clinical effects?
|
No
|
|
|
What is the method of action for Isoproterenol?
|
Beta-1 receptor: mediates increases in intracellular cAMP = elevations in Ca++
Increases membrane excitation and contraction |
|
|
What does isoproterenol do?
|
It increases both the contracility and heart rate
|
|
|
Should isoproterenol be used in preventive settings?
|
No, it should only be used in acute situations
|
|
|
What is the MoA of dopamine?
|
It is an adrenergic agonist on peripheral receptors.
|
|
|
Does Dopamine have different effects at different doses? What are those effects?
|
Yes.
Low Dose: stimulates DA1 and DA2 receptors= vasodilation, especially in the renal bed (increase GFR, Urine output) Moderate Dose: additional stimulation of Beta 1 receptors: increase contraction and slight increase in HR High dose: additional stimulation of alpha 1 receptors causes peripheral vasoconstriction. |
|
|
Is Dopamine's metabolism slow or fast?
|
Rapid action onset and metabolism by MAO/COMT
|
|
|
When should you give Dobutamine?
|
Use with short term management of heart failure following MI.
|
|
|
How is dobutamine different from Dopamine?
|
Dobutamine has a preferential increase in cardiac contractility w/o increasing HR
|
|
|
Dobutamine's MoA is what?
|
Less Alpha 1 effects and less Beta1 tachycardia
|
|
|
How should you administer Dobutamine?
|
continuous, short-term IV infusion. It will be eliminated by COMT and has a half life of 2 minutes.
|
|
|
Name two phosphodiesterase inhibitors?
|
Inamrinone and milrinone
|
|
|
What does phosphodiesterases do?
|
Metabolize cAMP
|
|
|
What is the result of inhibiting phosphodiesterases
|
results in elevated intracellular cAMP and ensuing increase in intracellular Ca++
|
|
|
What is a phosphodiesterase inhibitor similar to?
|
Beta 1 agonists
|
|
|
When should you use phosphodiesterase inhibitors and what method of administration?
|
You should it in acute settings only and with an IV administration.
|
|
|
Where is the baroreflex and how is that info transmitted to the brain?
|
Carotid sinus is the location and glossopharyngeal nerve transmits the information to the brain.
|
|
|
What is essential hypertension?
|
no clear cause or mechanism has been discovered for causing the hypertension.
clear genetic basis and usually found in middle age adults. |
|
|
What is secondary/non-essential hypertension?
|
small number of adults who have hypertension for a specific reason: tumor, renal disease, etc.
They usually require surgery to adjust their blood pressure |
|
|
How do you dx hypertension?
|
two or more readings with at least 4 wks apart.
|
|
|
What are "normal" values of blood pressure?
|
AHA: <140/90
WHO: <160/90 |
|
|
Does hypertension require medical intervention?
|
Yes--due to the pathological consequences.
|
|
|
Treatment of hypertension depends on what qualities?
|
Age, ethnicity, body-type, obesity, personality type
athletic/sedentary etiology of HTN rapidity of onset and severity presence of other CV risks |
|
|
What is the first line of defense in HTN Tx?
|
Modifications in lifestyle!
(lose weight, limit alcohol, increase activity, reduce NA+ <100mmol/6grams, maintain K+ 7grams, maintain Ca and Mg intake, stop smoking |
|
|
What should you consider when deciding to put your pt on HTN drugs?
|
Cost to pt
life-long ordeal (usually) dosage/drug class & side effects pt compliance ALWAYS consider Step-Care Therapy |
|
|
What must you consider with each drug for hypertension?
|
the Baroreceptor reflex
|
|
|
How will the baroreceptor reflex work?
|
retains Na and H2O by the kidneys
increases peripheral vascular resistance, HR and CO (all sympathetically) |
|
|
How do antihypertensives work?
|
MAP = CO x TPR
CO = HR x SV |
|
|
Name some diuretics
|
Thiazides, loop diuretics, K+ sparing diuretics
|
|
|
How do diuretics work?
|
relatively unknown
May be due to a decrease in blood volume causing a decrease in CO |
|
|
How effective are diuretics?
|
Have moderate monotherapy efficacy (20/10)
But augments antihypertensive effects of other drugs. |
|
|
What population has better efficacy with diuretics?
|
African-Americans and eldery pts.
|
|
|
How long does it take for diuretics to work?
|
2-4wks, but their peak effect in 3-4 months
|
|
|
Does increasing the dose of diuretics increase the efficacy?
|
No, it does increase the severity of the side effects
|
|
|
What are contraindications of diuretics?
|
hyperlipidemia (elevates LDL and TG) and diabetes (may induce hyperglycemia)
|
|
|
How does propranolol (Beta antagonists) help with HTN?
|
Blocks Beta-Receptors:
In the heart: Decrease HR/contractility => decrease BP In the Kidney: Decrease renin release => Ang II formation |
|
|
What is the efficacy of Beta-blockers with HTN?
|
moderately good in monotherapy, but better in combination therapy
|
|
|
Is there a population that responds poorly to beta-blocker therapy with HTN?
|
smokers
|
|
|
What are the side effects of Beta blockers?
|
hyperlipidema, male sexual dysfunction, exacerbates asthma and CHF.
Diabetes: masks signs of hypoglycemia (dysrhythmia, tachycardia, tremor, diaphoresis) and could lead to coma or death |
|
|
What is a good drug to lower HTN in the presence of CHF? Why?
|
Labetalol and carvedilol.
Block, Beta 1 and Beta 2, but also blocks alpha 1. This results in an vasodilation (which will decrease the afterload) |
|
|
What drug should you use in HTN emergencies?
|
labetalol (IV only)
|
|
|
What is the method of action with Clonidine?
|
post-synaptic alpha 2 agonist in CNS: inhibits sympathetic outflow resulting in decrease HR/TPR
Pre-synaptic alpha 2 agonist in the periphery: decrease NE release from post-ganglionic nerve terminals |
|
|
What is the efficacy of clonidine?
|
35/20 monotherapy (combination with a diuretic is common)
|
|
|
How does alpha-methyldopa work?
|
It is a centrally- acting sympatholytic.
Analog of DOPA, which is converted in CNS neurons to alpha-methylnorepinephrine. Stimulates inhibitory alpha 2 receptors--acts as a false transmitter |
|
|
Your 30 year old female pt with chronic HTN needs to try drug therapy--which drug would you use?
|
alpha-methyldopa
|
|
|
What could be some side effects of alpha-methyldopa?
|
positive direct Coombs test:
presence of auto-antibodies in RBCs. This could result in frank hemolytic anemia Also there is prominent sexual dysfunction, dry mouth and sedation. |
|
|
What are some peripherially acting sympatholytics?
|
Prazosin, terazosin, doxazosin
|
|
|
-zosin drugs act on what receptor?
|
alpha 1 antagonist--they spare alpha 2(NE is not released)
|
|
|
If you pt come into the office with HTN and you give them a -zosin drug--what might you expect as a pleasant side effect?
|
lowering of the LDL, TG and total cholestrol.
|
|
|
What would be some adverse effects of -zosin drugs?
|
mild reflex tachycardia
|
|
|
What is the efficacy of -zosin drugs?
|
15/10 monotherapy and 25/15 with diuretic
|
|
|
Verapamil can be used to treat supraventricular tachycardias with the heart...what else can verapamil and diltiazem be used to treat?
|
HTN: It is a CCB which acts on the periphery to inhibit Ca release from the vascular smooth muscle and from the SR.
This causes direct vasodilation |
|
|
What are the side effects and the effecacy of treating HTN with Verapamil?
|
Side effects: cardio depressant--which may counter with a reflex tachycardia
efficacy: 30/20 |
|
|
What is the efficacy of diltiazem in treating HTN?
|
20/15
|
|
|
How does nifedipine work?
|
It is a CCB (dihydropyridine)
|
|
|
Do you give nifedipine alone or with another drug? and why?
|
Give with a beta blocker b/c of the prominent reflex tachycardia
|
|
|
Which has better efficacy with treating HTN?
verapamil diltiazem nifedipine |
nifedipine
|
|
|
What is the method of action with Hydralazine?
|
direct vasodilation via cGMP.
increases intracellular cGMP increase Ca sequestration (smooth muscle relaxant) large effect on afterload with little effect on preload |
|
|
When would you want to use hydralazine?
|
Because of the decrease in afterload, but little effect on pre-load you would use Hydralazine with CHF
(but recently it has been replaced with ACE inhibitors) |
|
|
What is negative about using hydralazine as a long term drug?
|
It developes tachyphylaxis due to prominent baroreflex perturbation
|
|
|
How could you prevent the tachphylaxis of hydralazine?
|
Give with a beta-blocker and diuretic
|
|
|
What are some adverse effects of hydralazine?
|
SLE-like syndrome
palpitation, tachcardia use limited to resistant, fulminant hypertension and management of hypertensive emergency |
|
|
If you have a hypertensive emergency in a CHF pt, what drugs should you consider?
|
hydralazine
|
|
|
IF you have a hypertensive emergency in a p, what drugs should you consider?
|
labetalol
|
|
|
What drug would you use for severe, refractory hypertension?
|
Minoxidil
|
|
|
What is the MoA of minoxidil?
|
direct arteriolar vasodilation: stimulation of vascular smooth muscle K+ channel opening (results in membrane hyperpolariztion)
|
|
|
What is a side effect of minoxidil?
|
Tachyphylaxis (baroreflex mediated)
|
|
|
What other drugs should you prescribe with minoxidil?
|
Beta-blockers and diuretics
|
|
|
what is the danger with sodium nitroprusside?
|
extended continuous infusion may produce methemoglobinemia, cyanide poisoning and cell death.
|
|
|
What is the MoA of sodium nitroprusside?
|
Donates NO to cGMP mediated Ca sequestration.
It decreases BOTH after load and preload |
|
|
When and how would you use sodium nitroprusside?
|
Parenterally infused agent used in hypertensive emergencies and the rapid management of CHF
|
|
|
Name a few ACE inhibitors
|
enalapril, captopril and linsinopril
|
|
|
What is the efficacy of ACE inhibitors with monotherapy?
|
25/30
|
|
|
When is the maximium effect of ACE inhibitors occur?
|
4-8wks after dosing
|
|
|
Why would someone want to be removed from ACE inhibitor therapy?
|
They develop a dry, peristent cough
|
|
|
What group of people don't respond as well to ACE inhibitors?
|
african americans
|
|
|
What is the efficacy of ACE inhibitors?
|
25/20
|
|
|
When should you NEVER use Ace inhibitors?
|
in pregnant women
|
|
|
Why should you not use ACE inhibitors in pregnant women?
|
ACE inhibitors can cross the placenta and cause neuronal defects
|
|
|
What is ANG receptor blocker MoA?
|
specific antagonist of ANG II at AT1 receptor on vascular smooth muscle.
|
|
|
Is losartan okay to use in pregnancy?
|
NO. it is an ANG receptor blocker.
|
|
|
What are some names of ANG receptor blockers?
|
Candesartan, losartan, irbesartan, valsartan
---sartan |
|
|
When does ischemia occur?
|
when the work-load is greater than the oxygen supply
|
|
|
How can you improve angina pain?
|
improve oxygen (blood) delivery
decrease workload of the myocardium |
|
|
What is the Steal Phenomenon?
|
the small vessel are already maximally dilated in chronic ischemic states (reactive hyperemia), so vasodilators do not improve the pt condition by producing coronary vessel dilation
They may direct blood flow to non-ischemic areas by dilating larger distal vessels |
|
|
What are good vasodilators to use in angina?
|
non-endothelium-dependent:
NO-donators providing their own EDRF (endothelium-derived relaxing factor) |
|
|
What role does sodium nitroprusside play in tx of angina?
|
use in emergency parenteral use only
reduce BOTH preload and afterload |
|
|
What is the MoA with nitroglycerin?
|
NO stimulated increase in cGMP: Ca sequestration and vasodilation (preload and afterload)
|
|
|
What can be a danger with Nitroglycerin?
|
tachyphylaxis
|
|
|
What is the fastest onset of action dose with nitroglycerin?
|
sublingal (1-3 minutes), but some people have psychological relief within seconds
|
|
|
What are some adverse effects of nitroglycerin?
|
flushing of soft tissues and headache and sublingal burning sensation
headache and flushing pt will develop a tolerance |
|
|
What is EDRF?
|
it is a soluble gas produced by vascular endothelial cells.
produces a potent cGMP-mediated vasodilation |
|
|
How are EDRF and angina possibly related?
|
perhaps underproduction of EDRF could cause angina
|
|
|
What is Endothelin?
|
peptide produced by vascular endothelial cells that produce a potent receptor-mediated (ETa) vasoconstriction
|
|
|
How are Endothelin and angina, vasospasm and hypertension possibly related?
|
An overproduction of endothelin may cause angina, vasospasms or hypertension.
|

