![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
37 Cards in this Set
- Front
- Back
|
Layers of arteries |
Tunica intima: Endothelial cells and subendothelial connective tissue Tunica media: Smooth muscle cells in concentric layers with outer elastic membrane
Tunica adventitia: Connective tissue in wich nerve fibers and vasculature (vasa vasorum) runs |
|
|
Pathophysiological processes affecting vasculature
|
(1) atherosclerosis
(2) aneurysm (3) embolism (4) thrombosis (5) inflammation (6) trauma (7) vasospasm (8) arteriovenous fistula |
|
|
Laplaces law |
Tension = pressure X radius |
|
|
Mechanisms whereby aneurysms cause symptoms |
(1) rupture with subsequent hemorrhage (2) impingement on adjacent structures (4) embolism from mural thrombus (5) Presentation as a pulsatile mass |
|
|
Embolism
|
Clot or foreign body carried by blood to site distant from its point of origin
|
|
|
Types of Emboli |
(1) Thromboemoblism - most commonly cardiac (2) Atheroemboli - from proximal atherosclerotic plaques (3) Septic emboli (4) Malignant emboli (5) Venous (paradoxical) emboli (6) Foreign body emboli (e.g. Air) (7) Fat embolism |
|
|
Thrombosis |
in situ formation of a blood clot within the |
|
|
Causes of arterial thrombosis |
(1) Atherosclerosis (2) Vasculitis (3) Trauma |
|
|
Risk factors of peripheral arterial disease |
Related to atherosclerosis - Smoking - HTN - Hypercholesterolemia - DM
Non-related to atherosclerosis - IVDU - Prior trauma/surgery - History of PE - History of phlebitis - Autoimmune disease - Prior coagulation abnormalities - |
|
|
5p's of acute arterial occlusion
|
Pain Pallor Pulselessness Parasthesias Paralysis |
|
|
Overview of management of acute arterial occlusion |
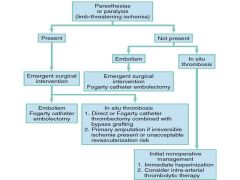
|
|
|
Patterns of pain with chronic arterial insufficency |
(1) Intermittent activity related claudication (2) Ischemic rest pain that improves with standing |
|
|
Buerger's sign |
Pallor with elevation of legs to 45 degrees that resolves to cyanosis then hyperemia with dangling |
|
|
ABI interpretation |
>1.3 Non compressible 0.9 - 1.3 Normal <0.9 Abnormal <0.5 Severe |
|
|
Differentiating emboli versus thrombus on acute PAD |
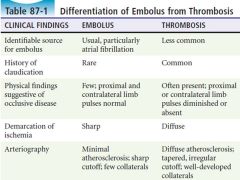
|
|
|
Raynaud's triphasic colors |
Pallor (white) Cyanosis (blue) Rubor (red) |
|
|
Indications for emergency angiography |
(1) acute arterial embolus or thrombosis if the clinical diagnosis is uncertain
(2) consideration of emergency vascular bypass grafting
(3) characterization of vascular abnormality before emergency surgical correction |
|
|
Vascular graft complications |
Stenosis Thrombosis False Aneurysm Infection |
|
|
Arterial Ulcers
|
Vasculopath
Moderate to severe pain that increases with elevation/activity and decreased by dependency Between toes/tips of toes Over phalangeal heads Around lateral malleolus At sites subjected to trauma Well demarcated, punched out, pale or white base |
|
|
Venous ulcers |
History of venous disease, obesity, advanced age
Mild to moderate pain that improves with elevation
On medial/lower calf and ankle
Rapidly progressive, with irregular borders, granulation, exudative, weeping
|
|
|
Diabetic ulcer |
Diabetic/peripheral neuropathy
Little to no pain
Pressure sites, heel, plantar surface
Deep and penetrating, often with secondary damage due to infection |
|
|
Hypertensive ulcer |
Red, very painful, ischemic lower extremity ulcers |
|
|
Buerger’s Disease (Thromboangiitis Obliterans) |
idiopathic inflammatory occlusive disease primarily involving the medium-sized and small arteries of the hands and feet
Males 20 - 40 years, heavy smokers |
|
|
phlebitis migrans |
painful, tender, reddened, or dark nodules over a peripheral artery with either a reduced or an absent pulse |
|
|
Clinical criteria for Buerger's disease |
(1) a history of smoking (2) onset before the age of 50 (3) infrapopliteal arterial occlusive lesions (4) either upper limb involvement or phlebitis (5) absence of atherosclerotic risk factors other than smoking |
|
|
Primary risk of central aneurysms (abdominal aorta, iliac, visceral) |
Rupture |
|
|
Primary risk of peripheral aneurysm |
Thombosis Embolism |
|
|
Most common causes of peripheral aneurysms by location |
Lower extremity: - atherosclerotic
Upper extremity aneurysms - lower trauma Visceral aneurysms - abnormal hemodynamics - infections |
|
|
Clinical characteristics of infected aneurysms |
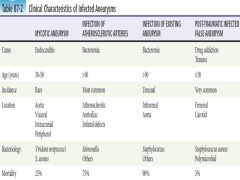
|
|
|
Diagnostic criteria for Raynaud's disease |
(1) precipitated by cold or emotion (2) symptoms are bilateral (3) gangrene is absent/minimal and confined to the skin (4) no disease or condition that could cause a secondary Raynaud’s phenomenon is present (5) occurring for at least 2 years |
|
|
Rayaud's phenomenon |
Raynaud's occuring secondary to an autoimmune cause |
|
|
Overview of thoracic outlet syndrome |

|
|
|
Physical Exam to elicit thoracic outlet syndrome |
Elevated arm stress test (EAST/Roos test) |
|
|
DDx of occluded indwelling catheter |
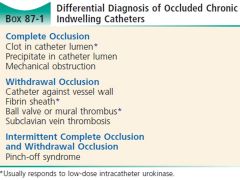
|
|
|
Rosen's approach to an occluded catheter |

|
|
|
Thoracic outlet syndrome |
Compression of the (1) brachial plexus, (2) subclavian artery, or (3) subclavian vein at the superior aperture of the thorax |
|
|
Indications for arteriography in thoracic outlet syndrome |
- obliteration of radial pulse on EAST - Blood pressure differential of 20mm between limbs - possible subclavian stenosis or aneurysm (supraclavicular bruit/pulsation) - peripheral emboli in UE |

