![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
43 Cards in this Set
- Front
- Back
|
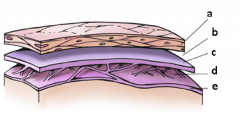
a = dura mater b = sub-dural space c = arachnoid d = sub-arachnoid space e = pia mater |
|
|
what are the layers that make up the meninges? |
dura mater arachnoid pia mater |
|
|
where do nutrients come from that supply the brain tissue? |
sub-arachnoid space (contains CSF which contains nutrients) |
|
|
CNS infection may include: |
meningitis encephalitis meningoencephalitis brain abscess subdural empyema epidural abscess ventriculo-peritoneal shunt infections |
|
|
meningitis defn |
inflammation of the membranes of the brain and spinal cord Specifically, inflammatory changes in the cerebrospinal fluid between the pia and the arachnoid membranes of the meninges |
|
|
CSF |
fluid - clear yellowish/beige (not completely white) -contains water, sodium, potassium, some protein, a few WBCs, glucose pH = 7.4 |
|
|
mortality of meningitis |
5-25%
eradication of bacteria is essential for improved outcome BUT is only one of the variables involved in mortality |
|
|
50% of Pts w meningitis have what other condition? |
persistent neurological disabilities -seizures -hearing loss |
|
|
what age group is mostly affected by meningitis? |
primarily a disease of the young, and adults with risk facors 75% incidence in children < 15 yrs 35% incidence in children < 1 yr |
|
|
what are the 3 routes of meningitis infection? |
Hematogenous Contiguous Direct inoculation |
|
|
Hematogenous route of meningitis infection |
Pts develop meningitis following systemic bacteremia as with endocarditis (infection of heart valve - into blood)
|
|
|
Contiguous route of meningitis infection |
most cases occur when colonization by potential pathogen is followed by mucosal invasion of the nasopharynx -infection in tissues surrounding brain tissue (sinuses, upper resp infection, otitis media) then spread to brain |
|
|
direct inoculation route of meningitis infection |
some pts develop disease by direct extension of bacteria across a skull fracture with subsequent leak into CSF -related to trauma |
|
|
etiology of aseptic meningitis |
fungal viral rickettsiae spirchetes protozoa |
|
|
etiology of septic meningitis |
bacterial |
|
|
etiology of non-infectious meningitis |
NSAIDs invasive procedures |
|
|
viral meningitis |
-less severe than bacteria -most people usually get better on their own within 7-10d (w/o Tx), however infants < 1mth and pts w weak immune system are more likely to have severe illness |
|
|
causes of viral meningitis |
-non-polio enteroviruses are most common (especially from summer to fall) however, only small number of people who get infected with enterovirus develop meningitis -mumps virus -herpesvirus (including Epstein-Barr, herpes simplex, varicella zoster) -measles virus -influenza virus -arbovirus (such as West Nile Virus) -lymphocytic choriomeningitis virus |
|
|
causes of bacterial meningitis (septic) |
these represent 80% of all causative organisms: -S. pneumoniae -N. meningitidis (6 & 12 serogroups cause epidemics) -H influenza
-all 3 have capsule - hard for immune system to engulf as macrophages and present (complement system used to help engulf) -pts who have had splenectomy are at higher risk, as well as HIV, chemotherapy, very young |
|
|
etiology of meningitis in neonates (<1mth) |
usually infected by bacteria found in birth canal at time of parturition -risk factors include: early rupture of membranes, low birth wt, immature immune system, immature BBB
organisms: -Group B streptococci -Listeria monocytogenes -E coli and other G(-) bacilli |
|
|
etiology of meningitis in children and young adults |
risk factors for children: inexperienced immune system, daycare, URTI
risk factors for adults: spleenectomy, complement deficiency, travel (eg sub-Saharan Africa or annual Hajj pilgrimage)
Organisms: -streptococcus pneumoniae -Neisseria meningitidis |
|
|
etiology of meningitis is adults (>50) or immunocompromised (HIV, alcoholism, debilitating illness, pregnancy) |
risk factors include: decreased immunity
organisms: -S pneumoniae -L monocytogenes - Gram negative bacilli -N meningitidis |
|
|
etiology of meningitis in open head trauma, post-operative, or CSF Shunt Infection |
risk factors: -barrier breakdown -contamination from surgery or injury -foreign indwelling device
organisms: -S aureus -S epidermis -gram negative bacilli |
|
|
etiology of meningitis in close-head trauma w skull fracture |
risk factors include: -no barrier breakdown
organisms: -S pneumoniae -H influenza -S pyogenes
through hematogenous spread of infection - haven't formed bone structure or immune system properly, etc (usually in kids w malformations) |
|
|
empiric therapy for meningitis |
early diagnosis is key! empiric therapy req'd until C&S data available -consider age and risk factors empiric therapy is broad and aggressive -combination therapy may be required based on suspected organisms PK factors are key -natural barriers and Abx propertie determine CSF penetration of ABx |
|
|
barriers to antibiotic preparation for meningitis |
BBB = tightly joined capillary epithelial cells, drug must penetrate endothelial cells and glial cells -when inflamed, can get up to 50% penetration rate (when not inflamed, 10-20%)
small drugs to penetrate through tight junctions (vanco and clinda too large) and be lipophilic (aminoglycosides very polar so not good) low protein binding -more free drug
|
|
|
empiric therapy for meningitis in neonates |
duration: 14-21 d
ampicillin + cefotaxime or ampicilin + gentamicin |
|
|
empiric therapy for meningitis in 1mth - young adults |
duration: 10d
cefotaxime or ceftriaxone or meropenem PLUS vancomycin |
|
|
empiric therapy for meningitis in adults (>50) or immunocompromised |
duration: strep pneumo: 10-14d neisseria: 5-7d listeria: 21d
cefotaxime or ceftriaxone or meropenem PLUS ampicillin PLUS vancomycin
vancomycin PLUS SMX/TMP (for severe beta-lactam allergy)
* can d/c vanco if susceptible to cephs |
|
|
empiric therapy for meningitis in open head trauma, post-operative |
duration: 10-14d
meropenem or ceftazidime or cefipime PLUS vanco |
|
|
empiric therapy for meningitis in CSF shunt infection |
duration: 14 d after shunt removal
cefotaxime or ceftriaxone PLUS vanco +/- rifampin |
|
|
empiric therapy for meningitis in closed trauma w fracture |
duration: 10-14d
cefotaxime or ceftriaxone PLUS vanco |
|
|
dosing for ceftriaxone in meningitis |
2g IV q12h |
|
|
dosing for cefotaxime in meningitis |
2g IV q4-6h |
|
|
dosing for vancomycin in meningitis |
15mg/kg IV q8-12h (aim for troughs 15-20mg/L) |
|
|
dosing for meropenem in meningitis |
2g IV q8h |
|
|
dosing for ampicillin in meningitis |
2g IV q4h |
|
|
dosing for TMP in meningitis |
15-20mg/kg/d (div q6-8h) |
|
|
when do you use chemoprophylaxis for meningitis? |
to prevent spread of meningococcal and haemophilus meningits but NOT for pneumococcal disease
to prevent development of disease in close contacts and to eradicate pharyngeal carriage |
|
|
chemoprophylaxis regimen for Neisseira meningitis |
rifampin 600mg po bid x 4 doses (2 days)
ciprofloxacin 500mg single dose |
|
|
chemoprophylaxis regiment for Hemophilus meningitis |
rifampin 600mg po daily x 4 days |
|
|
corticosteroid use for meningitis |
-dexamethasone prior to ABxs has some role for specific pathogens, age, severity of presentation -CSs have been shown to decrease mortality and hearing loss in adult pts w S. pneumo menigntis, children >6wks |
|
|
dexamethasone dose for meningitis |
0.15mg/kg iv q6h (max 10mg/dose) x 2-4d
give 20 min before ABx or with first dose but NOT AFTER
usually don't use CS |

