![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
137 Cards in this Set
- Front
- Back
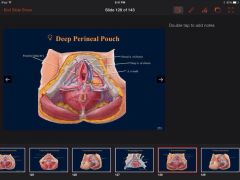
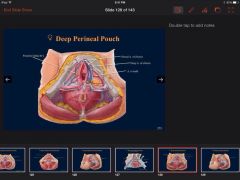
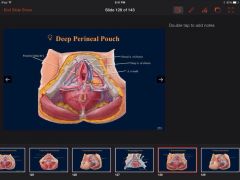
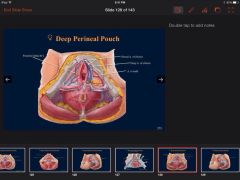
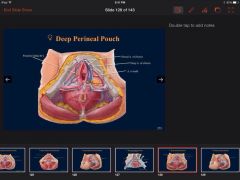
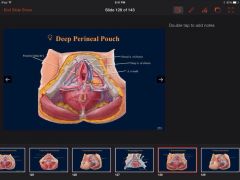
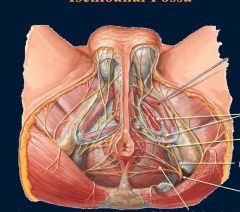
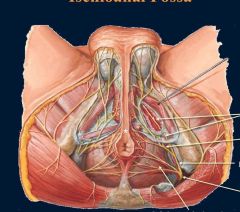
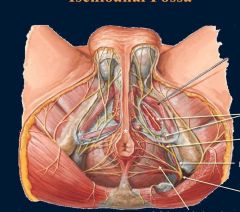
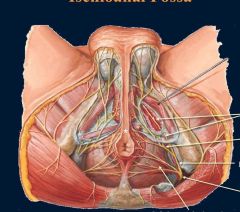
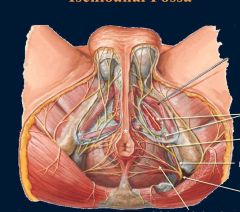
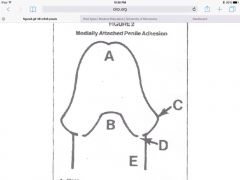
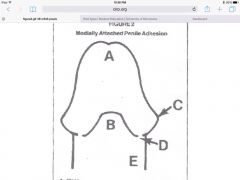
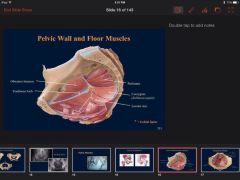
Describe and label the contents of the female deep perineal pouch? Label the pick for nerve?
|
Contents of Female Deep Perineal Pouch:
a. Part of urethra b. Part of vagina c. Sphincter urethrae d. Deep transverse perineal muscles e. Internal pudendal vessels, arterial branches: • Posterior labial branches • Artery to the bulb • Deep artery of the clitoris • Dorsal artery of the clitoris f. Dorsal nerves of the clitoris (of pudendal n.) • Supplies skin of clitoris |
|
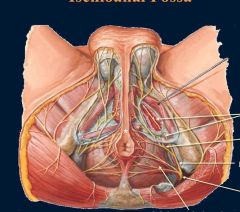
Describe and name the contents of the female superficial perineal pouch? Label structures on picture?
|
Contents of Female Superficial Perineal Pouch:
a. Root of clitoris (i.e. the bulb and crura) b. Muscles covering the bulb and crura: • Bulbospongiosus muscles o Cover bulb of the vestibule and greater vestibular glands o Compress deep dorsal vein of clitoris & weakly constrict vagina • Ischiocavernosus muscles (assist in erection) c. Greater vestibular glands • Open into vestibule, posterolateral to vaginal orifice • Secrete lubricating mucus during sexual arousal d. Lesser vestibular glands (Paraurethral) • Correspond to male’s prostate • Open into vestibule, lateral to urethral orifice • Secrete mucus into vestibule, for distribution to labia & vestibule e. Superficial transverse perineal muscles f. Perineal body g. Perineal branches of pudendal nerve |
|
|
Describe genital mutilation?
|
|
|
|
Draw out the fascia made simpler slide showing you how the names of fascia changes as you move through the body?
|
|
|
|
Explain a episiotomy?
|
An episiotomy also known as perineotomy, is a planned, surgical incision on the perineum and the posterior vaginal wall during second stage of labor. The incision, which can be done at a 90 degree angle from the vulva towards the anus or at an angle from the posterior end of the vulva (medio-lateral episiotomy), is performed under local anesthetic (pudendal anesthesia), and is sutured closed after delivery. It is one of the most common medical procedures performed on women. Vaginal tears can occur during childbirth, most often at the vaginal opening as the baby's head passes through, especially if the baby descends quickly. Tears can involve the perineal skin or extend to the muscles and the anal sphincter and anus. The midwife or obstetrician may decide to make a surgical cut to the perineum with scissors or a scalpel to make the baby's birth easier and prevent severe tears that can be difficult to repair.
|
|
|
Explain a uterine prolapse?
|
Uterine prolapse occurs when pelvic floor muscles and ligaments stretch and weaken, providing inadequate support for the uterus. The uterus then slips down into or protrudes out of the vagina.
Uterine prolapse can happen to women of any age, but it often affects postmenopausal women who've had one or more vaginal deliveries. Damage to supportive tissues during pregnancy and childbirth, effects of gravity, loss of estrogen, and repeated straining over the years all can weaken your pelvic floor and lead to uterine prolapse. |
|
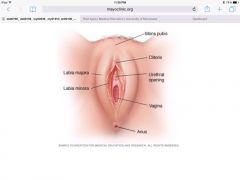
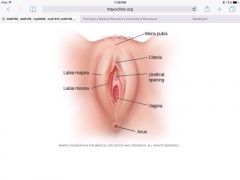
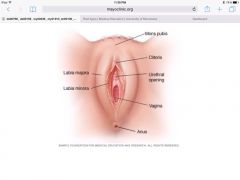
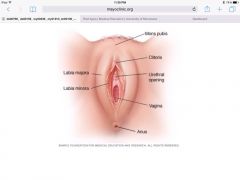
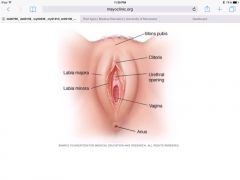
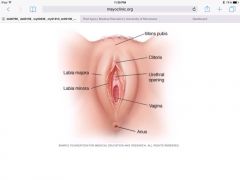
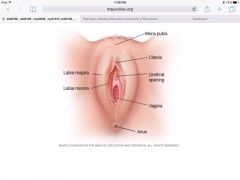
Explain and descibe the structures of the Female UG? Identify the structures that are folds of external skin?
|
Labia – folds of external skin
• Labia majora o = prominent folds of skin, providing protection o Filled with fat, smooth muscle, and terminal part of round ligament • Labia minora o = folds of skin, medial to labia majora o Form the prepuce & frenulum o Vestibule = space between labia minora, containing the external meati of the urethra, vagina, and ducts of the greater and lesser vestibular glands Clitoris • Root o = attached portion in superficial perineal pouch o 3 masses of erectile tissue (covered with muscles): -Bulb of the vestibule – homologous with bulb of penis and corpus spongiosum; divided into 2 parts, surrounding vaginal and urethral orifice, but unite within the glans -R & L crura – attach to pubic arch and become the corpora cavernosa • Body o = proximal detached portion of clitoris (glans is head) o 3 masses of erectile tissue: 2 corpora cavernosa & 1 slender erectile body from the bulb (formed by the uniting of the halves of the bulb of the vestibule) |
|
Explain and name the contents of the male deep perineal pouch? label the appropriate nerve? also name function of each part you name?
|
Contents of Male Deep Perineal Pouch:
a. Intermediate urethra b. Sphincter urethrae (external sphincter of the urethra) • Muscle surrounding urethra • Voluntary innervation, by perineal branch of the pudendal n. c. Bulbourethral glands (formerly Cowper’s) • Glands posterolateral to intermediate urethra and sphincter urethrae • Ducts extend into superficial perineal pouch to enter spongy urethra • Produces pre-ejaculate, lubricating urethra for sperm d. Deep transverse perineal muscle • Tiny! Posterior to sphincter urethrae • Extends from ischial rami to perineal body e. Dorsal nerve of the penis (of pudendal n.) • Supplies skin of penis and glans penis f. Internal pudendal vessels, the arterial branches are: • Artery to bulb of penis (supplies posterior corpus spongiosum and bulbourethral gland) • Deep arteries of the penis (fill crura and corpora cavernosa with blood; aids in erection) o Helicine branches – open into cavernous spaces, coiled arteries in flaccid penis • Dorsal arteries of the penis (supply fibrous tissue around corpora and penile skin) |
|
|
Explain extravasation of fluid into superficial and deep perineal spaces?
|
An injury to the urethra leaving Buck's fascia intact results in a collection of urine (extravasation) limited to the penis, deep to Buck's fascia. However, if the injury to the bulb of the penis results in urethral injury accompanying a tear of the Buck's fascia, then extravasated blood and urine would accumulate in the superficial perineal space, passing into the penis (outer to Buck's fascia) as well as the scrotum and lower anterior abdominal wall. Extravasation of urine involving a compromised Buck's fascia can be appreciated clinically by blood collecting in the superficial pouch, resulting in a 'butterfly'-shaped region around the penis.
|
|
|
Explain female circumcision?
|
Female genital mutilation (FGM), also known as female genital cutting and female circumcision, is the ritual removal of some or all of the external female genitalia. Typically carried out by a traditional circumciser with a blade or razor, with or without anaesthesia,
|
|
|
Explain male cicumcision?
|
Circumcision is the surgical removal of the skin covering the tip of the penis. Circumcision is fairly common for newborn boys in certain parts of the world, including the United States. Circumcision after the newborn period is possible, but it's a more complex procedure.
For some families, circumcision is a religious ritual. Circumcision can also be a matter of family tradition, personal hygiene or preventive health care. For others, however, circumcision seems unnecessary or disfiguring. After circumcision, it isn't generally possible to re-create the appearance of an uncircumcised penis. |
|
|
Explain phimosis?
|
Phimosis (/fɪˈmoʊsɨs/ or /faɪˈmoʊsɨs/[1][2]), from the Greek phimos (φῑμός ["muzzle"]), is a condition in males where the foreskin cannot be fully retracted over the glans penis. The term may also refer to clitoral phimosis in women, whereby the clitoral hood cannot be retracted, limiting exposure of the glans clitoridis.[3]
At birth, the foreskin is fused to the glans and is not retractable. Huntley et al. state that "non-retractability can be considered normal for males up to and including adolescence."[4] Normal developmental non-retractability does not cause any problems. Phimosis is deemed pathological when it causes problems, such as difficulty urinating or performing common sexual functions. There are numerous causes of so-called pathological phimosis. Common treatments include steroid creams, manual stretching, changing masturbation habits, preputioplasty, and circumcision. |
|
|
Explain sexual function in males? 3 stages?
|
|
|
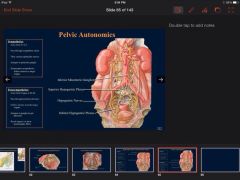
Explain the autonomic innervatin for the pelvis? general plan? where do they arrise from? synapse points? Label the points?
|
Autonomics
1. Sympathetics a. usually 4 ganglia bilaterally on anterior sacrum, converge at ganglion impar (end of sympathetic trunk) b. General Plan (sympathetics simplified…) • arise from T11-L2 spinal segments • Pass through sympathetic chain • Then through lumbar and sacral splanchnic nerves • Synapse in inferior mesenteric ganglion • Postsynaptics travel through superior hypogastric plexus, R/L hypogastric nerves, and/or the inferior hypogastric (pelvic) plexus • Follow pelvic arteries to target organs 2. Parasympathetics a. General Plan • Parasympathetics arise from S2-S4 (pelvic splanchnics) • Ascend mainly through inferior and superior hypogastric plexuses • Follow arteries to target organs • Synapse in ganglia in organ/gut plexuses • Reach targets via short postsynaptic fibers |
|

Explain the branching of just the anterior division of the internal iliac? Label them?
|

Common Iliac A’s
1. Internal Iliac a. Anterior Division • Umbilical o Superior vesicular - Artery to ductus deferens (variable) • Obturator • Inferior vesicular • Middle rectal • Internal pudendal • Inferior gluteal • Uterine o Vaginal |
|

Explain the branching of just the posterior division of the internal iliac? Label them?
|

Posterior Division
• Iliolumbar • Lateral sacral • Superior gluteal – extremely variable (sometimes from anterior division) |
|
|
Explain the ejaculation stage of sexual function? Explain innervation and parts involved?
|
3. Ejaculation – Somatic (also autonomic)
a. = expulsion of secretions and spermatozoa b. effected by rhythmic contractions of bulbospongiosus and ischiocavernosus muscles c. Pudendal nerve (S2-S4) e. Autonomics also: • Sympathetics – close internal urethral sphincter • Parasympathetics – contract urethral muscle |
|
|
Explain the Emmision stage of sexual function? innervation and details on parts involved?
|
2. Emission – Sympathetic (L1-L2)
a. = movement of semen into prostatic urethra b. Peristalsis of ductus deferentes and seminal vesicles c. Prostatic contraction adds prostatic fluid d. Several glands involved: seminal vesicles, prostate, and bulbourethral glands |
|
|
Explain the erection? innervation? Blood supply? Shat stage in sexual function is it?
|
Erection – Parasympathetic
a. Pelvic splanchnic nerves (S2-S4) b. Dilate helicine arteries, filling cavernous tissues with blood c. [ the bulbospongiosus and ischiocavernosus muscles help by compressing venous plexus, impeding venous return] |
|
|
Explain the innervation of the pelvic floor?
|
Pelvic floor
1. Somatics via pudendal n. (S2-S4) 2. Tonically active, relaxes during voiding |
|
|
Explain the innervation of the urethral sphincters?
|
Urethral sphincters
1. Internal – only present in males a. Smooth muscle at neck of bladder b. Prevents retrograde ejaculation into the bladder c. Sympathetic control 2. External a. Striated muscle, voluntary b. Permits holding urine paste point at which bladder would empty as a reflex; prevents leakage with stress, strain, and in sleep |
|
|
Explain the innervation of the vagina?
|
Vagina
• Innervation: o Lower ¼ = somatic (deep perineal branch of pudendal) o Upper ¾ = autonomic |
|
|
Explain the lower half of the Anal Canal? Derived from embryo? Lined by? unique structures? Innervation? blood supply? Lymphatics?
|
b. Lower ½
• Derived from ectoderm of proctodeum (future anal pit) • Lined by stratified squamous epithelium • No anal columns • Innervation: Somatic (inferior rectal branch of pudendal n.) • Arteries: Inferior rectal (of internal pudendal) • Veins: Inferior rectal (draining to internal pudendal) • Lymphatics: Travel inferiorly, eventually to superficial inguinal nodes |
|
Explain the lymphatics of the pelvis? Label this pic
|

Lymphatics
1. Inguinal nodes (superficial & deep) – receives lymph from lower limbs & lowest body wall (including external genitalia) 2. External & Internal iliac nodes – receive lymph from pelvis & inguinal nodes 3. Common iliac nodes – receive lymph mainly from external & internal iliac nodes 4. Lumbar nodes – receive lymph from common iliac nodes |
|
|
Explain the parasympathetic innervation of the bladder and rectum?
|
3. Parasympathetics (S2-S4)
a. Motor – contracts detrusor and rectal muscles b. Sensory – conveys normal sensation of bladder and rectal distension |
|
|
Explain the Pelvic Brim? Whats an alternate name? What are its borders?
|
pelvic brim or pelvic inlet = pectineal line of pubis, arcuate line of ilium, & sacral promontory
|
|
|
Explain the pudendal nerve block?
|
Pudendal anesthesia, also known as a pudendal block, or saddle block, is a form of local anesthesia commonly used in the practice of obstetrics to relieve pain during pregnancy. The anesthesia is produced by blocking the pudendal nerves near the ischial spine of the pelvis.[1] The ischial spine separates the greater and lesser sciatic foramina.
The pudendal block gets its name because a local anesthetic, such as lidocaine or chloroprocaine, is injected into the pudendal canal where the pudendal nerve is located. This allows quick pain relief to the perineum, vulva, and vagina. A pudendal block is usually given in the second stage of labor just before delivery of the baby. It relieves pain around the vagina and rectum as the baby comes down the birth canal. It is also helpful just before an episiotomy . Lidocaine is usually preferred for a pudendal block because it has a longer duration than chloroprocaine which usually lasts less than one hour.[2] |
|
|
explain the seminal vesivle function
|
Seminal vesicles
• Paired glands secreting thick fluid into ejaculatory ducts |
|
|
Explain the somatic innervation of the bladder and rectum?
|
Somatics (S2-S4)
a. Motor – to external anal sphincter, external urethral sphincter, & pelvic floor muscles (tonically active, so inhibition causes relaxation) b. Sensory – afferents from external anal sphincter, external urethral sphincter, pelvic floor muscles, anal canal, and urethra (including prostatic part) |
|
Explain the sphincters of the anal canal? Divisions and parts? Innervation? Label the pic?
|
Anal Canal
3. Sphincters a. Internal • 1 part: thickening of inner circular muscular coat at proximal anal canal • Involuntary b. External • 3 parts: o Subcutaneous – encircles lower end o Superficial – encircles middle region o Deep – encircles upper end (blends with puborectalis) • Voluntary, innervated by inferior rectal n. (br. of pudendal n.) |
|
|
Explain the structure of the vagina? Where is it located with regaurds to the urethra/bladder, rectum?
|
Vagina
• = musculomembranous tube running from cervix to vestibule (so partly in pelvis, partly in perineum) • Posterior to urethra and bladder, anterior to rectum |
|
|
Explain the sympathetic innervation of the bladder and rectum?
|
2. Sympathetics (T11-L2)
a. Motor – contracts internal anal and internal urethral sphincter; also causes contraction of internal urethral sphincter, ductus deferens, seminal vesicles, and prostatic muscles during sexual function b. Sensory – poorly localized, most sensitive to feelings of distension |
|
|
Explain the upper half of the anal Canal? derived? lined by what cells? structures it has? innervation? blood supply? lymphatics?
|
Anal Canal
1. Closely related to perineal body, anococcygeal body, & ischioanal fossae 2. Divided into upper and lower halves, based upon embryology (i.e. pectinate line) a. Upper ½ • Derived from hindgut endoderm • Lined by columnar epithelium • Anal columns = vertical folds, indicating anorectal jxn o Semilunar folds (or anal valves) – inferior aspect indicates pectinate line • Innervation: autonomic (review abdominal cavity lectures…) • Arteries: superior (off IMA) & middle rectals (off int. iliac) • Veins: superior rectal (drains into IMV) • Lymphatics: Travel superiorly, eventually to inferior mesenteric nodes |
|
|
Explain the ureters in men? Explain structure of ureters? Blood supply? Inervation? and ureter location?
|
Ureters
a. = retroperitoneal muscular tubes transporting urine from kidneys to posterosuperior bladder b. enter bladder obliquely, forming flap valves so muscular contractions of bladder act as sphincters preventing urinary reflux into ureters c. FEMALES: ureters pass medial to uterine arteries’ origins d. MALES: ductus deferentes rest between ureters and peritoneum e. Arterial supply: via nearby arteries (in pelvis = uterine in females, inferior vesicular in males) f. Innervation: via nearby autonomic plexuses (renal, aortic, superior and inferior hypogastric) |
|
|
Explain the Urethra in females vs males? Also explain where urine exits
|
FEMALES:
• descends anterior to vagina (partly pelvic, partly perineal) • urine exits via external urethral orifice • glands exist adjacent to urethra (will discuss in perineum) MALES: • much longer and more complex than in females • 2 urethral curves in flaccid penis; 1 in erect penis |
|
|
Explain ureters in Female? Blood supply? Innervation? Location?
|
Ureters
a. = retroperitoneal muscular tubes transporting urine from kidneys to posterosuperior bladder b. enter bladder obliquely, forming flap valves so muscular contractions of bladder act as sphincters preventing urinary reflux into ureters c. FEMALES: ureters pass medial to uterine arteries’ origins d. MALES: ductus deferentes rest between ureters and peritoneum e. Arterial supply: via nearby arteries (in pelvis = uterine in females, inferior vesicular in males) f. Innervation: via nearby autonomic plexuses (renal, aortic, superior and inferior hypogastric) |
|
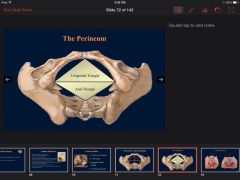
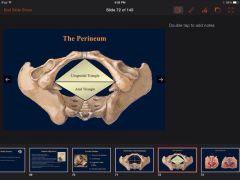
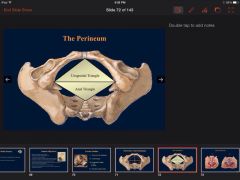
Explain what the perineum is? What are its boundaries? What is it broken into? What are those in those dividions of the perineum? Label it?
|
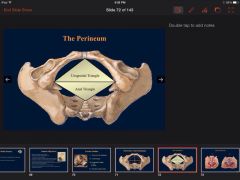
Perineum = trunk inferior to pelvis
1. diamond-shaped area, when viewed with thighs abducted 2. bounded by coccyx, ischial tuberosities, and pubis 3. a line through ischial tuberosities divides it into 2 triangles: a. Anal triangle • Posterior triangle • Includes anal canal & paired ischioanal fossae b. Urogenital triangle • Anterior triangle • Includes different structures in male & female o MALE: penis, scrotum, testis, & epididymis o FEMALE: vulva = female external genitalia; mons pubis, labia majora, labia minora, vestibule, vaginal orifice, clitoris |
|
How does the internal iliac branch? List the branches ? Label?
|
Common Iliac A’s
1. Internal Iliac a. Anterior Division • Umbilical o Superior vesicular - Artery to ductus deferens (variable) • Obturator • Inferior vesicular • Middle rectal • Internal pudendal • Inferior gluteal • Uterine o Vaginal b. Posterior Division • Iliolumbar • Lateral sacral • Superior gluteal – extremely variable (sometimes from anterior division) |
|
|
How many joints are in the pelvis? Name them? What kind of joint are they?
|
4. Sacroiliac (synovial joint), lumbosacral (secondary cartilaginous), sacrococcygeal (secondary cartilaginous), and pubic symphysis (secondary cartilaginous)
Secondary cartilaginous joints: (symphysis): These are also known as fibro-cartilaginous joints. There articular surface is covered by a thin layer of hyaline cartilage and the bones are united by fibro-cartilage. These joints are permanent and persist throughout the life of an individual. Typically the secondary cartilaginous joints occur in the median plane of the body and permit limited movements because of compressible pad of cartilage in them synovial joint-There articular surfaces are covered with hyaline cartilage. This articular cartilage is avascular, non nervous and elastic. Lubricated with synovial fluid, the cartilage forms slippery surfaces for free movements. |
|
|
How many ligaments are in the pelvis? Name them? What do they connect?
|
2 ligaments
Sacrospinous ligament- sacrum to ischial spine Sarcotuberous ligament- sacrum to ischial tuberosity |
|
Label and explain the Pelvic fascia pouchs? where are they located? Distinguish betwen which are in male or females?
|
Spaces
1. Retropubic space (Space of Retzius) – behind pubis, accommodates bladder distension 2. Retrorectal space – behind rectum, accommodates rectal expansion 3. Rectovesical pouch – in males, between bladder/prostate & rectum 4. Vesicouterine pouch – in females, between bladder & uterus 5. Rectouterine pouch (Pouch of Douglas) – between uterus and rectum • may be easily accessed via posterior fornix |
|
|
Label and name the parts of the male superficial perineal pouch?
|
Contents of Male Superficial Perineal Pouch:
a. Proximal spongy urethra b. Root of penis (i.e. the bulb and crura) c. Muscles covering the bulb and crura • Bulbospongiosus muscles o Paired muscles, fused as median tendinous raphe o Cover the bulb of the penis o Compress bulb and crura when contracted, which aids - Emptying spongy urethra of residual urine/semen - Erection by increasing pressure on erectile tissue in the root and compressing venous return (i.e. deep dorsal vein of penis) • Ischiocavernosus muscles o Paired muscles, covering crura o Compress each crus, which aids - Achieving and maintaining an erection via the compression of the crura (forcing blood distally) and by retarding venous return d. Superficial transverse perineal muscles • = small muscle bodies arising from ischial tuberosity and inserting into perineal body • They fix the perineal body e. Perineal body • = small fibrous mass in center of perineum • Structures attaching to the perineal body include the external anal sphincter, bulbospongiosus, and superficial perineal muscles f. Perineal branches of pudendal nerve • Supply perineal muscles and skin |
|
Label and name the contents of the male deep perineal pouch? Give function of each part?
|
Contents of Male Deep Perineal Pouch:
a. Intermediate urethra b. Sphincter urethrae (external sphincter of the urethra) • Muscle surrounding urethra • Voluntary innervation, by perineal branch of the pudendal n. c. Bulbourethral glands (formerly Cowper’s) • Glands posterolateral to intermediate urethra and sphincter urethrae • Ducts extend into superficial perineal pouch to enter spongy urethra • Produces pre-ejaculate, lubricating urethra for sperm d. Deep transverse perineal muscle • Tiny! Posterior to sphincter urethrae • Extends from ischial rami to perineal body e. Dorsal nerve of the penis (of pudendal n.) • Supplies skin of penis and glans penis f. Internal pudendal vessels, the arterial branches are: • Artery to bulb of penis (supplies posterior corpus spongiosum and bulbourethral gland) • Deep arteries of the penis (fill crura and corpora cavernosa with blood; aids in erection) o Helicine branches – open into cavernous spaces, coiled arteries in flaccid penis • Dorsal arteries of the penis (supply fibrous tissue around corpora and penile skin) |
|
Label the homologous structures of the male and female genitalia?
|
|
|
|
Label the Os Coxa, The Sacrum, The coccyx? What do theese bones make up?
|
They make up the bony Pelvis.
|
|
Label the parts of Hip Bone? Whats another name for it?
|
Ilium, Ischium, Pubis....Os Coxa
|
|
|
Label the parts of the male urogenital triangle for penis and scrotum.
|
Contents: scrotum & penis
• Be familiar with prepuce, frenulum, glans, corona, and penile, scrotal & perineal raphes • Anatomical position: penis erect |
|
|
Locate the Greater and lesser sciatic notches? What are they converted to when ligaments are attached? What ligaments are attached?
|
Converted to the greater and lesser sciatic foramina. An opening between the pelvis and the posterior thigh. The sacrotuberous and sacrospinous ligaments of the pelvis are attached.
|
|

Name and Identify where urine goes when exiting the ureter? Name the function? Position of that structure in children vs adults?
|
Bladder
a. Function = temporary reservoir for urine b. Position – variable dependent upon age and individual state • Adults: empty bladder rests in lesser pelvis; full may extend to umbilicus • Children: empty bladder may rest in abdomen (even when empty) |
|

Name and descibe the parts of the female UG triangle? label the parts of the UG?
|

Labia – folds of external skin
• Labia majora o = prominent folds of skin, providing protection o Filled with fat, smooth muscle, and terminal part of round ligament • Labia minora o = folds of skin, medial to labia majora o Form the prepuce & frenulum o Vestibule = space between labia minora, containing the external meati of the urethra, vagina, and ducts of the greater and lesser vestibular glands Clitoris • Root o = attached portion in superficial perineal pouch o 3 masses of erectile tissue (covered with muscles): Bulb of the vestibule – homologous with bulb of penis and corpus spongiosum; divided into 2 parts, surrounding vaginal and urethral orifice, but unite within the glans R & L crura – attach to pubic arch and become the corpora cavernosa • Body o = proximal detached portion of clitoris (glans is head) o 3 masses of erectile tissue: 2 corpora cavernosa & 1 slender erectile body from the bulb (formed by the uniting of the halves of the bulb of the vestibule) |
|

Name and describe the contents of female superficial perineal pouch? Label the nerve?
|

Contents of Female Superficial Perineal Pouch:
a. Root of clitoris (i.e. the bulb and crura) b. Muscles covering the bulb and crura: • Bulbospongiosus muscles o Cover bulb of the vestibule and greater vestibular glands o Compress deep dorsal vein of clitoris & weakly constrict vagina • Ischiocavernosus muscles (assist in erection) c. Greater vestibular glands • Open into vestibule, posterolateral to vaginal orifice • Secrete lubricating mucus during sexual arousal d. Lesser vestibular glands (Paraurethral) • Correspond to male’s prostate • Open into vestibule, lateral to urethral orifice • Secrete mucus into vestibule, for distribution to labia & vestibule e. Superficial transverse perineal muscles f. Perineal body g. Perineal branches of pudendal nerve |
|
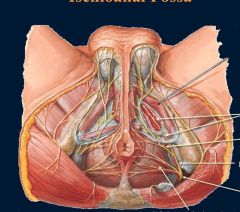
Name and describe the contents of the female superficial perineal pouch? Id structures on the image bottom right?
|
Contents of Female Superficial Perineal Pouch:
a. Root of clitoris (i.e. the bulb and crura) b. Muscles covering the bulb and crura: • Bulbospongiosus muscles o Cover bulb of the vestibule and greater vestibular glands o Compress deep dorsal vein of clitoris & weakly constrict vagina • Ischiocavernosus muscles (assist in erection) c. Greater vestibular glands • Open into vestibule, posterolateral to vaginal orifice • Secrete lubricating mucus during sexual arousal d. Lesser vestibular glands (Paraurethral) • Correspond to male’s prostate • Open into vestibule, lateral to urethral orifice • Secrete mucus into vestibule, for distribution to labia & vestibule e. Superficial transverse perineal muscles f. Perineal body g. Perineal branches of pudendal nerve |
|
Name and describe the contents of the female UG? Label the Image?
|
Labia – folds of external skin
• Labia majora o = prominent folds of skin, providing protection o Filled with fat, smooth muscle, and terminal part of round ligament • Labia minora o = folds of skin, medial to labia majora o Form the prepuce & frenulum o Vestibule = space between labia minora, containing the external meati of the urethra, vagina, and ducts of the greater and lesser vestibular glands Clitoris • Root o = attached portion in superficial perineal pouch o 3 masses of erectile tissue (covered with muscles): - Bulb of the vestibule – homologous with bulb of penis and corpus spongiosum; divided into 2 parts, surrounding vaginal and urethral orifice, but unite within the glans - R & L crura – attach to pubic arch and become the corpora cavernosa • Body o = proximal detached portion of clitoris (glans is head) o 3 masses of erectile tissue: 2 corpora cavernosa & 1 slender erectile body from the bulb (formed by the uniting of the halves of the bulb of the vestibule) |
|
Name and describe the contents of the male deep perineal pouch? Identify structures?
|
Contents of Male Deep Perineal Pouch:
a. Intermediate urethra b. Sphincter urethrae (external sphincter of the urethra) • Muscle surrounding urethra • Voluntary innervation, by perineal branch of the pudendal n. c. Bulbourethral glands (formerly Cowper’s) • Glands posterolateral to intermediate urethra and sphincter urethrae • Ducts extend into superficial perineal pouch to enter spongy urethra • Produces pre-ejaculate, lubricating urethra for sperm d. Deep transverse perineal muscle • Tiny! Posterior to sphincter urethrae • Extends from ischial rami to perineal body e. Dorsal nerve of the penis (of pudendal n.) • Supplies skin of penis and glans penis f. Internal pudendal vessels, the arterial branches are: • Artery to bulb of penis (supplies posterior corpus spongiosum and bulbourethral gland) • Deep arteries of the penis (fill crura and corpora cavernosa with blood; aids in erection) o Helicine branches – open into cavernous spaces, coiled arteries in flaccid penis • Dorsal arteries of the penis (supply fibrous tissue around corpora and penile skin) |
|
Name and describe the contents of the male deep perineal pouch? Label the arteries in particular? Also name fuctions for each part named?
|
Contents of Male Deep Perineal Pouch:
a. Intermediate urethra b. Sphincter urethrae (external sphincter of the urethra) • Muscle surrounding urethra • Voluntary innervation, by perineal branch of the pudendal n. c. Bulbourethral glands (formerly Cowper’s) • Glands posterolateral to intermediate urethra and sphincter urethrae • Ducts extend into superficial perineal pouch to enter spongy urethra • Produces pre-ejaculate, lubricating urethra for sperm d. Deep transverse perineal muscle • Tiny! Posterior to sphincter urethrae • Extends from ischial rami to perineal body e. Dorsal nerve of the penis (of pudendal n.) • Supplies skin of penis and glans penis f. Internal pudendal vessels, the arterial branches are: • Artery to bulb of penis (supplies posterior corpus spongiosum and bulbourethral gland) • Deep arteries of the penis (fill crura and corpora cavernosa with blood; aids in erection) o Helicine branches – open into cavernous spaces, coiled arteries in flaccid penis • Dorsal arteries of the penis (supply fibrous tissue around corpora and penile skin) |
|
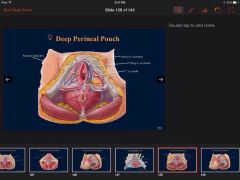
Name and describe the female deep perineal pouch contents? Label pic of the vessels?
|

Contents of Female Deep Perineal Pouch:
a. Part of urethra b. Part of vagina c. Sphincter urethrae d. Deep transverse perineal muscles e. Internal pudendal vessels, arterial branches: • Posterior labial branches • Artery to the bulb • Deep artery of the clitoris • Dorsal artery of the clitoris f. Dorsal nerves of the clitoris (of pudendal n.) • Supplies skin of clitoris |
|
Name and explain the locations of the spaces in the pelvic fascia? Label this pic?
|
Spaces
1. Retropubic space (Space of Retzius) – behind pubis, accommodates bladder distension 2. Retrorectal space – behind rectum, accommodates rectal expansion 3. Rectovesical pouch – in males, between bladder/prostate & rectum 4. Vesicouterine pouch – in females, between bladder & uterus 5. Rectouterine pouch (Pouch of Douglas) – between uterus and rectum • may be easily accessed via posterior fornix |
|
Name describe and label the specializations of the male prostatic urethra
|
• Specializations of the prostatic urethra:
Urethral crest – median ridge Seminal colliculus – rounded eminence Prostatic utricle – cul-de-sac remnant of uterovaginal canal in seminal colliculus Openings of ejaculatory ducts in seminal colliculus (inferior to prostatic utricle) Openings of prostatic ducts – lateral to seminal colliculus |
|
Name the contents of female deep perineal pouch? Label image with structures?
|
Contents of Female Deep Perineal Pouch:
a. Part of urethra b. Part of vagina c. Sphincter urethrae d. Deep transverse perineal muscles e. Internal pudendal vessels, arterial branches: • Posterior labial branches • Artery to the bulb • Deep artery of the clitoris • Dorsal artery of the clitoris f. Dorsal nerves of the clitoris (of pudendal n.) • Supplies skin of clitoris |
|
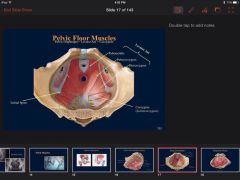
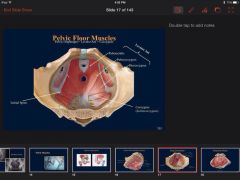
Name the muscles of Levator ani? Explain their connections and relation to one another in space? Label them?
|
Levator ani, composed of (medial to lateral):
• Puborectalis – muscular sling arising from pubis; maintains fecal continence; This muscle is sometimes treated as part of the pubococcygeus • Pubococcygeus – arises from pubis & tendinous arch, attaching to coccyx • Iliococcygeus – arises from tendinous arch & ischial spine and blends with pubococcygeus |
|
|
Name the parts of the urinary system? Which part is considered part of the abdomine and why?
|
Kidneys are considered abdominal organs, although embryologically pelvic]
|
|
Name the pelvic joints? Label them? What do they joint with?
|
1. Sacroiliac – synovial joint
2. Lumbosacral – secondary cartilaginous (fibrocartilaginous) joint with IV disc 3. Sacrococcygeal – secondary cartilaginous (fibrocartilaginous) joint with IV disc 4. Pubic symphysis – secondary cartilaginous (fibrocartilaginous) joint |
|
|
The anal canal is part of what portion of the perineum? It is closely related to ? what are the divisions and what explain how they are derived, lined by what cells, ways to physically id them? Innervation? blood supply?and lymphatics? sphincters?
|
Anal Canal
1. Closely related to perineal body, anococcygeal body, & ischioanal fossae 2. Divided into upper and lower halves, based upon embryology (i.e. pectinate line) a. Upper ½ • Derived from hindgut endoderm • Lined by columnar epithelium • Anal columns = vertical folds, indicating anorectal jxn o Semilunar folds (or anal valves) – inferior aspect indicates pectinate line • Innervation: autonomic (review abdominal cavity lectures…) • Arteries: superior (off IMA) & middle rectals (off int. iliac) • Veins: superior rectal (drains into IMV) • Lymphatics: Travel superiorly, eventually to inferior mesenteric nodes b. Lower ½ • Derived from ectoderm of proctodeum (future anal pit) • Lined by stratified squamous epithelium • No anal columns • Innervation: Somatic (inferior rectal branch of pudendal n.) • Arteries: Inferior rectal (of internal pudendal) • Veins: Inferior rectal (draining to internal pudendal) • Lymphatics: Travel inferiorly, eventually to superficial inguinal nodes 3. Sphincters a. Internal • 1 part: thickening of inner circular muscular coat at proximal anal canal • Involuntary b. External • 3 parts: o Subcutaneous – encircles lower end o Superficial – encircles middle region o Deep – encircles upper end (blends with puborectalis) • Voluntary, innervated by inferior rectal n. (br. of pudendal n.) |
|
The penis is in what part of the perineum? Label the parts? and explain function
|
Penis -part of the UG triangle
• Root o = attached part of penis, located in superficial perineal pouch o 3 masses of erectile tissue (covered with muscles) - Bulb - attached to UG diaphragm; pierced by intermediate urethra - Right & Left crura – attached to ischiopubic rami • Body o = continuation of erectile tissues from the root o 3 cylinders of erectile tissue - Corpus spongiousum – continuation of bulb; contains urethra, expands to form glans - Corpora Cavernosa (n = 2) – formed by crura, bound by Deep penile/Buck’s fascia |
|
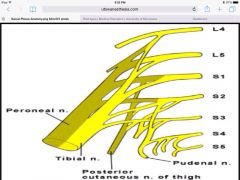
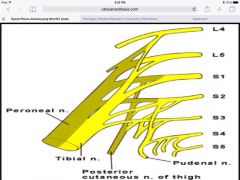
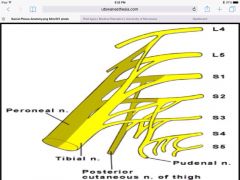
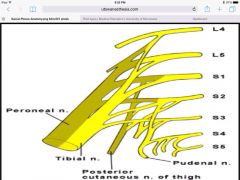
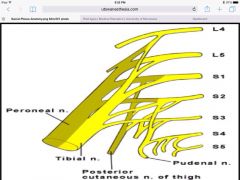
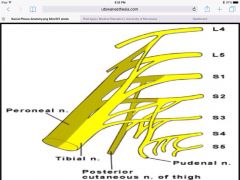
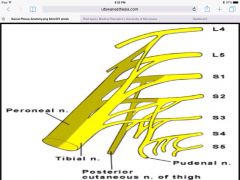
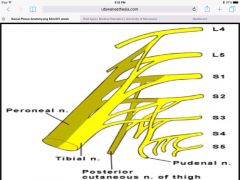
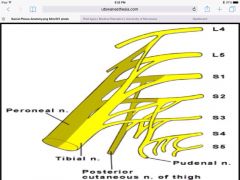
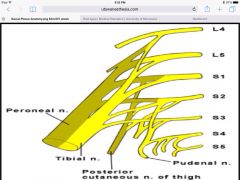
The Pudendal Nerve is part of what? what does it innervate? where does it branch from? Identify it?
|
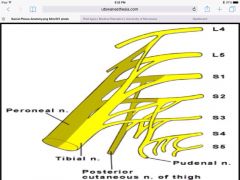
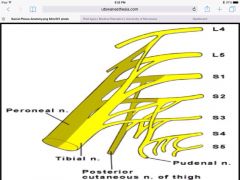
Sacral Plexus
1. Sciatic (L4-S3) a. anterior & posterior division b. exits pelvis via greater sciatic foramen c. supplies lower limb 2. Pudendal (S2-S4) a. anterior division b. exits pelvis via greater sciatic foramen, enters perineum via lesser sciatic foramen c. supplies skin and muscles of perineum; main sensory nerve for external genitalia 3. Superior gluteal (L4-S1) a. posterior division b. exits pelvis via greater sciatic foramen c. supplies gluteus medius, minimus, & tensor fascia latae (will be covered in gluteal lectures) 4. Inferior gluteal (L5-S2) a. posterior division b. exits pelvis via greater sciatic foramen c. supplies gluteus maximus (will be covered in gluteal lectures) |
|
The sciatic nerve is part of what? What does it innervate? wher does it exit? What plexus is it from?
|
Sacral Plexus
1. Sciatic (L4-S3) a. anterior & posterior division b. exits pelvis via greater sciatic foramen c. supplies lower limb 2. Pudendal (S2-S4) a. anterior division b. exits pelvis via greater sciatic foramen, enters perineum via lesser sciatic foramen c. supplies skin and muscles of perineum; main sensory nerve for external genitalia 3. Superior gluteal (L4-S1) a. posterior division b. exits pelvis via greater sciatic foramen c. supplies gluteus medius, minimus, & tensor fascia latae (will be covered in gluteal lectures) 4. Inferior gluteal (L5-S2) a. posterior division b. exits pelvis via greater sciatic foramen c. supplies gluteus maximus (will be covered in gluteal lectures) |
|
|
The scotum is part of the UG Triangle. Name its parts and label it?
|
Scrotum – contains testes, epididymides, and lower ends of spermatic
cords (covered earlier in semester) |
|
The superior gluteal nerve is part of what? Where does it branch from? Where does it exit? what does it innervate? ID it?
|
Sacral Plexus
1. Sciatic (L4-S3) a. anterior & posterior division b. exits pelvis via greater sciatic foramen c. supplies lower limb 2. Pudendal (S2-S4) a. anterior division b. exits pelvis via greater sciatic foramen, enters perineum via lesser sciatic foramen c. supplies skin and muscles of perineum; main sensory nerve for external genitalia 3. Superior gluteal (L4-S1) a. posterior division b. exits pelvis via greater sciatic foramen c. supplies gluteus medius, minimus, & tensor fascia latae (will be covered in gluteal lectures) 4. Inferior gluteal (L5-S2) a. posterior division b. exits pelvis via greater sciatic foramen c. supplies gluteus maximus (will be covered in gluteal lectures) |
|
|
What are bulbourethral glands? what do they do? where are they located?
|
Bulbourethral glands
• Small glands secreting during sexual arousal o Semen = a mixture of secretions by the testes, seminal vesicles, prostate, and bulbourethral glands (usually containing sperm) • Posterolateral to intermediate/membranous urethra • Ducts open into spongy urethra in bulb of penis |
|
What are the nerves that compose the sacral plexus? Wherer do they branch from? What do they inervate? Where do they exit?
|
Sacral Plexus
1. Sciatic (L4-S3) a. anterior & posterior division b. exits pelvis via greater sciatic foramen c. supplies lower limb 2. Pudendal (S2-S4) a. anterior division b. exits pelvis via greater sciatic foramen, enters perineum via lesser sciatic foramen c. supplies skin and muscles of perineum; main sensory nerve for external genitalia 3. Superior gluteal (L4-S1) a. posterior division b. exits pelvis via greater sciatic foramen c. supplies gluteus medius, minimus, & tensor fascia latae (will be covered in gluteal lectures) 4. Inferior gluteal (L5-S2) a. posterior division b. exits pelvis via greater sciatic foramen c. supplies gluteus maximus (will be covered in gluteal lectures) |
|
|
What are the 3 layers of the urogenital triangle?
|
Fascia
Superficial perineal pouch Deep perineal |
|
|
What are the 3 parts of the articulated pelvis? describe their location?
|
Pelvic brim or inlet, greater pelvis or False pelvis, and Lesser pelvis or True pelvis
|
|
|
What are the branches of arteries off of the common illiac?
|
Internal Iliacs and external Iliac
|
|
What are the contents of the anal canal? Include innervation blood supply. Label veins?
|
Contents:
a. Fat and connective tissue, which permit distension of anal canal b. Pudendal canal 1. = fascial canal on lateral wall (obturator internus) of fossa 2. Contents: (all enter canal at lesser sciatic notch) a. Pudendal nerve (S2-S4) • Exits pelvis via greater sciatic notch; enters perineum via lesser sciatic notch • Branches = inferior rectal, dorsal nerve of penis or clitoris, & perineal nerves b. Internal pudendal artery (off internal iliac a.) • Branches = inferior rectal & branches to penis or labia & clitoris c. Internal pudendal vein (tributaries correspond to arteries) d. FYI: n. to obturator internus enters canal, but exits early |
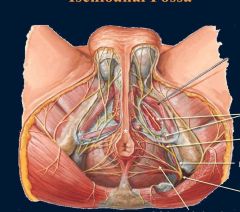
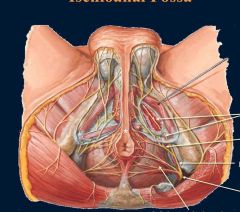
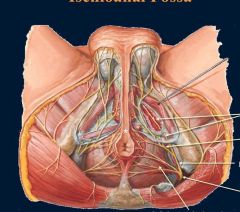
|
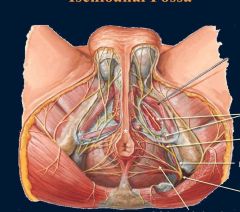
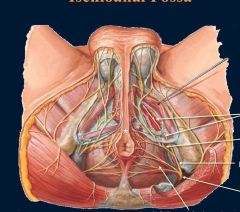
What are the contents of the Ischiorectal fossa? Include nerves and blood supply? Label arteries on pic?
|
Contents:
a. Fat and connective tissue, which permit distension of anal canal b. Pudendal canal 1. = fascial canal on lateral wall (obturator internus) of fossa 2. Contents: (all enter canal at lesser sciatic notch) a. Pudendal nerve (S2-S4) • Exits pelvis via greater sciatic notch; enters perineum via lesser sciatic notch • Branches = inferior rectal, dorsal nerve of penis or clitoris, & perineal nerves b. Internal pudendal artery (off internal iliac a.) • Branches = inferior rectal & branches to penis or labia & clitoris c. Internal pudendal vein (tributaries correspond to arteries) d. FYI: n. to obturator internus enters canal, but exits early |
|
What are the contents of the Ischiorectal fossa? Include nerves and blood supply? Label nerves on pic?
|
Contents:
a. Fat and connective tissue, which permit distension of anal canal b. Pudendal canal 1. = fascial canal on lateral wall (obturator internus) of fossa 2. Contents: (all enter canal at lesser sciatic notch) a. Pudendal nerve (S2-S4) • Exits pelvis via greater sciatic notch; enters perineum via lesser sciatic notch • Branches = inferior rectal, dorsal nerve of penis or clitoris, & perineal nerves b. Internal pudendal artery (off internal iliac a.) • Branches = inferior rectal & branches to penis or labia & clitoris c. Internal pudendal vein (tributaries correspond to arteries) d. FYI: n. to obturator internus enters canal, but exits early |
|
|
What are the differences between the musculature of male and female bladders?
|
FEMALES: muscle of bladder’s neck continuous with urethra’s muscle
MALES: muscle of bladder’s neck continuous with prostate’s fibromuscular tissue; muscle fibers form involuntary internal urethral sphincter (prevents semen from entering bladder) |
|
|
What are the differences in the pelvis between male and females?
|
1. pelvic inlet: females rounded/oval; males heart-shaped
2. pelvic canal: females short with parallel walls; males long and funnel-shaped 3. ischial tuberosities and spines: females everted; males not everted 4. greater sciatic notch: females broader; males narrower 5. pubic arch & subpubic angle: females broader (usually ≥ 90˚); males narrower (usually ≤ 70˚) 6. sacrum: females relatively short and broad; males relatively long and narrow |
|
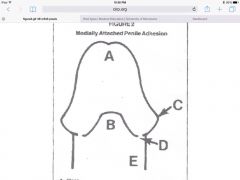
What are the fascia layers of the urogenital triangle? What layers are they continuous with in the abdomen? What are differences between the layers in men and women? Label the fascial layers.
|
Fascia
a. Superficial Fascia – Fatty Layer • In abdomen, this layer is called Camper’s Fascia • Continuous with ischioanal fat • Males: fat disappears in scrotum & penis • Females: continues into labia majora and mons pubis b. Superficial Fascia – Membranous Layer (Colles Fascia) • In abdomen, this layer is called Scarpa’s Fascia • Forms tubular sheath around penis & clitoris (Colles Fascia or superficial penile or clitoral fascia) • Males: contains the scrotum’s Dartos muscle c. Deep fascia • Continuous with fascia of external oblique • Forms suspensory ligament of penis or clitoris (fascial condensation extending from dorsal penis/clitoris to pubis) • Continues as the Deep penile fascia (Buck’s Fascia) o Holds penile corpora together |
|
|
What are the function of the ovaries?
|
Glands housing and releasing ova
|
|
|
What are the functions of the pelvic floor muscles? What are the muscles of the pelvic floor known as? What are the names of those muscles?
|
functions to support viscera (particularly when increased intraabdominal
pressure) and aids voluntary control of urination of fecal continence Known as the Pelvic diaphragm. Composed of the Levator ani and Coccygeus muscles |
|
|
What are the major nerves of the pelvis?
|
Lumbosacral trunk (L4-L5)
Obturator (L2-L4) Accessory obturator when present Sacral Plexus Coccygeal Plexus Autonomics |
|
What are the male complexities to the fascia of the urogenital triangle? Label the parts? What are the functions of each layer?
|
Male complexities
a. Penis, internal to external: • Tunica albuginea surrounds corpora cavernosa and corpus spongiosum (erectile bodies) • Deep penile fascia (Buck’s) then binds erectile bodies together • Superficial penile fascia (Colles/Membranous) surrounds penis externally b. Scrotum • Membranous fascia (Colles) continues • Dartos muscle contained within o Helps elevate testes a little (elevation is mainly the cremaster muscle’s job) o Mainly, wrinkles or expands skin of scrotum o Changes surface area exposed for thermoregulation o Innervation: Genital branch of genitofemoral |
|
|
What are the muscles of the vagina called?
|
• Compressed via several muscles, these include the external urethral sphincter & bulbospongiosus
|
|
|
What are the parts of the bladder? In older men what is visible? What kind of muscle makes up the walls of the bladder?
|
Composed of several parts:
• Apex – anterosuperior aspect • Fundus – posterior wall of bladder • Body – area between apex and fundus • Neck – constriction • Trigone – triangle between ureteric and urethral openings uvula = projection of trigone visible in older men -Walls - primarily of detrusor muscle |
|
What are the parts of the female reproductive system? Label it?
|
Ovaries, uterine tubes, uterus, and vagina
|
|
|
What are the parts of the female UG?
|
Clitoris and labia
|
|
What are the parts of the male reproductive system?
|
Testes, epididymis, ductus deferentes, seminal vesicles, ejaculatory ducts, prostate, and bulourethral glands
|
|
|
What are the parts of the male superficial perineal pouch? Explain what each structure does?
|
Contents of Male Superficial Perineal Pouch:
a. Proximal spongy urethra b. Root of penis (i.e. the bulb and crura) c. Muscles covering the bulb and crura • Bulbospongiosus muscles o Paired muscles, fused as median tendinous raphe o Cover the bulb of the penis o Compress bulb and crura when contracted, which aids - Emptying spongy urethra of residual urine/semen - Erection by increasing pressure on erectile tissue in the root and compressing venous return (i.e. deep dorsal vein of penis) • Ischiocavernosus muscles o Paired muscles, covering crura o Compress each crus, which aids - Achieving and maintaining an erection via the compression of the crura (forcing blood distally) and by retarding venous return d. Superficial transverse perineal muscles • = small muscle bodies arising from ischial tuberosity and inserting into perineal body • They fix the perineal body e. Perineal body • = small fibrous mass in center of perineum • Structures attaching to the perineal body include the external anal sphincter, bulbospongiosus, and superficial perineal muscles f. Perineal branches of pudendal nerve • Supply perineal muscles and skin |
|
|
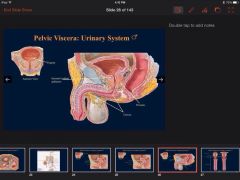
What are the parts of the pelvic viscera?
|
Pelvic Viscera = urinary bladder, parts of ureters, parts of reproductive system, & rectum
|
|
What are the parts of the Scrotum and Penis?
|
Contents: scrotum & penis
• Be familiar with prepuce, frenulum, glans, corona, and penile, scrotal & perineal raphes • Anatomical position: penis erect |
|
What are the parts of the uterine tubes? label?
|
Uterine Tubes, 4 parts:
• Infundibulum – funnel-shaped with fimbrae • Ampulla – widest and longest • Isthmus – entering uterine horns • Uterine part – short segment in uterine wall |
|
What are the parts of the uterus? Name and label them and their parts?
|
Uterus, 2 parts: Body & Cervix
• Body – upper 2/3rds o Fundus – superior to uterine tubes o Uterine horns – entrance of uterine tubes (obvious on radiographs) o Isthmus – constricted region superior to cervix • Cervix – neck o Internal os – opening to uterus o External os – opening to vagina |
|
|
What are the parts to the male urethra? Explain where they begin and end?
|
• 4 parts:
-Preprostatic – from neck of bladder to prostate -Prostatic – within prostate; gently curves -Intermediate/Membranous – short, narrow, and least distensible; passes through external urethral sphincter -Spongy – longest, ending at external urethral orifice of glans penis |
|
What are the subdividions of the broad ligament? what does each do? Id them?
|
o Broad ligament = mesentery of uterus, subdivisions:
-Suspensory ligament – conveys ovarian vessels, lymphatics, and nerves - Mesovarium – suspends ovary - Mesosalpinx – suspends uterine tube -Mesometrium – suspends most of uterus |
|
What are the supporting structures of the uterus? Label them?
|
• Supporting structures
o Ovarian ligament – ovary to uterus (posteroinferior to uterotubal junction) o Round ligament (ligamentum teres) – uterus (anteroinferior to uterotubal junction) to labia majora o Broad ligament = mesentery of uterus, subdivisions: -pelvic diaphragm |
|
|
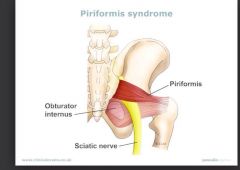
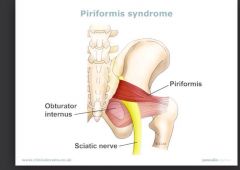
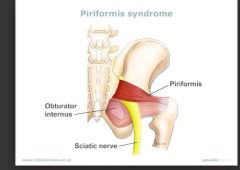
What are the three areas of the pelvis with muscles? What muscles are associated with each?
|
Lateral- obturator internus
Posterior- piriformis Pelvic floor- pelvic diaphragm |
|
What are the two pouch layers of the urogenital triangle? What are they spaces between? What do they communicate with? Which is easily ruptured? Label the pouch layers?
|
Superficial perineal pouch
a. = a potential space between Membranous / Colles Fascia and perineal membrane (a thin inferior fascia of UG diaphragm) b. Anteriorly, communicates with a potential space b/t abdominal fascia and abdominal muscles c. Posteriorly, closed at perineal body 3. Deep perineal pouch a. = a space between superior fascia of “UG diaphragm” & perineal membrane b. Essentially filled by sphincter urethrae and transverse perineal muscles • Sometimes called the UG diaphragm, as it was supposed to be a triangular muscular layer filling space between ischiopubic rami (not in reality!) c. This space is easily ruptured! |
|
What artery that is in the pelvis doesnt branch off of the iliacs? Where does it branch from? Locate it?
|
Gonadal A’s (testicular or ovarian) – directly from abdominal aorta
|
|
|
What bones make up the bony pelvis?
|
The Bony Pelvis (= os coxae/ hip bones, sacrum, and coccyx)
|
|
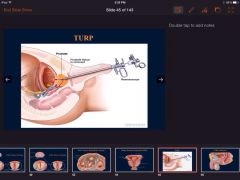
What causes this?
|
Benign Prostatic Hyperplasia BPH- problems with the bladder
|
|
|
What composes the male urogenital anatomy?
|
Scrotum and penis
|
|
|
What does the anterior portion of the perineum contain? what is it called? How does it differ from male and females
|
Urogenital triangle
• Anterior triangle • Includes different structures in male & female o MALE: penis, scrotum, testis, & epididymis o FEMALE: vulva = female external genitalia; mons pubis, labia majora, labia minora, vestibule, vaginal orifice, clitoris |
|
What ducts are associated the male reproduction? explain them? Identify them?
|
Ejaculatory ducts
• = 2 ducts formed by joining of seminal vesicle duct and ductus deferens, converging upon the seminal colliculus of prostatic urethra • Descends through posterior prostate |
|
|
What is a clinical condition shown in red? Explain it?
|
A retroverted uterus (tilted uterus, tipped uterus) is a uterus that is tilted posteriorly. This is in contrast to the slightly "anteverted" uterus that most women have, which is tipped forward toward the bladder, with the anterior end slightly concave.
|
|
|
What is a clinical issue with the anal canal? Does innervation play a factor?
|
Hemmorrhoids Yes above pectinate line is visceral innervation and below is somatic
|
|
|
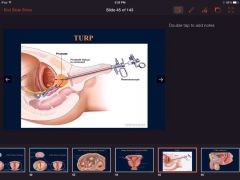
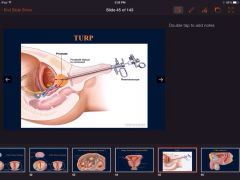
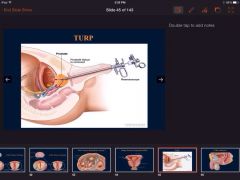
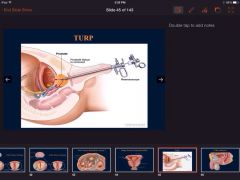
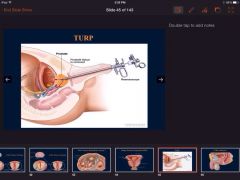
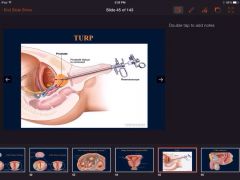
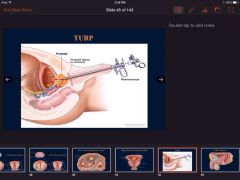
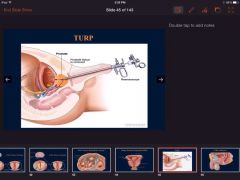
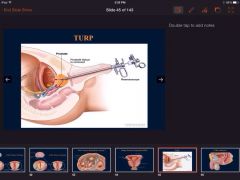
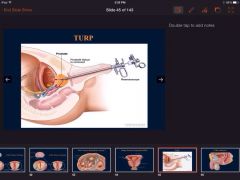
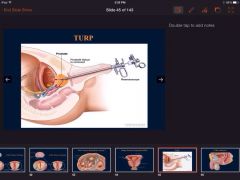
What is a comon disorder in older men that involves the prostate? how do you fix it? what are common symptoms?
|
|
|
|
What is another name for the ischioanal fossa
|
Ischiorectal fossa
|
|
What is the coccygeal plexus? Where does it come from? ID it?
|
Coccygeal Plexus
1. = small plexus from ventral rami of S4-S5 & coccygeal n’s |
|
What is the ductus deferentes a continuation of? what does it join? Label it?
|
Ductus deferentes (singular = ductus deferens)
• = continuation of duct of epididymis • Ampulla = expansion of ductus deferens • Joins duct of seminal vesicle to form ejaculatory duct |
|
|
What is the funcrion of the urinary system? What composes the urinary system? Explain order pee travels to leave the body through urinary system?
|
Functions to transport urine from kidneys to bladder, store urine, and transfer urine to outside world.
Kidneys, Ureters, Bladder, Urethra |
|
What is the function of ligaments in the pelvis? how many are there? Name them? Label them in the Pic?
|
Ligaments: Sacrotuberous & Sacrospinous
1. Functionally a. help prevent anteroinferior displacement of superior sacrum b. convert greater & lesser sciatic notches into greater & lesser sciatic foramina 2. Ligaments a. Sacrospinous ligament – sacrum to ischial spine b. Sacrotuberous ligament – sacrum to ischial tuberosity |
|
|
What is the general plan for innervation of pelvic and perineal organs?
|
General Plan:
1. Somatics – pelvic floor muscles and external sphincters (tonically active) 2. Sympathetics – internal sphincters 3. Parasympathetics – smooth muscle in organ walls |
|
What is the inferior gluteal nerve part of? Where does it branch off of? what does it innervate? where does it exit the pelvis? Id it?
|
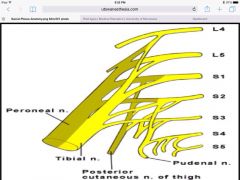
Sacral Plexus
1. Sciatic (L4-S3) a. anterior & posterior division b. exits pelvis via greater sciatic foramen c. supplies lower limb 2. Pudendal (S2-S4) a. anterior division b. exits pelvis via greater sciatic foramen, enters perineum via lesser sciatic foramen c. supplies skin and muscles of perineum; main sensory nerve for external genitalia 3. Superior gluteal (L4-S1) a. posterior division b. exits pelvis via greater sciatic foramen c. supplies gluteus medius, minimus, & tensor fascia latae (will be covered in gluteal lectures) 4. Inferior gluteal (L5-S2) a. posterior division b. exits pelvis via greater sciatic foramen c. supplies gluteus maximus (will be covered in gluteal lectures) |
|
|
What is the ischioanal fossa? What are its boundaries?
|
Ischioanal Fossa (formerly the ischiorectal fossa)
1. = fat-filled spaces lateral to anal canal 2. Boundaries (lots!): skin, levator ani, obturator internus & ischium, sacrotuberous & sacrospinous ligaments, & deep transverse perineal muscles a. anterior recess extends into UG triangle |
|
What is the orange region of the picture? explain its involvement? what it contains? divisions?
|
Prostate
• Accessory gland for male reproduction • Contains prostatic urethra • Divided into lobes (anterior, posterior, middle & lateral) • Prostatic ducts (n= 20-30) empty into prostatic sinuses on either side of seminal colliculus |
|
|
What is the pelvic fascia a continuation of? Explain the layers?
|
Pelvic Fascia = continuation of endoabdominal fascia
1. Parietal – lines walls and floor 2. Visceral – lines pelvic surfaces |
|
|
What is the position of the Uterus?
|
Typically anteverted an anteflexed
In most women, the uterus is anteverted and anteflexed. Anteversion refers to the position of the uterus in which its long axis is bent forward on the long axis of the vagina. Anteflexion refers to the position in which the long axis of the body of the uterus is bent forward on the long axis of the vagina at the internal os. |
|
|
What is the Posterior pelvic Muscle? What are its attachments? What is it a bed for?
|
Posterior – piriformis
1. attaches to sacrum within lesser pelvis (passes through greater sciatic foramen) and attaches to femur’s greater trochanter 2. “bed” for sacral nerve plexus |
|
What is the prineal body in obstetrics?
|
ABSTRACT The female perineal body is a mass of interlocking muscular, fascial, and fibrous components lying between the vagina and anorectum. The perineal body is also an integral attachment point for components of the urinary and fecal continence mechanisms, which are commonly damaged during vaginal childbirth. Repair of injuries to the perineal body caused by spontaneous tears or episiotomy are topics too often neglected in medical education. This review presents the anatomy and physiology of the female perineal body, as well as clinical considerations for pelvic reconstructive surgery.
|
|
|
What is the prterior part of the perineum called? what does it include?
|
Anal Triangle
• Posterior triangle • Includes anal canal & paired ischioanal fossae |
|
|
What is the true pelvis? Where is it located?
|
Lesser pelvis (or true pelvis) – actual pelvis; inferior to pelvic inlet & superior to pelvic outlet (space closed by pelvic diaphragm)
|
|
|
What is the urethra?
|
A muscular tube conveying urine from bladder to the outside world
|
|
|
What makes up the perineum?
|
The anal triangle and the urogenital triangle
|
|
|
What muscle is this?
|
Obturator Internus
|
|
|
What nerve in the pelvis isnt always Present? Explain where it branches from?
|
Accessory obturator
|
|
What nerves in the Pelvis make are branches of the lumbar plexus? Label them? Where did they branch from?
|
A. Lumbosacral trunk (L4-L5)
B. Obturator (L2-L4) |
|
|
What parts of the male penis is located in the perineum not the pelvis?
|
Intermediate /Membranous and Spongy
|
|
|
What plexus of nerve is located in the Piriformis?
|
Bed for the sacral nerve plexus
|
|
What structure is the Coccygeus muscle apart of? ID It? what is it attached to?
|
Coccygeus is part of the pelic diaphragm with the levator ani muscles- located on the pelvic floor
Coccygeus (= ischiococcygeus) – ischial spine to coccygeus/sacrum |
|
|
What structures are extraperitoneal, primarily Retroperitonal, and intraperitoneal?
|
Peritoneal Reflections
1. Extraperitoneal or subperitoneal = technically outside or below the peritoneal cavity; this includes most pelvic viscera 2. Primarily Retroperitonal (PRP) – kidneys, ureters, rectum, anal canal; additionally the male prostate, seminal vesicles, & vas deferens 3. Intraperitoneal (IP) – uterus, ovaries, uterine tubes • FYI - Uterus is complicated and could be considered secondarily IP |
|
|
What two branches do the common illiac branch into?
|
Internal and external iliac
|
|
|
When giving birth how would you numb the woman?
|
|
|
|
Where is the detrusor muscle located?
|
In the walls of the bladder
|
|
Where is the false pelvis? Label it
|
Greater pelvis (or false pelvis) – lower part of abdominal cavity; superior to pelvic inlet
|
|
|
Where is the obturator internus located? Explain its attachments and where it arises? Does it have a membrane and if so name it?
|
Lateral Pelvis – obturator internus
1. arises within lesser pelvis (passes through lesser sciatic foramen) and attaches to femur’s greater trochanter 2. obturator membrane – lines obturator internus muscle (membrane forms tendinous arch medially) |
|
|
Where is the vagina in proximity to the cervix?
|
Vagina
• Superiormost vagina surrounds cervix as anterior, posterior, and lateral fornices (fornix = singular) • |

