![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
664 Cards in this Set
- Front
- Back
|
HEADS is what ?
|
H - Home
E - Education/Employment E - Eating disorder screening A - Activities/Affiliations/Aspirations D - Drugs (and alcohol, tobacco, and steroids) S - Sexuality S - Suicidal behavior (along with depression and mental health concerns) S - Safety (abuse, fights, weapons, seatbelts, etc.) |
|
|
Causes SGA
|
Etiologies of Small Size for Gestational Age at Birth
Maternal Factors: - Both young and advanced maternal age - Maternal prepregnancy short stature and thinness - Poor maternal weight gain during the latter third of pregnancy - Nulliparity - Failure to obtain normal medical care during pregnancy - Cigarette smoking, cocaine use, other substance abuse - Lower socioeconomic status - African-American ethnicity (in the United States) - Uterine and placental anomalies - Polyhydramnios - Intrauterine infections Fetal Factors: - Chromosomal abnormalities (e.g., trisomies) and syndromes - Metabolic disorders - Congenital infections (e.g., toxoplasmosis, rubella, cytomegalovirus) Medications and Other Exposures: - Amphetamines - Antimetabolites (e.g., aminopterin, busulfan, methotrexate) - Bromides - Cocaine - Ethanol - Heroin and other narcotics (e.g., morphine, methadone) - Hydantoin - Isotretinoin - Metal (e.g., mercury, lead) - Phencyclidine - Polychlorinated biphenyls (PCBs) - Propranolol - Steroids - Tobacco (carbon monoxide, nicotine, thiocyante) - Toluene - Trimethadione - Warfarin Placental and Uterine Abnormalities: - Avascular villi - Decidual or spiral artery arteritis - Infectious villitis (as with congenital or "TORCH" infections) - Multiple gestation (limited endometrial surface area, vascular anastomoses) - Multiple infarctions - Partial molar pregnancy - Placenta previa and abruption - Single umbilical artery, umbilical thrombosis, abnormal umbilical vascular insertions - Syncytial knots - Tumors, including chorioangioma and hemangiomas |
|
|
SGA vs IUGR
|
Terms:
SGA = baby small at TIME OF BIRTH IUGR = baby in mothers uterus small when size estimated by fundal height or other methods |
|
|
name enteroviruses
|
polio
cox hep a |
|
|
Food poisening
under 6 hours over 10 hours |
Under 6 hours :
1. Staph aureus toxin: vomit, Nausea, Diarr 2. B Cerus toxin : vomit, Nausea, "emetic syndrome" Over 10 hours 1. B cerus "diarr syndrome" diarr and cramps 2. Clos. perfringens eat bugs, toxin release in GI tract diarr and cramps |
|
|
Bloody inflammatory diarrhea
|
Shigella
** Salm typhi - thyphoid fever ** Salm enteritidis - the bad one Clos jejuni EHEC O157 and Entinvasive Yersinia - watery diarr Vibrio parahemolyticus ** C diff Entame histolytica |
|
|
Non Inflamm or watery diarrhea
|
TOXIN diarr: cholera, travel diarr EHEC
Clos perfringens (toxin release in GI) and BCerous. ROTA in kids Norwalk in adults ADENO older kids Giardia - duod with cysts C parvum |
|
|
Differential for infectious causes skin vesicles
|
Varicella
smallpox Coxsackie 1 and 2 HSV1 and 2 Molluscum contag |
|
|
DIff cellulitis
|
staph
strep psuedo past multicida in animal bites |
|
|
Diff myositis
|
Clos perf
staph Trich. spirialsis T solium ( eating raw pork) T spiralsis - pork or game Coxsackie B ( B body myocarditits, pericrditis, pleurodyania, muscle pain) dengue - bone break fever |
|
|
Varicella rash
|
red base has vesicles
spreads "centrifugally" ? |
|
|
Smallpox rash
|
starts in head, then extremities, then fill with pus and crust.
ALL in same stage. |
|
|
Rubella rash
|
First FEVER.Swollen glands.
Then pink maculopapular on FACE spreads to extremities. Lasts 3 days. rash is antidoy rxn in skin. Adults: rash, arthritis/arthalgias. Congenital: deaf, cataract, microceph, PDA. Live vaccine. |
|
|
- white lesions in mouth
- red maculopapular rash starts on head and progresses down trunk to feet. - high fever - cough and runny nose |
measles
Also PHOTOPHOBIA HIGH FEVER PRODROME RASH Kopliks deaths due to secondary PNA and postinf enceph |
|
|
child with fever of 103.5
maculopapular rash lasting 24-48 hours |
HSV6 rash
roseola or 6th diease or exanthum subitum VERY HIGH fever 103-106 rash starts on trunk - spreads to other parts of body. Can recur. |
|
|
slapped cheek rash
|
Parvo B19 erthyema infectiosum
|
|
|
sandpaper rash on trunk then spreads outward
|
Scarlet fever
Strep Pyogenes |
|
|
maculopapular rash on palms and soles spreads inward to trunk (centipedal)
|
RMSF R Rickettsii
Rx Doxy 150 BID |
|
|
spreading annular red lesion
|
Lyme - B Burgdofferi
|
|
|
maculopapular rash on palms and soles
|
T pallidum - syphilis
|
|
|
Papule forms and turns into ulcer with black base
|
tularemia
|
|
|
rash
inflammatitions, itching, scaly skin, pustules |
dematophytoses - ringworms
|
|
|
Coag neg staph
|
Staph epi
Staph sapro |
|
|
Coag pos Staph
|
Staph Aureus
All staph catalase + aurus is coag pos |
|
|
Beta hemolytic strep
|
Strep pyogenes - Bacitracin sens
Strep A galactiae - bacitracin resist |
|
|
alpha hemolytic strep
|
Strep PNA - optochin susp
S mutans |
|
|
child :
abn teeth (pointy) interstitial keratitis cranial nerve 8 deafness abn nose |
Congenital syphillis
also saber shins mulberry molars saddle nose |
|
|
What type of Chlamdia gets into babies eyes ?
|
Chlam trachomatis D-K
Use erythromycin drops at birth. |
|
|
osteomyelitis
|
Staph #1 : treat nafcillin OR clinda
Strep : penny PSeudomonas HInf in kids ! also w/ arthalgia/arthritis |
|
|
Neonatal menny
|
Group B strep
E Coli Listeria |
|
|
Viral menny older children
|
HSV2
mumps LChoriomen polio, cox, echo Arbovirus |
|
|
S/S congential toxo
|
Mom has 1 in pregmancy
enceph hydropceph blind anemia rash jaundice PNA |
|
|
dehydr 2 year old
watery diarr no fever no blood |
Rota
|
|
|
chlid with diarr then has bloody urine
|
EHEC O157 gets HUS
|
|
|
child in family
bloddy diarr |
Salmonella
all ate chicken dinner but kid got sicker. Are motile. LActose Neg. H2S postive. |
|
|
child in daycare
watery diarr with bloddy mucus flecks and PMNs cramps fever |
Shigella
|
|
|
Coxsackie A
|
RASH, CNS, COLDs
heprangina hand foot mouth meninngitis acute hemmoragic conjunctivtiis : red eyes, oain, |
|
|
Coxsackie B
|
MUSCLE, MenINGITIS
pleurodynia - fever and chest pain esp neonates : pericarditis, myocarditis, chest pain, arrhty, cardiomyopathy meninngitis (try plconaril) An entero so in stool. |
|
|
Parvo B19
|
First: fever, flu like and anemia
Then slapped cheek rash and maculopaprular rash with central clearning on body "lacy" - occ aplastic anemia Rx IvIg -adults polarthritis -fetal hydrops and stillbirth |
|
|
Immunizd to Hep B
|
You have anti-Hb S
You have no Hb S No HbE No antibodies to other parts of HepB unless you had real virus |
|
|
Sign of Hep B in window
|
IgM to Core
|
|
|
Mumps
|
fever, h/a/ big parotids
Risks: enceph, panc, menny |
|
|
3 Yo
pus vesicles on face swollen LN |
impetigo/pyoderma
|
|
|
child rash and strawberry tongue
|
scarlet fever erythrogenic toxon
|
|
|
baby blister like lesions all over body
|
scaled skin
|
|
|
2 YO
fever barking cough like a seal sore throat hoarse voice high pitched noise on inhalation |
croup
parainfluenza Try cool mist |
|
|
20 YO
nonprod cough low fever h/a tired |
Mycoplasma PNA - no cell wall
Also stevens-johnsons syndrome And Rx macolides like erythromycin or tetracyclines |
|
|
epiglottis
|
Hib
|
|
|
croup
|
#1 parainfl 2-5 YO "BARKING cough"
RSV flu |
|
|
infant
low grade fever cough expiratory wheeze tachycardia tachypnea |
RSV
bronchiolitis and PNA in those under 3 XRAY: hyperinfalted and diffuse infiltrates Try albuterol and ribavirin in ICU |
|
|
EBV in
5 YO versus college |
5 YO mild, sore throat and fever
college: mono |
|
|
kid 2
fever sore throat cough coryza |
acute febrile pharyngitis
adenovirus in under 3 YO |
|
|
pink eye
fever sore throat Cough coryza |
pharyngoconjunctival fever
realted to swimming pools |
|
|
infants and child
diarr (bloody) vomitting |
gastroent from Adeno
very contagious |
|
|
pin worm
|
Enterobius vermic
nematode / round pyrantel OR mebendazole |
|
|
whip worm trichuris trichiura
|
bile stained egg with polar plugs
pain bloddy diarr appendicitis Rx mebendazole |
|
|
Group B strep
|
Usually beta-hemolytic
S Agalactiae Cause neonatal menningitis, PNA, sepsis. In wk 1-3 mnth : bactremia with sepsis Pregnant Wn: UTI, postpartum sepsis DM/low immune: bactrmeia, PNA, bone and joint infection Rx: penny +/- aminogly |
|
|
strep pyogene
|
Group A
beta hemo Has toxin shock toxin scarlet fever, eryp, Pen, cephalo, erythro |
|
|
shigella
|
child daycare
invasive diarr, cramp, fever -floxacin -SMX-TMP |
|
|
To kill Staph aureus
|
Beta lactamase resistant pennys:
methicillin nafcillin oxacillin MRSA: VANc + gent + Rifampin |
|
|
To kill Staph epidermis
|
VANC
|
|
|
treat h pylori
|
triple for 2 weeks
amoxi PPI omeprazole clarithomycin bismuth OR quad with tetracycline, metro, bismuth, PPI omeprazole |
|
|
H i b menningitis
|
Affect kids over 6 months when mom Ab gone.
Rx ceftriaxone or other 3G cephalo prophy contacts rifamin |
|
|
child with long coughs and then a gasp whoop
|
Bordadella pertussis
toxin inc CAMP and kills cilia cells Rx erythro and macrolides |
|
|
16 year old
fever of 102 then after 2 days dizzy low BP myalgia diffuse rash below chest |
later palms peel -
Stah aureus toxic shock |
|
|
7 year old
has had fever and sore throat rough rash trunk and neck now on arms, worst in axilla spares palms and soles |
scarlet fever
strep throat will get strawberry tongue later Treat with penn ASO + |
|
|
cellulitis
acute fever shock |
Toxic shock from strep
Add penn G for Strep IN TSST add clindamycin to prevent scarlet fever toxin production |
|
|
Strep Group A vs B
|
Strep Group A = Strep pyogenes , mainly beta hemolytic
Strep Group B = Strep agalact and also mostly beta hemo I think |
|
|
Strep in pregnant women
|
Group B strep Agalact
Treat in preg with AMPicillin (is bacitracin resistant) |
|
|
Strep PNA
|
alpha hemolytic
- PNA rx cephalo or penn - o media rx cephalo or penn - menningitis Rx vanc USe Pneumovax |
|
|
asthma inhalers
|
albuterol B2 short acting
terbutaline : B2 selective, used emergency treatment status Long acting : salmeterol |
|
|
No good to use anti-histamines
|
angioedema
atopic dermatitis asthma |
|
|
cyproheptadine (periactin)
|
headache precentive
(a histamine drug) |
|
|
RA drugs
|
azathioprine : supress B and Ts
leflunomide (arava) inhibits pyrimidine. CI in under 18YO and if planning conception. TERATO and slow clearence. |
|
|
Cox2 drug
|
celecoxib
CI sulfa allergy USED RA, fam adeno polyposis Less gastric irritation |
|
|
TNF a drugs
|
etanercept dimer to bind TNF: RA, JRA,
infliximab monoclonal Ab : crohns and RA |
|
|
Inflam bowel drugs
|
sulfasalazine 5-ASA
mesalamine (Asacol) |
|
|
leukotriene drugs
|
Montelukast: LT receptor blocker (=Singulair)
EArlier in path: zileuton 5lipoox inhibitor but can inc theo and warf levels |
|
|
asthma steroid inhalers
|
corticoseroids : block PL2 turning PL to arach and cz bronchoconst
beclomethasone SE lowers bone density, candida in mouth Triamcinolone nasal Flunisolide fluticasone (Flovent) Strong: budesonide (Pulmicort) |
|
|
HSP vs ITP
|
HSP: Iga
ITP: anti plt antibodies HSP has normal plt count. ITP has LOW plt count. HSP: renal involve, more abd pain. More boys. W/U: CBC (plt count), UA, renal BUT NOT necc to do cell culture or PT/PTT |
|
|
How treat ITP
|
IvIg or RhoGAM
|
|
|
Spleen exam in kid and cause of big spleen.
|
Spleen:
Exam techniques: Place child supine, knees bent; helpful to start in RLQ and move superiorly. Lifting along left flank or having patient roll onto right side may help move spleen forward into a palpable position Spleen tip is palpable in one-third of neonates, 10% of normal children, and 2% of healthy adolescents. A spleen edge palpable more than 2 cm below the left costal margin is abnormal. Causes of splenomegaly: infection (e.g. EBV, CMV, bacterial sepsis, endocarditis), hemolysis (e.g. sickle cell disease), malignancy (e.g. leukemia, lymphoma), storage diseases (e.g. Gaucher), systemic inflammatory diseases (e.g. SLE or juvenile idiopathic arthritis - JIA), or congestion (e.g. related to portal hypertension.) |
|
|
How feel liver and cause of large liver
(from CLIPP) |
Liver:
Examine by palpating, percussing in the midclavicular line Place child supine, knees bent; helpful to start in RLQ and move superiorly In normal children, the liver edge may be palpable up to 3.5 cm below the costal margin in newborns and 2 cm below the costal margin in older children. Causes of hepatomegaly: inflammation (e.g. viral hepatitis), infiltration (e.g. leukemia/lymphoma), accumulation of storage products (e.g. glycogen storage disease), congestion (e.g. congestive heart failure), or obstruction (e.g. biliary atresia). |
|
|
My kid has a fever of 103F,
do I need to go to ER ? |
Yes if under 6-8 weeks old.
If older, need to ask more info, if on phone ....CLIPPP case |
|
|
IO lines
Indication? Ages ? Sites ? Risks ? PALS |
IO lines
Ind : fail at 3 periph IVS or 90 secs in PALS Kid < 6 faster vs central lines. Now fine in older kids. Site: #1 anteromedial tibia 1- 3 cm DISTAL to tibial tuberosity. ALso in femur, other end tibia, iliac crests. Comps: fx, fluids goes subQ, ostepmyelitis, emboli, Take out IO lines once have other line in. IO lines like IV lines and can give same fluids. |
|
|
Menningitis sepsis prophy - menninococcemia
|
Only close contacts warrant prophylaxis. Household, child care and nursery school contacts are considered high risk. Prophylaxis is recommended for those health care workers who had intimate exposure such as occurs with unprotected mouth-to-mouth resuscitation, intubation, or suctioning before antibiotics are administered. In adults, ciprofloxacin is the drug of choice. In children (<18 years old) either rifampin (p.o.) or ceftriaxone (IM) may be used for prophylaxis.
|
|
|
sweat chloride testing
|
value over 60 diagnostic of CF
Other cause of high sweat chl values: adrenal insuff ectodermal dysplasia nephrogenic Diabetes insipidis hypothyroidism malnutrition |
|

|
blue sclerra
Osteo gen imperfecta Ehlers-Danos Marfan. rare iron def anemia Look for : otosclerosis and hearing loss, cardio lesions - mitral regurg, floppy mitral, cystic medianecrosis aorta |
|
|
TREAT TB IN KIDS
|
TREATMENT OF TUBERCULOSIS DISEASE. The goal of treatment is to achieve sterilization of the tuberculous lesion in the shortest possible time. Achievement of this goal minimizes the possibility of development of resistant organisms. The major problem limiting successful treatment is poor adherence to prescribed treatment regimens. The use of DOT decreases the rates of relapse, treatment failures, and drug resistance; therefore, DOT is recommended strongly for treatment of children and adolescents with tuberculosis disease in the United States.
For M tuberculosis disease, a 6-month regimen consisting of isoniazid, rifampin, and pyrazinamide for the first 2 months and isoniazid and rifampin for the remaining 4 months is recommended for treatment of drug-susceptible pulmonary disease, pulmonary disease with hilar adenopathy, and hilar adenopathy disease in infants, children, and adolescents. If the chest radiograph shows a cavitary lesion or lesions and sputum remains culture positive after 2 months of therapy, the duration of therapy should be extended to 9 months. For children with hilar adenopathy in whom drug resistance is not a consideration, a 6-month regimen of only isoniazid and rifampin is considered adequate by some experts. When drug resistance is possible (see Table 3.75, p 690), initial therapy should include a fourth drug, either ethambutol or an aminoglycoside, until drug susceptibility results are available. If an isolate from the pediatric case under treatment is not available, drug susceptibilities can be inferred by the drug susceptibility pattern of isolates from the adult source case. If this information is not available, local endemic rates of single and multiple drug resistance can be helpful. Data may not be available for foreign-born children or in circumstances of international travel. If this information is not available, a 4-drug initial regimen is recommended. In the 6-month regimen with triple-drug therapy, isoniazid, rifampin, and pyrazinamide are given once a day for the first 2 weeks. Between 2 weeks and 2 months of treatment, isoniazid, rifampin, and pyrazinamide can be given daily or twice a week by DOT. After the initial 2-month period, a DOT regimen of isoniazid and rifampin given twice a week is acceptable (see Table 3.72, p 686, for doses). Several alternative regimens with differing durations of daily therapy and total therapy have been used successfully in adults and children. These alternative regimens should be prescribed and managed by a specialist in tuberculosis. |
|
|
Who gets TB drugs even without TB symptoms ?
|
1. Child with postive PPD (high risk kid >5mm, kid over 4 >10mm)
2. INH for kids under 6 exposed to infected adult (false neg PPD) 3. INH infants of moms w/TB If exposed kids PPD negative after 3 months can d/c meds. |
|
|
What is a postive PPD in kids ?
|
high risk kid is 5 mm
kid over 4 is 10 mm But young kids have false neg as do malnutrition. If exposed to adult, under 6, use INH for 3 months and repeat PPD. |
|
|
rare comp staphlococcal PNA ?
|
tension pneumothorax :
needle to 2-3 ICS MCL. Can be due to pneumocele which is rare in PNA (1%) but 85% in staphccocc aureus PNA. Do not see on admit xray, but days later sudden resp distress. |
|
|
spasmodic croup
|
adol and teens OR First aid says 1-3YO
not a bug recurrent nighttime, insp stridor bark cough, worse when excited. Use cold mist and calm kid gets better on own so don't give steroids. |
|
|
steeple sign on xray
|
croup
on AP |
|
|
If think epiglottitis
DO NOT |
lay supine
examine throat venipuncture give narc or antihist no xray TO OR and intubate Dx laryngoscopy Tx: ceftriaxone and rifampin for contacts |
|
|
If you did do an xray in epiglottis, after intubation in OR
|
LATERAL xray
thumbprint sign drool tripod tACKYCARDIA toxic NO COUGH |
|
|
tracheitis
|
rapid upper airway obst but slower vs epiglottitis
Bugs: Staph and Hae Ib Often after Infl A high fever, toxic, Inspir stridor LATERAL XRAY like epiglottis : thumbprint PSEUDOMEMBRANE pus secretions RX: ceftriaxone, amp-sulbactam and ICU |
|

A vacc child.
Few days of URI : sore throat, cough (barky. )Then fever to 104F, insp and expir stridor. arrow goes to membrane |
tracheitis.
rapid upper airway obst but slower vs epiglottitis. Bugs: Staph and Hae Ib. Often after Infl A Sudden high fever, toxic, Inspir stridor LATERAL XRAY like epiglottis : thumbprint PSEUDOMEMBRANE pus secretions can rapidly block airway to INTUBATE RX: ceftriaxone, amp-sulbactam and ICU |
|
|
comps of RSV ?
Ages ? |
RSV in mostly in 1-9 Months but really 0-2 YRs
Comps: bactremia, pericarditits, cellulitis, empyema, meningitis, supporative arthritis. |
|
|
treat sinusitits
|
PreTest:
Just 10-14 days antibiotics. decong and antihist no use. |
|
|
When is racemic epi given ?
|
viral croup or Parainfluenze I and III
|
|
|
infant alone with dollhouse.
coughs. then drooling. |
FB esophagus.
Later on avoid food more then liquids. |
|
|
young boy with sickle anemia
sudden fever to 104 tackypnea cough |
Diff: PNA, pulm thromboemboli, sepsis
Note: In anemia, cannot rely on cyanosis as that requires certain amt of blue RBCs to be in skin caps. |
|
|
If you have metabolic alkalosis from diuretics what is your ABG ?
|
High PCO2 from hypoventilation
low PO2 you get low K from diuretics |
|
|
What is a sign of an impossible blood gas ??
|
On Room Air
If O2 goes up The PCO2 must go down in proportion |
|
|
DOC strep throat
|
oral pen V 25-50 mg/kg/day x 10 days OR 500mg TID for adult
IM: benzathine and procaine penicillin single dose weight based If penny allergy : macrolide or clinda x 10 days NO SULFONAMIDES |
|
|
When to admit patient with whooping cough ?
How long contagious ? |
infant under 3 months (apnic episodes)
apnea or cyanosis resp distress Use macrolides to dec spread and isolate until on abx 5 days |
|
|
Diag signs pertussis ?
|
insp whoop
post tussive emesis lymphocytosis CXR butterfly PCR + nasophar secretions |
|
|
tachycardia out of proportion to fever
|
diptheria
|
|

adenoid ?
When to remove ? |
Adenoid facies : pinched nose, and open mouth.
Remove adenoids when hypertrophy -> open mouth breathing, snoring, hyponasal speech, persistant rhinitis, recurrnet OM or nasopharyngitis. Don't do tonsils out also unless separate indication. |
|

sudden high fever, hard to swallow
throat pain toxic hyperextension of head |
retropharn abscess
note pre vertebral edema. Normal retrophar space should be under half-width of adj vertebra. Also can see abn air pocket behind vertebra. RX clinda or amp-sulbactam Note- after age 3 no more LN here. |
|
|
cannot pass catheter into stomach
drooling choke when feed polyhydramnios |

Signs :
POLYhtdram esoph atresia tachynea DX: use radioopague feeding tube barium swallow Is assoc with esoph atresia so suspect it. Most common is Type A but in ED see type H |
|
|
in first few days of life
cough, wheeze, dysnpea and cyanosis A congenital lung d/o |
congen lobar emphy
over expanded lung lobe radiolucent CXRL mediastinal shift to other side ! Flat diaphragm RX remove obst and remove lobe |
|

neonatal resp distress
|
Et: broncioles overgrow
neonatal resp distress recur PNA PTX DX CXR in 3 positions CT see air fluid level It increase risk for cancer |
|
|
Gilberts
|
low enz
unconj hyperbili |
|
|
Onset day 3 of life
high unconj bili pale stool no signs hemolysis |
crijir najjir I
AR glut trans gene parents nml serum bili homos : unconj bili in first 3 days life pale yellow stool no signs hemolysis DX: liver biopsy and measure enx level; need new liver VS criijir Najjir II: less severe, normal stool, no kernicterus, nml bili levels treat phenobarn a week |
|

Alagille
|

Etiol : absent or reduction in number of bile ducts due to destruction.
S/S: face broad forehead, small mandible, wide eyes. Present: itchying (bile salts) xanthomas, high cholesterol, neuro comps Ocular abn CV abn: pulm stenosis peripheral Tubulointest nephropathy vertebral defect |
|

|

HETEROTAXY SYNDROME
- AKA situs ambiguous - a visceral malposition and dysmorphism and indeterminate atrial arrangement TYPES - Heterotaxy with asplenia (ie,bilateral right-sidedness) Both lungs have three lobes and bronchi/art set up like right. - Heterotaxy with polysplenia (ie, left isomerism or bilateral left-sidedness) associated anomalies include: - CHD 50% to nearly 100% - Malrotation 89% |
|
|
what hep most common in kids v
|
hep A.
Treat sibs and parents of patient with Ig |
|
|
Hep B :
What are core ag and ab |
HbC antigen :
valuable as appears early and stays when HbS gone. Also Core ab NOT in vaccine only in those who had virus. TREATMENT IN KIDS : INF-alpha end stage can use liver Tx |
|
|
Hep C perinatal ?
Treat hep C in kids ? |
Yes if high titer.
InF a-2b with comp liver dz |
|
|
cushings triad
|
with high ICP a LATE response esp in kids
bradycardia slow HR tachypnea fast RR hypertension |
|
|
Glascow :
when do you need to add moniters and such ? |
CLIPP:
Below 8 consider CV and ICP moniters |
|
|
In case lead poisening labs to order ?
|
serum lead level as numbers guide treatment.
+ iron studies + erythrocyte protoporphyrin (EP). |
|
|
poisen control number national ?
|

|
|
|
lead levels to treat ?
chelation agents ? |
LEVELS :
-over 10 toxic - over 45 treat w/ chelation in 48 hours - over 70 Hx and chelate - 100-150 acute encephalopathy CHELATION DRUGS - oral: 1st line succimer (?DMSA) and penicillamine 2nd line as AE lupus - IV : dimercaprol (BAL) and CaEDTA USE BOTH BAL and CaEDTA as concerns that CaEDTA monoTx dislodges and might send lead to brain making enceph worse ! - if poop with lead flakes use laxtive hyperosmotic agent first |
|
|
AAP lead screening reccs
|
Live house pre1950 ?
House 1978 with construction ? Test cap blood 9-12 months and at 2 years. For WIC need 2 tests |
|
|
CLIPP case Key Findings
WHAT IS DIFFERENTIAL ? *-altered mental status * afebrile * no focal neurological findings * disrupted social environment * papilledema |
Toxin/Ingestion - usually produce diffuse encephalopathy. without focal signs- A chaotic social environment can increase the risk
Lead Intoxication - anemia, basophilic stippling and constipation in child with radiodense material in rectum points to this diagnosis. The presence of cerebral edema and acutely altered mental status make acute lead poisoning most likely. ****Metabolic causes of increased ICP include Reye's syndrome, liver failure, and electrolyte disturbances, which usually cause diffuse encephalopathies, and are unlikely to present with focal findings or fever. - Increased ICP typically can present with altered mental status and papilledema. Trauma - head trauma can lead to either diffuse brain injury or focal pathology (e.g. epidural or subdural hematomas). - Children with epidural or subdural hemorrhages more likely to have focal neurologic findings. - Non-accidental trauma (abuse) can cause brain injury including subdural hemorrhages producing increased ICP and papilledema. Achaotic social environment makes consideration of abuse important. Mass Lesion - Any space-occupying mass lesion can ultimately cause altered mental status and papilledema, ***however only about a third of patients have these findings at presentation.*** - The presence of focal neurologic findings (ataxia, gait disturbance) should always prompt consideration of mass lesion. Meningitis - usually presents with altered mental status (irritability, lethargy, coma) and fever. Signs of meningeal irritation such as nuchal rigidity, Kernig or Brudzinski signs may only be present in 60% of patients with bacterial meningitis above 1 month of age. - Both focal findings and papilledema rare. - Papilledema should prompt consideration of other diagnoses. |
|
|
Most Common Causes Altered Mental Status in 2-year-old:
|
meningitis, encephalitis,
ingestion/toxin exposure, trauma (accidental and non-accidental), seizure disorder. CLIPPP |
|
|
"approach to fussy infant"
|
CCHMC Hamilton Schwatrz
SPITFACE SVT, SBI (men, PNA, sepsis, UTI) P: phy abuse (fracture, ICH) I : intussection, incarc hernia, intol of formula T: torsion (ovary or test) tornequet (hair) F: for body A: acute abdomen (malrot, volv) anom L Cor Art C: cong heart dz, CHF, Corneal abrasion, colic (dz exclusion) E : electrolyte disturb (hypogly) error of metab |
|
|
Peds lab values that differ from adults
|
CREATININE mg/dl
.....infant 0.2-0.4 .....child 0.3-0.7 .....adol 0.5-1.0 .....adult man 0.9-1.4 women 0.7-1.3 PHOSPHOROUS mg/dl .....10d-2 years 4.5 - 6.7 .....2 yrs - 12 years 4.5 -5.5 .....12 yrs - 18 yrs 2.7 - 4.5 .....over 18 yrs 2.5 - 4.8 POTASSIUM ...infant 4.1 - 5.3 ...child 3.4 - 4.7 ....adult 3.5 - 5.1 Blood count - not on this card alk phos not here Refs: ttp://clinicalcenter.nih.gov/ccc/pedweb/pedsstaff/pedlab.html which refs Harriet lane 16th ed |
|
|
Peds
management low K |
Potassium
• Normal value 3.3-5 mmol/L BUT UP TO 6 ok. • Replacement: • For chronic or ongoing losses, oral therapy or a slow replacement is preferred (e.g. 1 liter normal saline with X mEq KCl or K-acetate- maximum concentration is 80 mEq potassium in 1 liter) • Bolus IV KCl generally not needed unless potassium <3.3 mmol/L • Maximum infusion rate is 10 mEq/hour if weight over 20 kg, and 0.5 mEq/kg/hour if weight under 20 kg. Ref NIH clin peds resources |
|
|
teaspoon =
ounce = |
5 mL = 1 teaspoon
30 mL = 1 ounce |
|
|
Diff Dx apnea infants
|
Apparent life-threatening event (ALTE)
Respiratory illness Sepsis Seizure Gastroesophageal reflux Breath-holding spells Central nervous system dysfunction Cardiac arrhythmias ReF: CLIPP cases |
|
|
*Creatinine Clearance
|
*Creatinine Clearance = (Urine Cr x Urine volume x 1.73)/(Serum Cr x minutes x BSA)
|
|
|
Body Mass Index
|
Body Mass Index (kg/m2) = wt(kg)/ [ht(cm)]2
|
|
|
Normal rectal temp ?
fever/hyperthermia ? hypothermia ? |
Under 96.5° F hypothermic
Over 100.4° F fever / hyperthermic |
|

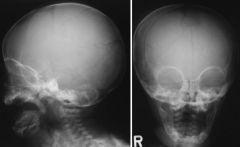
What kind of head injury ?
What kind of trauma ? fall off bed ? birth ? A CLIPP case. |
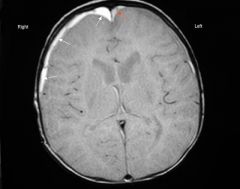
Sub-dural hematoma (rupture bridging veins) as from shaken baby.
above same brain but MRI. has 2 sub-durals. Can be from a fall, but rarely from less than 4 feet. More like MVC. Can occur with forceps/vacuum birth but gone after 4-6 weeks. |
|
|
shaken baby aka abusive head trauma
|
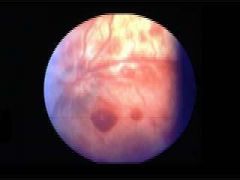
Shaken Baby Syndrome
- 10-12% of all deaths among children who are victims of child abuse due to syndrome. Mortality rate is 25%, and 20-40% with poor outcomes due to neurological injury. - Injury is due to violent shaking or shaking and throwing. Increased risk: retardation, motor delay or extreme motor deficit, partial or total blindness and seizures. - Victims of shaken baby syndrome often have no other signs of physical abuse. Signs and Sxs - constant crying, stiffness, sleeping excessively, unable to wake up, seizures, dilated pupils, decreased appetite, blood spots in eyes. Risk Factors - young parents with social stresses who make frequent doctor visits for seemingly minor problems, and have a lack of impulse control and poor coping skills. * 10-12% of all deaths among victims of child abuse. * mortality rate is 25%, * morbidity is 20-40% : risks for retardation, motor delay or extreme motor deficit, partial or total blindness and seizures. Victims of shaken baby syndrome often have no other signs of physical abuse. Diffuse retinal hemm confirm shaken baby but lack of them does not excl it. If baby has subdural that already confirms non-accidental trauma. |
|
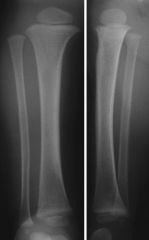
limping 20month old
What is it ? |
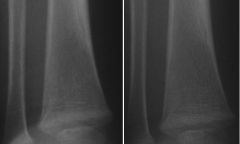
non displaced fracture of distal tibia.
"toddlers fracture" suggests abuse as this kid is not walking yet. |
|
what happened ?
7 month old with bump on head ? |

Multiple fracture lines parietal and occipital.
Suggest abuse not fall off couch. A fall off couch would have one fracture line. Above CT : ** CAREFUL hole at top is ant fontenalle !! At sides is two fracture lines At left is SUBGALEAL hematoma |
|
|
How might newborn with arrhythmia present ?
|
dec feeding
irritability - Apnea uncommon in arrhythmias, but decreased feeding and irritability or lethargy are common. - Severe bradycardia, marked supraventricular tachycardia or prolonged QT syndrome could present this way. CLIPPP |
|
|
What is colic ?
|
Colic - syndrome of crying several hours/day, usually after 5 p.m., 5 nights/week or more. Baby comforted only by holding or rocking.
- Crying starts after 2 weeks of age and generally lessens by 2 months of age. May continue until age 3-4 months. - Infant eats normally and has normal growth. - The crying can create feelings of rejection and anxiety in caregivers. CLIPPP |
|
|
SIDS vs Apnea vs ALTE
|
ALTE/Apnea and SIDS
Apparent Life-Threatening Event - replaces "near-miss SIDS" (sudden infant death syndrome). Event frightens the observer and includes color change, change in tone, and possibly choking or gagging. Apnea - cessation of inspiratory gas flow for 20 seconds, or for a shorter period of time if accompanied by bradycardia (HR <100 bpm), cyanosis or pallor. - most common problem of ventilatory control in preemies. SIDS - In U.S., leading cause of death among infants 1 month to 1 yo. Highest incidence in infants 6 mos old. - Risk Factors - stomach sleeping, African-American, Native Americans, male. - Potential Risk Factors - smoking, drinking, or drug use during pregnancy; poor prenatal care; prematurity or low birth-weight; mothers younger than 20; smoke exposure following birth. CLIPPP |
|
|
RF child abuse
|
Risk Factors of Child Abuse
- Perpetrators often exhibit impulsive behavior, may have been abused themselves as children, and are experiencing stress without family or social support. - No correlation between incidence of child abuse and abusers' race or ethnicity; abuse occurs at every socioeconomic level. - Single mothers and families with large numbers of children at increased risk. CLIPP Also kids with devel delay or special needs. |
|
|
ICP what is normal !!!
|
ICP
Normal newborn 6 mmHg children 6-13 adol/adult 0-15 High ICP in baby-toddler may see fat head. |
|
|
migraine in kids
|
Unlike adults :
aura more paresthesia, rarely visual. 90% fam hx most bilateral incl w/u high ICP causes Rx: caff, triptans, ergots Prophy 2x/month : valproate, TCA, BBl, CCB, topiramate Diff from tension: tension rare before puberty, in tension rarely N/V |
|
|
cluster headache
|
conjunctivitis , uni stabbing
acute : O2, steroids prophy Li or CaCh blocker |
|
|
treat high ICP
|
hypervent post intubate (works 30 minutes)
raise head 15-30 degrees mannitol ** moves fluids to INTRAVASCULAR compartment |
|
|
kid aneurysms
|
Age: under 2, over 5
Dz: ehlers, co-arc, polycytic kidney How present: SAHemm Dx: angio gold standard Rx: clip or coil Unlike adults kids more often vertebrobasilar 23% vs 12% but still most circle willis |
|
|
Kid AVMs varients
* vein of Galen * cavernous hemang * venous angiomas |
**Vein of Galen malform
CRANIAL BRUIT as large shunt. As infant high output CHF and FTT and often have heart murmur. 50% die. ** cavernous hemangioma low flow AVM and leak slow, present as seizure, MRI "popcorn", only sx if symptoms ** venous angiomas rarely issue, can sz if seizures |
|

Name term ?
|
Spasticity results from a lesion that involves upper motor neuron tracts and may be unilateral or bilateral. Rigidity, the result of a basal ganglia lesion, is characterized by constant resistance to passive movement of both extensor and flexor muscles. As the extremity is undergoing passive movement, a typical cogwheel (caused by superimposition of an extrapyramidal tremor on rigidity) sensation may be evident. The rigidity persists with repetitive passive extension and flexion of a joint and does not give way or release, such as with spasticity. Children with spastic lower extremities drag the legs while crawling (commando style) or walk on tiptoes. Patients with marked spasticity or rigidity develop a posture of opisthotonos, in which the head and the heels are bent backward and the body bowed forward
Nelson Peds |
|
|
floppy infant ? has what ?
|
Hypotonia refers to abnormally diminished tone and is the most common abnormality of tone in neurologically compromised premature or full-term neonates. Demonstration of hypotonia may reflect pathology of the cerebral hemispheres, cerebellum, spinal cord, anterior horn cell, peripheral nerve, myoneural junction, or muscle. An unusual position or posture in an infant is a reflection of abnormal tone. A hypotonic infant is floppy and may have difficulty in maintaining head support or a straight back while sitting. Such infants may assume a frog-leg posture in the supine position and have significant head lag during the traction response. Premature infants of 28 wk of gestation tend to extend all extremities at rest, but by 32 wk there is evidence of flexion, particularly in the lower extremities. A normal full-term infant's posture is characterized by flexion of all extremities.
Nelson Peds |
|
|
ataxia ?
|
Truncal ataxia is characterized by unsteadiness during sitting or standing and results primarily from involvement of the cerebellar vermis. Abnormalities of the cerebellar hemispheres characteristically cause intention tremor unaffected by visual attention. Ataxia may be demonstrated by the finger-to-nose and heel-to-shin tests, by heel-to-toe or tandem walking, and, in infants, by observation of reaching for or playing with toys. Additional abnormalities associated with cerebellar lesions include dysmetria (errors in measuring distances), rebound (inability to inhibit a muscular action, such as when the examiner suddenly releases the flexed arm and the patient inadvertently strikes the face), and disdiadochokinesia (diminished performance of rapid alternating movements). Hypotonia, dysarthria, nystagmus, and decreased deep tendon reflexes are common features of cerebellar abnormalities. Sensory ataxia is found with diseases of the spinal cord and peripheral nerves. In these disorders, the Romberg sign is positive (patient is unsteady with eyes closed, but not when they are open), and there are often related sensory findings including abnormalities in joint position and vibration sense.
nelson peds |
|
|
chorea in kids
|
Chorea is characterized by irregular involuntary movements of the major joints, trunk, and the face that are rapid and jerky. Affected children are incapable of extending their arms without producing abnormal movements. They have a tendency to pronate the arms when held above the head. The hand grip contracts and relaxes (milkmaid sign), the speech is explosive and inarticulate, the deep tendon reflexes of the knee are “hung up,” and patients may have difficulty in maintaining protrusion of the tongue.
nelsons peds |
|
|
dystonia and athetosis ?
|
Athetosis is a slow, writhing movement that is often associated with abnormalities of muscle tone. It is most prominent in the distal extremities and is enhanced by voluntary activity or emotional upset. Speech and swallowing may be affected. Chorea and athetosis are the result of basal ganglia lesions and are difficult to separate clinically. Both may be prominent in the same patient. Dystonia is an involuntary, slow twisting movement that primarily involves the proximal muscles of the extremities, trunk, and neck. Nelsons Peds
|
|
|
kids DTRs.
* extra : crossed adductor response |
The knee jerk in an infant may produce a crossed adductor response (tapping the patellar tendon in one leg causes contraction in the opposite extremity), which, if present, does not become abnormal until 6–7 mo of age. The deep tendon reflexes are absent or decreased in primary disorders of the muscle (myopathy), nerve (neuropathy), and myoneural junction and in abnormalities of the cerebellum. They are characteristically increased in upper motor neuron lesions. Asymmetry of deep tendon reflexes suggests a lateralizing lesion.
Nelson Peds |
|
|
Babinski kids and newborns
|
The plantar response is obtained by stimulation of the external portion of the sole of the foot, beginning at the heel and extending to the base of the toes. Firm pressure from the examiner's thumb is a useful method for eliciting the response. The Babinski reflex, indicating an upper motor neuron lesion, is characterized by extension of the great toe and by fanning of the remaining toes. Too vigorous stimulation may produce withdrawal, which may be misinterpreted as a Babinski response. Most newborn infants show an initial flexion of the great toe on plantar stimulation. As with adults, asymmetry of the plantar response between extremities is a useful lateralizing sign in infants and children.
|
|
|
tonic neck reflex
|
The grasp response is elicited by placing a finger or object in the open palm of each hand. Normal infants grasp the object, and with attempted removal, the grip is reinforced. The tonic neck reflex is produced by manually turning the head to one side while supine. Extension of the arm occurs on that side of the body corresponding to the direction of the face, while flexion develops in the contralateral extremities. An obligatory tonic neck response, by which the infant remains “locked” in the fencer's position, is always abnormal and implies a CNS dis-order.
Onset : 35 weeks Full: 1 month Duration: 6-7 months |
|
|
parachute reflex
|
The parachute reflex is demonstrated by suspending the child by the trunk and by suddenly producing forward flexion as if the child were to fall. The child spontaneously extends the upper extremities as a protective mechanism. The parachute reflex appears before the onset of walking.
onset: 7-8 months Full at : 10-11 months remains thru life |
|
|
Moro
|
Moro reflex is obtained by placing the infant in a semi-upright position. The head is momentarily allowed to fall backward, with immediate resupport by the examiner's hand. The child symmetrically abducts and extends the arms and flexes the thumbs, followed by flexion and adduction of the upper extremities. An asymmetric response may signify a fractured clavicle, brachial plexus injury, or a hemiparesis. Absence of the Moro reflex in a term newborn is ominous, suggesting significant dysfunction of the CNS.
MORO onset 28-32 weeks Full 37 weeks duration 5-6 months |
|
|
walking like a toy soldier
|
The spastic gait
|
|
|
waddling gait
|
waddling gait results from weakness of the proximal hip girdle. Affected children often develop a compensatory lordosis and have difficulty in climbing stairs.
|
|
|
clumsy, tentative gait
|
Weakness or hypotonia of the lower extremities may result in genu recurvatum and flat feet, which causes a clumsy, tentative gait.
|
|
|
CI to LP
|
Contraindications for performing an LP include: (1) elevated ICP owing to a suspected mass lesion of the brain or spinal cord, (2) symptoms and signs of pending cerebral herniation in a child with probable meningitis, (3) critical illness (on rare occasions), (4) skin infection at the site of the LP, and (5) thrombocytopenia plt under 20
|
|
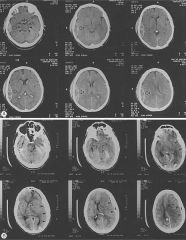
what does A have ? What does B have?
|
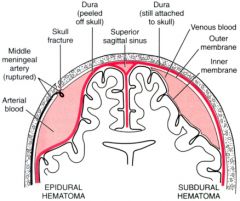
A has epidural, assoc MMA and skull fx often
B has subdural, see with shaken baby, bridging veins |
|
|
why do kids stroke ?
mgt ? |
kids stroke : thromboemb from heart abn
- art emboli ( trauma to int carotid like pencil to mouth, often see seizures as little clots shed) - retrophar abscess - heart : myxoma, arhhy, PFO, bact endocarditis VENOUS clots septic, dehy, pro-coag abn NEONATES : diff neuro signs seizures with ICH W/U: CT/MRI head, angio, if nothing then heart ECHO next. |
|
|
coup vs countre coup
|
coup : hit with bat (accelleration injury)
coutre coup : decelleration, fall down stairs |
|
|
Epi vs subdural
uni vs bila ret hemm vs not fx versus not |
EPI: lentil shape
uni lateral MMA - temp bone no retina hemm high death, low morbidity/injury if live SUB: concave hugging shape bilat, shaken baby retina hemm more often seizures high morbidity - injury |
|
|
diffuse axonal injury - how to see it ?
|
T2 MRI as only 10% of CTs show abn
|
|
|
CSF flow path and where blocked.
|

CSF lat ventricle
Foramen Monro 3rd vent cerebral aqueduct **Obst NonCom** 4th vent * kids-ChiariII, dandy,posttumor* for magendie and luscheka subarach space cord and brain arachnoid villi where reabsorbed **nonObst/comm hydroceph in adults/neonates post intrauteroinfections |
|

causes of aqueduct stenosis ?
|
* familial and x linked
* NF * meningitis |
|
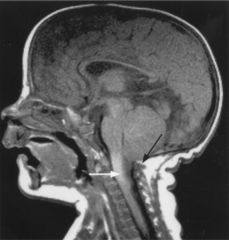
Name it ?
|
Figure 592-11 A midsagittal T1 weighted MRI of a patient with type II Chiari malformation. The cerebellar tonsils (white arrow) have descended below the foramen magnum (black arrow). Note the small slitlike 4th ventricle, which has been pulled into a vertical position.
|
|

Name
|
chiari I
|
|

|

Figure 28-2 Examples of several posterior fossa anomalies. A midsagittal MRI (A) and photograph (B) of a brain with Dandy-Walker malformations. The cerebellar vermis is rotated anteriorly and there is a cystlike dilation of the fourth ventricle. C, A Chiari I malformation is characterized by a tongue of cerebellar tonsils extending over the cervical spinal cord. The cerebellar vermis is intact and shows no displacement. D, The Chiari II malformation is characterized by the cerebellar vermis extending as a tongue of tissue into the cervical spinal canal. The inferior vermis is white, corresponding to the extreme gliosis usually seen in this disorder. Note the beaking of the inferior tectum, the elongated and distorted pons and medulla, with the kinking of the lower medulla.
|
|
|
brain biopsy has Rosenthal fibers ?
|
Rosenthal fibers :
cerebellar astrocytomas AND "Alexander's disease" progressive leukodystrophy w/ MR, spasticty, and megaloencephaly |
|
|
Alexanders disease
|
"Alexander's disease" progressive leukodystrophy w/ MR, spasticty, and megaloencephaly
brain has Rosenthal fibers |
|
|
Kids post fossa tumors
S/S |
First symptoms usually change personality
high ICP : papilledema, headache, N/V, gait classic: nystagmus hydropceph |
|
|
Kids post fossa tumors types
|
Glial cell tumors
--- astrocytoma #1 : often cystic, Rosenthal fibers, Rx sx resection, over 90% survive --- ependymoma : IN 4th vent and cause hydroceph, Tx with removal and rad, 5 yr surv 50% ** Meduloblastoma only in kids is PNET #2 and in kids under 7yrs psuedorosettes, deep nuclei scant cytosol In 4th V and spreads w/ "drop mets" So sx and radiation/chemo, surv 80% vary with disemm |
|
|
craniopharngioma
|
Signs :
shortness endo probs tumors grow slow cannot often remove whole thing Dx: 90% calcified on CT but image with MRI PreOP do visual field test and endo studies |
|
|
NF1
what kind of CNS do they get more than NF2's ? |
NF1
most common 90% ch 17 About half NEW muts -- so screen before telling parents about risk to future children. S/S: 6 cafe au laits of 5 mm in kid pre puberty ( after that 15mm) freckle arm pit; 2 lisch haratomas, 2 NF, osseus lesion, OPTIC GLIOMA, Common: seizure, learning disabilities, Pts higher risk seiz and CNS tumors |
|
|
NF2
|
NF2 chr 22
less common 10%, teen onset bilat ac neuroma parent/sib : NF, meningioma, glioma, schwannoma, MULT CNS tumors much more than NF1 NO cafe au lait and no freckles |
|

Name disease ? What would you scan next ?
|

Tuberous sclerosis
AD 1/2 spont muts brain tubers with Ca go into vents cz hydroceph and kids have seizures. Gene: tuberin TSC1 and 2 #1 cause infantile spasms On face aden seb appear age 4-6 are hamatomas 50% heart abn like myxomas Common kidney haramtomas: adomyolipomas |
|
|
neuroblastoma
|
From neural crest. Can be anywhere with SYM neurosystem
"opsoclonus-myoclonus" is sign dancing eyes- dancing feet #1 tumor in infants : often cervical, thoracic region, can see Horners. In older more diss abdominal, adrenal, retroper ganglia 95% VMA Scan MIBG If infantile even if stage 4 good prog Histo: sm round blue cell some neuron diff Signs : |
|
|
teen with syringomelia
|
Do MRI
think chiari type I cerbellar tonsilar herniation thur for magnum VS More common Chiari II assoc with cervical meninomyelocele, cerebellum and medulla shifted and medulla kinked, |
|
|
Dandy walker
|
failure 4th vent roof
huge cyst of a 4th vent infants gets a really fast growing head with hydropceph tx shunt often agenesis cer vermis, c callosum |
|
|
no corpus collpsum
|
* normal
* see in lissencephaly (smooth) which die early - normal intell * ARchairi II and Dandy OFTEN * Aicardi syndrome X dominent : girls only, nml until at 3 mnths infantile spasm, retina "lacunae" (specific!), no c. call. Can see brain cysts. FIRST AID and Wiki for Aicardi |
|
|
How localize brain tumor.
CLIPP |
supratent :
focal : motor weak, sens changes, speech, seiz, reflex abn Infratent (cerebellum or block 4th vent): nyst, N/V, papilledema, vision changes and nystagmus stem: CN gaze palsy, hyperreflexia, clonus, hemiparesis Cord: bowel, back or radic issues |
|
|
what kid gets intra cerebral hemm and what are signs ?
CLIPPP |
Premie
focal neuro signs seiz |
|
|
Why would you think a h/a is an AVM not a migraine ?
CLIPPP |
AVM: stays one one side, h/o seizures, when ruptures a BAD h/a with vomit, nuchal ridgid, progressive LOC. hemiparesis and local-gen seizure.
Migraine: bilat |
|
|
Gonads
Wolff vs Mullerian AND how do you get a teste ? |
Wolffian: epididymis, vas def, seminal vesicles
TESTES make ANTI-MULLERIAN Mullerian is default -> fallopian, UTERUS, upper vagina How get testes: With SRY gene with ovary becomes a testes |
|
|
Hypospadia that makes you think maybe female ?
|
with separation scrotal sac
(of course bilat undescended testes) |
|
|
Bilat cryptorchidism with phallis - what is it ?
|
boy
OR CAH female with severe virilization. With all CAH there are abdominal gonads/normal ovaries. So if you can palpate a gonads - it is not CAH. |
|
|
Size of penis, clitoris for ambiguous genitalis
|
2 cm penis
female over 9 mm long width 6 mm |
|
|
Labs for ambig genitalia
|
Classic 21 hydroxlase :
* high 17 hydprog and andro ALso do renal and lyte panal chromo panal FISH for SRY gene Can do genitogram for pelvis in search for gonads/vagina/FT biochem for test synth, 5alpha test |
|
|
can CAH females have children
|
maybe - have ovaries.
Most other ambig genitalia non fertile |
|
|
Vaccine precautions CDC
DTaP |
If after last DTaP dose
brain or CNS disease in 7 days NonStop crying for 3 or more hours seizure or collapse fever over 105F |
|
|
Polio vax is for polio strain 1,2,3
OPV and IPV to same strains |
When: 2m, 4m, 6-18M, 4-6Y
IPV: SQ ! (so is c pox) CI : life threat allergy neomycin, streptomycin, polymyxin B AE: VAPP vax assoc paralytic polio with Oral vax is 1 / 760,000. With IPV reduced by 75-90% but NOT ZERO. |
|
|
CDC precautions
Vax HepB |
life threat YEAST allergy
|
|
|
CDC precautions
Rotavirus |
weak immune system
ongoing digestive probs recent blood transf ever intussception |
|
|
How take temp kids
|
rectal best under 3 YRS
Mouth OK 4-5 YRs EAR babies axillary 3 Mnths |
|
|
When to call clinic after vax
|
Fever or fussy over 24 hrs
pale or limp crying over 3 hrs and wont stop high pitched odd cry seizure/shaking/jerking marked dec responsiveness |
|
|
Kids fever remedies
|
Infant drops 0.8 mls = 80 mg
...For 10kg OR 2-3 year old : ...Give 160 mg or 1.6 mls Child liq or susp 1 tsp ( 5ml) = 160 ml Give 1 tsp child tablet = 80 mg Dose every 4-6 hours PRN, no more than 5 times in 24 hours. IBUPROFEN Give 6-8 hours PRN, no more than 4 x in 24 hours Infant drops 1.25 mls = 50 mg 10 kg 1.8 ml Child susp 1 tsp = 100 mg 10 kg kid give 1 tsp child tab = 50 mg |
|
|
My kid got a vax 2 days ago and now has :
fever (1 of 4) red swollen leg fussy (1in3) I'm worried as when my neighbors kid got this same shot they had : jerking and staring (1/14000), cried for 5 hours straight, fever of 105 ! |
DTAP
Given at 2 M 4M 6M 15 - 18M 4-6 Yr |
|
|
Risks of Hib vax ?
|
1 of 4 red, warm swelling at site.
1 of 20 : fever over 101F can last 2-3 days. Given w/ DtaP, PCV, IPV 2M 4M 6M 12M-16M |
|
|
My HPV vax itches ? a big deal ?
|
HPV
itching at site in 1 of 30 pain red or swell 1 of 4 fever 100 1 of 10 fever 102 1 in 65 |
|
|
MMR AE
ages given |
MMR given : 12-16 M, 4YR
mild and in week 1 fever 1 of 6 mild rash neck gland swell Moderate jerk and staring (seiz) 1 of 3000 temp pain stiff joint in adult teen women ** temp low plts and bleeding disorder ** SEvere allergy under 1 in million Unk incidence and link: deaf, LT seiz and unconsc, brain damage |
|
|
meningitis vax
|
more pain and red with
MCV4 vs MPSV4 GBS: reports after MCV4, unk link |
|
|
pneumococcal vax
|
PCV7 conjugate vax for BABIES
Ages: 3 doses 2 months apart 2M, 4M, 6M, then 4th dose 12-15M Also high risk kids over 2 yrs. 1 in 4 red swell tender 1 in 3 : fever over 100.4F 1 in 50 fever over 102.2F some fussy, drowsy, loss appetiteNo severe rxns CI:usually defer in preg OLDER PPV23 polysacc Who: not indicated for kids under 2. Given to high risk kids. half red, pain (more vs PCV7) Under 1% fever (less) rare severe all rxn |
|
|
RAbies vax AE
|
30-74% sore red swell itch
5-40% h/a, abd pain, myalgia, dizzy with boosters ~ 6% hives, pain joints, fever Illness resembling GBS but with complete recovery. RARE |
|
|
Rota vax
|
Rota
1-3% mild temp Diarr / vomit no mod/sev rxnx New vax |
|
|
shingles vax
|
1 in 3 sore itch red
1 in 70 headache ! |
|
|
smallpox vax
|
mild
...rash 2-4 days ...LN swell for 2-4 weeks post blister heals ...70% kids fever over 100 vs 17% adults ...1 in 1000 secondary blister Mod-Severe ...serious eye inf and blind ...whole body rash ..encephlitis and risk perm brain damage high as 1 in 83,000 ...severe infect starts at vax site 1 in 667,000 mostly in those with poor imm fx ...DEATH 1-2 per million, mostly those weak imm system *** For every million vax, 14 to 52 could have life threat rxn. Another person TOUCHING site can cause reaction. |
|
|
Tdap
AE |
New for adults and adol
AE clinical trial pain in most red swell 1 in 5 mild fever 100.4 1 in 25 adol 1 in 100 adults headache 40% adol 30% adults tired 30-40% N/V/D 10% adult 25% adol MODERATE fever over 102 worse pain or red, worse stomach ache, N/V/D SEVERE = sought med attn, cant do oactivities NONE in adol adult had 2 nervous system probs, went away, unsure link severe all rxn under 1 in million which is less than severe rxn chance if get dz CDC and vax sheets |
|
|
typhoid vax AE
|
Inactivated shot
fever 1 % headache 3% red swell 7% Live Vax oral 5% fever or headache Rare abd discomfort, N/v, rash |
|
|
Varicella vax
chicken pox who? AE |
ADMIN is SubQ
CI: allergy vax, neomycin, gelatin CI: poor immunity (its live but cell free), on csteroids over 14 days, on salicylate rx, PREGNANT, recent blodo product admin or IG admin in last 5 months NB: do give to kids with HIV unless immsupr Admin schedules ***typ 12-18M (NB: WITH MMR or wait) booster after age 4 *** catch up Over 13Yr 2 doses 4wks apart *** some use as post-exp prophy TYPE vax: cell free live atten VAX AE: 20-35% red, swell 10% fever 1-4% rash like c pox under 1 in 1000 seiz (jerk or stare) very rare PNA Ext rare reports of brain/neuro rxn and low blood count, unsure link CPOX AE: 2nd bacteria, death PNA, enceph, hep, Reye |
|
|
childrens Vax given SQ
|
SQ
chicken pox |
|
|
MMRV vs MMR
|
MMRV high fever 1 in 5 and measles-like rash 1 in 20
versus separate CDC vax sheet |
|
|
yellow fever AE
If I have this go to doctor: high fever, behav change, flu-like 1-30 days post. |
less with booster
25% sore, fever, ache With passive reporting allergy 1 per 131,000 dose severe neuro rxn 1 per 200,000 doses life threat systemic rxn MOFS 1 per 250,000 doses BUT in those OVER 60 1 per 45,000 and in people w/ those rxns half die. CDC vax sheets |
|
|
Anemia screening
|
For WIC with CBC
9M 12M Normal values : 6 mths to 2 yrs hgb 10.5 - 13.5 and MCV 70-[78]-86 Microcytic = under 78 Macrocytic = over 100 RF: low SES, milk before 6M Birth wt under 500g low iron formula used, low diet intake |
|
|
Hgb and MCV birth
|
Birth
Hgb 13.5 - 24 MCV 95 - 121 Then decreases... 1 month hgb 10-20 1-2 M hgb 10-18 2-6 months hgb 9.5 to 14 6m-2 yr 10.5 to 13.5 2-6 yr 11.5 to 13.5 6-12 yr 11.5 to 15 |
|
|
what happens if baby doesnt get vit k shot at birth
|
In 1% babies, esp breast milk
days 2-7 hemmoragic s/s melena hematuria bleed circ site ICH : seiz, low resp, focal hypovol shock Dx: ** high PT as low FII, FVI, IX, X |
|
|
kid anemic
MCV 75 hypochromic LOW ferritin Low TIBC |
IRON DEF
microcytic < 78 hypochromic ** high RDW unlike thallassemia LOW ferritin unlike anemia chr dz + anisocytosis +elipotocytes ** high PLTs |
|
|
anemia and spherocytes
What labs ? |
spherocytes
AIHA : check bili/LDH and direct Coombs AIHA: Macrocytic, normochromic, High RDW, |
|
|
target cell : 2 causes and how to tell
|
target cell
Hgb-pathies : (thal, sickle) normochrom and normocytic MCV adults 80-100, kids 78-100 Look for signs thal (high RBC ct, or sickle) Liver dz: targets, round, echino, acanth nml RDW MACROcytic over 100 as had DNA synth, and normochromic. Post-splenectomy |
|
|
hypothyroidism effect of blood
|
anemia
round RBC macrocytic anemia normochromic |
|
|
Oval RBC
|
hydroxyurea (for sickle)
myelodysplasia w/ macrocytic anemia and teardrop cells in megaloblast anemia MCV over 110 folate and B12 (se eother card) |
|
|
Oval RBC
seg PMNs MCV over 110 |
Megaloblast anemia MCV over 110
and RDW high ** folate def ...low retics, low serum folate, ... HIGH homocysteine *** low serum cobalamine, ....HIGH homo AND methymalonic ACID schilling, low retics |
|
|
How use Mentzer to tell anemias
|
To tell thall vs iron def
Mentzer index = MCV/RBC count Over 13 suggests iron def under suggests thall |
|

What vitamin does she need ?
|
Acrodermatitis enteropathica
Zinc deficiency You need 300 mcg daily if under 3kg, burns, diarr 100 mcg after that UC Davis derm paper online |
|
|
When caution or changes with GI/renal dz ?
Copper Mang Chromium SElenium |
Half needs copper in cholestasis and
D/c manganese Renal insuff : caution chrom, selenium CCHMC pocket |
|
|
Labs in anemia for systemic causes in kids ?
|
LDH for leukemia
LFTs Cr uric acid for liver or renal failure condider BM biopsy, low B12 or folate |
|
|
healthy 1 yr old
has cold now pale, tired won't eat CBC hgb 5 MCV 80 |
Dx: transient erythroblastosis of infancy
Possible link to parvo Get RBC back 30-60 days Transfuse |
|
|
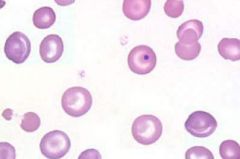
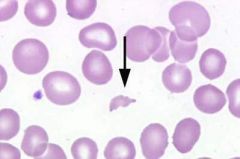
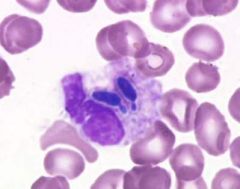
Howell-Jolly bodies
Howell-Jolly bodies are spherical blue-black inclusions of red blood cells seen on Wright-stained smears. They are nuclear fragments of condensed DNA, 1 to 2 µm in diameter, normally removed by the spleen. They are seen in severe hemolytic anemias, in patients with dysfunctional spleens or after splenectomy. |
|

|
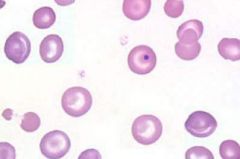
Nucleated red blood cells, (nrbcs or normoblasts), represent the stages of a red blood cell before it matures. Cells of this stage are usually seen in newborn infants, and in patients with responses to hemolytic crises, such as in megaloblastic anemia and iron deficiency anemia. The average size of the normoblast is 7-12 µm in diameter. The cytoplasm is pink. The nucleus is pyknotic (a homogeneous blue-black mass with no structure).
|
|
|
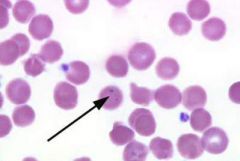
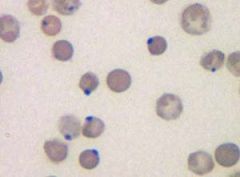
Pappenheimer bodies
Pappenheimer bodies are iron containing granules in red blood cells that are seen because the iron is aggregated with mitochondria and ribosomes. They appear as faint violet or magenta specks, often in small clusters, due to staining of the associated protein. They are associated with severe anemias and thalassemias. |
|
|
|
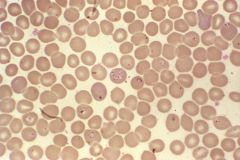
acanthrocyte
excess lipids are in mmb * liver dz * renal failure / uremia * spelic dz * DIc * pyruvate kinase def |
|
|
howell jowell
dense blue nuc frags hemolytic anemia megaloblast anemia hyposplenism post splenectomy |
|
|
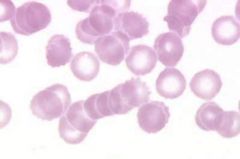
rouleux
MM macroglobemia |
|
|
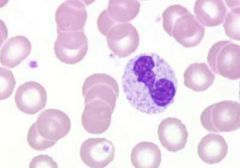
toxic grans
|
|
|
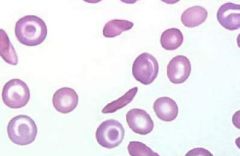
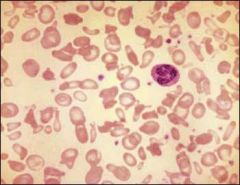
Schistocyte
First AId: microangiopathic hemolytic anemia hemolytic anemias : G6PD DIC HUS vascultits PLUS : severe burns, uremia, aka "bite cells". |
|
|
sickle cell
|
|
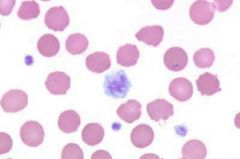
Name white/central cell ?
|
Giant platelet
Giant platelets are platelets that are larger than 6.5 µm, or 75 to 100% the size of a normal red blood cell. A normal red cell is 6-8 µm in diameter. Normal platelets are approximately 1-4 µm, large platelets are approximately 4-6.5 µm. |
|
|
neut eating yeast
|
|
|
heinz bodies
oxidized or denatured hgb abh hgb like post drugs G6Pd |
|
|
Kids iron def anemia
signs treatment |
Mentzer over 13 (MCV/RBC)
cheliosis, spoon nails, esoph web blue sclera, big spleen. ferritin under 10. HIgh PLTs over 600,000 With oral iron should retic in 4 days Use ferrous sulfate and keep for 8 wks post nml hgb 1st aid |
|
|
Iron suppl reccs
|
Term infants
1 mg/kg/day start by 4 months PreTerm need more, 2 mg/kg/day, ma xof 15 per day start earlier, by 2 months 1st aid |
|
|
goats milk in kids
|
folate def
megaloblast anemia |
|
|
folate def in kids
|
Age peak 4-7 months
goat milk VLBW penytoin or MTX Vit C def pregnancy S/S anemia (CHF), chr diarrhea, dont gain wt Labs: serum folate under 5 To check chr levels use RBC folate ! ALso see hyperseg neuts, high LDH, RULE OUT B12 def |
|
|
B12 def
|
strict veg
pern anemia stom bowel sx red beefy tongue premature ag: grey hair, blue eyes, vitiligo weak, anorexia, Myxedema, neuro subacute comb degen Cells: macro-oval RBC neut low and hyperseg, urine methy malonic acid |
|
|
refractory anemia
neutropenia osteoporosis ataxia |
copper def
need copper for RBC, transferrin, hgb Copper in : liver, oyster, meat, fish, whole grain, nuts, legume |
|
|
kid with JRA
normo normo anemia |
anemia chr dz
hgb 7-10 often normo -normo OR hypochr microcytic low serum iron nml or low TIBC high serum ferritin |
|
|
Pyropoikilocytosis
SEvere form of elliptocytosis. One gene for ellito and one for spectrin def. In infancy severe hemolytic anemia (thermal instability). More African descent. Physical examination is remarkable for signs of anemia or, possibly, the effects of ongoing severe anemia, such as frontal bossing, growth retardation, or signs and symptoms of gallbladder disease. Splenomegaly may also be present. |
|
|
intra vs extra vasc hemolysis
|
INTRAVASC HEMOLYSIS
hgb urine hemosiderin urine LOW serum haptoglobin EX: babesiosis, Microang, G6Pd, PNH EXTRAVASC abn RBC shape nml haptoglobin levels big spleen |
|
child, camping in North East
fever anemia dark urine |
Clear Dx: Giemsa stain of thin smear "Maltese cross" as not seen in malaria cross-shaped inclusions (4 merozoites asexually budding)
Trans: Ixodes tick, white foot mouse, blood trans, HAve hgburia as intravascular hemolysis Rx: Treatment with clindamycin* plus quinine or atovaquone* plus azithromycin* are the options. The Medical Letter notes that exchange transfusion has been used. |
|
|
define erythroblastosis fetalis
VS transient erythroblastopenia of childhood |
erythroblastosis fetalis :
AKAhemolytic dz of newborn mom senstive to ABO, rn, kell transient erythroblastopenia of childhood : post cold kid has no RBC and no retics, recovers in 1-2 months |
|
|
newborn
anemic jaundice |
transient hemolytic dz newborn
= erythroblastosis fetalis mom ab to fetal blood Lab findings: High UNCONJ bili Direct Coombs: for ab on babies RBCs fetal hydrops |
|
|
fetal hydrops
|
Mom Rh dz, under 1% hemolysis,
50% no rx, 50% die/kernicteris, 25% hygropic FETAL HYDROPS LARGE placenta rising UNCONJ bili, worse jaund as born and kernicteris abd distended (big spleen and liver) motor bad: limbs adducted, loss of flexion scalp edema, purpura, CYANOSIS Test + direct coombs 1st aid |
|
|
At birth
newborn Hgb F, A, S What can it have ? What is electrophereis finding diagnostic of sickle cell ? |

Newborn screen that can be diagnosic of a SICKLING DISORDER include:
FS sickle OR sickle B thal0 FSA sickle B thal+ FSC sickle and hgb C |
|
|
Hgb sickle biochem
|
beta globin abn
glut acid less soluble in deoxy state low affinity for O2 1:500 AA SIckle cell Carriers 8% |
|
|
Treatment and prophy sickle
|
Pne vax 2 Yr 5 yr
Prophy penny by 4 months old ( sepsis strep pna COD) priapism: exch transfusion |
|
|
Hgb H ?
|
Hgb H = alpha thal with 3 gene deletion
(all 4 Barts) alpha minor = 2 gene deletion carrier silent = 1 gene deletion |
|
|
anemic kid needs trans
big spleen and liver funny skull What is his electrophor ? |
beta thal major
hypo chromic microcytic anemia hgb under 5 low retics ** high LDH as ineff erythropoiesis HGB electrophoresis Hgb F high 30-90% Hgb A2 over 3.5% which is high low to no Hgb A |
|
|
drugs causing hemolysis in G6PD ?
treatment ? when transfuse ? |
aspirin
sulfonamides ciprofloxacin antimalaria fava beans See HEINZ bodies (denatured hgb), bite cells See higher retics High serum bili and LDH (making more RBCs) TREAT: O2, remove trigger, transfuse IF unstable CV, hgb under 6, ongoing hemolysis |
|
|
how many calories do babies need ?
term versus pre-term How much does a term infant gain in weight in a day ? CLIPP |
Term :
100-120 cal/kg/day Term infants gain 20-30 g a day. PreTerm 115-130 VLBW up to 150 |
|
|
plantar grasp reflex
|
touch ball of foot and toes flex
stays until 8 M Has to go away before infant can walk. |
|
|
At 4 months a kid can :
CLIPP |
eat cereal with a spoon
at 4-6 month start to sleep thru night |
|
|
Vit D suppl
|
400 IU needed
breast fed infants need more as only get 25 IU |
|
|
Car seat reccs
|
under 1 year under 10 kg... rear car seat, faces rear
Over 1 y over 10 kg: forward facing car seat Over 4 yrs over 40 pounds (18kg) booster seat Over 8 seat belt Over 12 front seat ok |
|
|
2 month shots vax
CLIPP |
Dtap
IPV Hib PCV PRV HBV #2 Combo: pediarix : dtap, hbv, ipv |
|
|
when does a child reach birth weight ?
double birth weight ? triple ? CLIPP |
double BW 4-5 months
triple 1 year |
|
|
Denver vs bright futures
|
Bright futures: what most kids will do. Is description not a screening test.
Denver is screening test. Documents minimal criteria. |
|
|
When should d/c bottle ?
CLIPP |
12- 15 months
|
|
|
AAP develop landmarks screening
9 months clipp |
bangs 2 cubes in air
cruusing fine motor: plucks pellet with fingertips lang: says any 2 words and nursery rhyme, social: can push arm thru sleeve once started |
|
|
AAP develop landmarks screening
18 months clipp |
imitates pushing cubes
imitates vertival line walks down stairs 1 hand held stack 4 cubes 30 words combines 2 idea/word "dada by" points pics in book regular cup |
|
|
AAP develop landmarks screening
3 years CLIPP |
copies circle
repeats 3 digits alternates feet down stairs broad jumps with 2 feet stacks 10 cubes holds crayon like adult gives full name 2 colors toilet train dry at night takes turns dress with supervision |
|
|
Kid with pidgeon toes?
CLIPP |
There are three causes of intoeing in healthy children. They are metatarsus adductus, * internal tibial torsion +/- excessive femoral anteversion (This cause of intoeing usually shows up in children between the ages of 2 and 4. It can get worse during early childhood. Braces no good).
Can do sx for appearence. |
|
|
CLIPP clinical assess 3 year old
|
gross motor
jump place, kick ball, ride tricycle fine motor copy circle and cross, wiggle thumb social/cog knows name, age, sex, self-care skill, early imag behav lang: knows 2 actions, 1 color, speech half understandable |
|
|
FLACC scale
|
For pain in pre-verbal children
Face 2 months to 7 years Legs - kicking, legs up activity - ached, rigid, jerking Cry - steady scream or sobs Consolobility - hard to sonsole or comfort |
|
|
FACES
|
pictures for for kids 3 years and older
|
|
|
6 and 24 months of age with chronic abdominal pain, abdominal distention, diarrhea, anorexia, vomiting and poor weight gain
|
celiac dz
Dx: IgA tissue transglutaminase IgA antiendomysial antibodies NOt longer test antigliadin ab as nonspecific |
|
|
Kids with H Pylori get what
|
More gastritis than ulcers
|
|
|
anemia
short small head no thumbs hyper pig skin |
Fanconi anemia
|
|
|
Diamond Blackfan anemia
|
presents early infancy
pure red cell aplasia |
|
|
Signs of IBD in pt with abdom pain.
CLIPP |
Red flags are raised to the possibility of Crohn's disease when a patient with abdominal pain experiences any of the following:
1. Pain that awakens the child at night 2. Pain that can be localized 3. Involuntary weight loss or growth deceleration 4. Extraintestinal symptoms such as fever, rash, joint pain, aphthous ulcers or dysuria 5. Sleepiness after attacks of pain 6. Positive family history of inflammatory bowel disease (although only positive in about 30% of patients) 7. Abnormal labs such as heme + stool, anemia, high platelet count or high ESR, hypoalbuminemia 8. Abnormalities in bowel function (diarrhea, constipation, incontinence) 9. Vomiting 10. Dysuria CLIPP |
|
|
functional ab pain in children
CLIPP |
Functional Abdominal Pain - diagnosis of exclusion that should not present with associated abnormalities.
- Most common cause of chronic abdominal pain among children. - Bloody stools rule out this diagnosis. - Growth failure strongly suggests constitutional disease. - Abdominal pain usually nonspecific, not associated with other symptoms, and not life-threatening. - Treatment - reassuring patient and parents. |
|
|
UC
CLIPP |
Ulcerative Colitis (UC) - remitting and relapsing inflammation of the large intestine.
Age - peaks between adolescence and early adulthood (15-30 yo). Signs and Symptoms: - In mild cases - insidious onset of diarrhea, later associated with hematochezia (passage of bloody stools). No systemic findings of fever, weight loss or hypoalbuminemia. - In moderate disease - bloody diarrhea, cramps, urgency to defecate, and abdominal tenderness. Associated findings include anorexia, weight loss, low-grade fever and mild anemia. - Severe colitis - > 6 bloody stools per day, abdominal tenderness, fever, anemia, leukocytosis and hypoalbuminemia. Complications include severe hemorrhage, toxic megacolon or intestinal perforation. - <5% of children with mostly extraintestinal manifestations (growth failure, arthropathy, skin manifestations, or liver disease). Findings: - diffuse, continuous from rectum and extending to colon. Mucosa is friable and erythematous; small ulcerations and pseudopolyps. - UC always affects rectum, with contiguous involvement that can include entire large intestine. Dx - distinguish CD from UC with radiography and endoscopy (upper GI with small bowel follow-through). Treatment - anti-inflammatory therapy with 5-ASA preparations (Sulfasalazine or Azulfidine), mesalamine (Pentasa, Asacol); corticosteroids; immunosuppressive agents (6-mercaptopurine (Purinethol) and azathioprine (Imuran); cyclosporin. Prognosis - 25-40% of patients with ulcerative colitis will eventually require colectomy to treat the disease, but this most often does not occur until adulthood. |
|
|
treatment cronhns
CLIPP |
Treatment - 1st line treatment for mild-moderate CD is mesalamine (5-aminosalicylic acid). May require prednisone; budesonide; antibiotics; immunomodulators (azathiprine, 6-mercaptopurine, methotrexate and cyclosporine); monoclonal antibody (infliximab - brand name: Remicade).
|
|
|
ESR kids
|
androgens lower ESR
1 month - 12 YR old 10-20 mm/hr males over 12 Y 15 mm or less females over 12 yrs 20 mm or less Obese kids higher ESRs 20 vs 10 mm/hr HIGHER ESR in bacteria or myco vs viral or non serious infection Very low w/ DIC |
|
|
leukocytosis in kids
|
WBC
over 11 adults VS Over 20,000 1- 4 week newborns Over 13-15,000 kids 4-16 |
|
|
HIgh LFTs and lnfections
|
staph or strep toxin shock/systemic dz
EBV CMV mono (bili high too) acute hepatitis ( ALT over 1000) half of Kawasaki pts legionella |
|
|
medical futility
|
There is a goal : of medicine, and pts goals
There is proposed action to meet goal, action will not meet goal (determined by MD), virtual certainty action will fail a balence |
|
|
atopic dermatitis
|
baby form: red oozy crusty on face
child/adult: dry, lichenified, itchy plaque antecubital, politeal Rx: topical corticosteroids, Avoid oral ones. No antihistamines. Lubricate skin. |
|
|
cradle cap
|
sebborrheic dermatitis
worse in winter Dx: KOH to rule out fungal Rx: antiseb shampoo, topical corticosteroids. |
|
|
Psoriasis
|
Rare under 10 years old
thick adherent Where: extensor limbs,s trunk, scalp. Nail pits Rx: coal tar, anthralin, steroids, Vit D analog, PUVA (psoralen, UVA), MTX, cyclosporin, |
|
|
lesion with peripheal scale and central clearing
itchy |
tinea
|
|

itchy
|
cut larval migrans
Often dog cat hookworm Ancylodtoma braziliense Self limited or can treat with thiabendazole |
|
|
Neuroblastoma
CLIPP |
abdom mass
anemia CT show calcification, hetro cyst areas and mets HIGH urine VMA HVA in 95% most anemia and cytopenia due to BM mets |
|
|
Wilms
CLIPP |
abdom mass
Age Do renal ultrasound CT shows pseudocapsule - a sharp line bet tumor and kidney Must do chest CT and CXR for lung mets UA shows hematuria |
|
|
How to make formula
CLIPP |
RTF (ready to feed) : as is
powder 2 scoops + 4 oz water (1/2 cup) concetrate 1:1 with water |
|
|
CLIPP
Feeding changes at 9 months |
Need 100 cal/kg/day
about 75% formula/milk about 24 oz day strained food ok finger food ok small bit chicken new food per 5 days No choking foods (popcorn, grapes) |
|
|
when does a kid double their length / height
CLIPP |
2x birth length by 4 years old
|
|
|
hip exam
|
In first 3 months of life
DDH in left 3:1, girls, breech, CAuc and Native Amer, fam hx |
|
|
Ages and Stage ASQ
Denver PEDS CLIPP |
ASQ
Ages infants to 5 screen for devel delays parents do form DENVER II kids 0-6 PEDS parents eval devel status 0-8 behav probs questionaire and dialogue opener |
|
|
Recurrent PNA define
|
2 PNA in one year
OR 3 PNA in life |
|
|
ear infection symptoms
ear discharge anterior displacement of pinna |
mastoiditis -> acute mastoid osteitis
also red and painful over mastoid Dx: CT mastoid Surg eval PE tubes, cut TM, if bone infected need that bone removed IV antibiotics |
|
|
kid 3 years old
fever for 7 days conjunctiva red red lips, palms big ant cerv LN increased PLTS |
KAWASAKI
Most kids under 4 , males UNIQUE FEATURE IS HIGH PLTS peeling fingers and toes sterile pyuria, aseptic men bil conjunct no exudate mucocut lesion : straw tongue, lips dry and red, red/swollen feet or hands rash esp truncal, cervical LN DX: echo and f/u echo Do ESR and CRP RX: IvIg and high dose ASA 1st aid |
|
|
sick
then petechiae then purpura + palms soles no perfusion of finger tips crash in BP fever |
meningococcemia
Dx blood cx, CSF, skin rash Rx: broad abx vanc ceftri until have susc back |
|
|
PNA and then on bactrim.
then conjunctivitis oral ulcers urethritis rash |
Stevens johnsons
prodrome fever, h/a, malaise red rash target lesions infalmed bullous lesions Dx skin biopsy Rx hx, Iv fluids, hyperalimentation |
|
|
pyloric stenosis Dx and imaging signs
|
Ultrasound 90% sens with long pyloric channel
Radiocontrast STRING sign shoulder sign - bulge of pyloric m. into antrum double tract sign - parallel streaks barium into narrow channel |
|
|
pyloric stenosis
PE and metabolic signs |
vomit at 3 weeks
and still HUNGRY and eating and otherwise well. SOemtimes : epigastric peristattic waves felt olive felt hypochol hypokal metab alkalosis Rx pyloromyotomy Dx: u/s |
|
|
bilious vomit after birth
no abdom distention |
duod atresia
half of h/o polyhydraminous 30% Downs Assoc malrot, esoph atresia, con heart dz Rx : decompress stomach, treat life threat anomolies, sx duododemOSTOMY |
|
|
Volvulus
|
gastric : sudden epigastric pain, intractible retching and emesis
With abd xray see giant stomach and air fluid level intestinal: w/ malrotation infant vomit (bile) abd pain early satiety Dx bird beak or air fluid level |
|
|
RF intussecption
|
Most idio
viral entero or rota meckel polyp lymphoma HSP CF |
|
|
triad intussception and other signs
|
triad: colicy abd pain, bilous vomit, current jelly stool (late, absent)
Neuro signs: lethary, shock-like, seiz, apnea RUQ sausage mass "Dance's sign" no bowel in RLQ Abdom xray: paucity bowel gas, loss liver tip, "target sign" two fat circles U/S target or donut |
|
|
intussection
enema rules |
Rule 3's
try 3 times only 3 minutes per try For barium column only 3 feet CI barium peritontis, perf, bad shock Next is OR reduction. Less change recurrence with OR reduction. |
|
|
rectal bleeding in 2 year old
painless vs painful |
painless meckels
painful is intussception |
|
|
First Aid
abx campylobacter |
erythromycin
|
|
|
First Aid
abx E Coli Diarrhea |
SMx-TMP
|
|
|
First Aid Abx
salmonella diarr |
ampicillin or chloramphenicol
OR smx-tmp in infants under 3 months, immunocomp, bactremia |
|
|
first aid
shigella diarr |
tmp-smz or ceftriaxone
|
|
|
first aid
cholera diarr |
tetracycline
or doxycycline |
|
|
strongloides treatment
|
ivermectin
|
|
|
pork worm
myalgia periorb edema PNA heart |
trichinella spiralis
albendazole and prednisone |
|
|
inguinal hernia
|
indirect most common
thru processes vaginalis if do uni repair, 30% get on other side |
|
|
teen
extra teeth , impacted teeth jaw osteomas father died of colon cancer. What does he have? |
Gardner's syndrome AD
* multiple adeno polyps in the colon w/ high malig potential together with tumors outside the colon. * congenital hypertrophy of the retinal pigment epithelium (CHRPE), The extracolonic tumors may include osteomas of the skull, thyroid cancer, epidermoid cysts, fibromas and sebaceous cysts. It is same gene as APC and now merged with FAP |
|
|
FAP when screen ?
|
10 years old do colon scopes
|
|
|
short bowel syndrome ?
|
malab diarr
steattrhea dehyd low Na and potassim ACIDOSIS as loss of bicarb RX TPN, small oral feeds Metro for bug overgrowth |
|
|
indirect hyperbili
retic high |
hemolysis
|
|
|
direct hyperbili
|
hepatitis
cholestatsis error metab CF sepsis |
|
|
liver tumor
|
hepatoblastoma
rare in kids see in Beckwith-Wiedeman (hemihypertrophy) R lobe liver Large aymto mass with big liver Later wt loss, anorexia, vomit, abd pain. DX: AFP level, Rx: sx remove, cisplatin and doxurubicin adjunct -> 90% surv |
|
|
treat echinnococcus
|
albendazole if you cant do sx
|
|
|
what is toddler's diarrhea ?
|
Toddler diarrhea is a common pediatric condition. In infants it is referred to as chronic diarrhea of infancy and in older children as irritable bowel syndrome. Common clinical characteristics include:
1. Age between 6-30 months. Most are better by 4 years of age 2. 2-6 watery stools per day. There can be periods of days without stools. Many stools contain undigested material and may drip down the child's leg from the diaper. 3. Normal weight, height, and head circumference growth curves without falling off 4. No evidence of infection 5. Stools are hematest negative 6. The child looks well and there is no evidence of malnutrition and no history of abdominal pain 7. Growth may be compromised if the diet manipulations that have been tried to control the diarrhea have not been enough calories. 8. There is often a history of colic, gastroesophogeal reflux, and family history of irritable bowel syndrome. |
|

|

Erythema Toxicum Neonatorum
Onset in the second to third day of life, mostly in term babies of lesions characterised by a central whitish to yellowish papule surrounded by a halo of erythema, mainly over the trunk but also in the limbs and face. Lesions may intensify or coalesce particularly in response to local heat. They wax and wane over the ensuing 3 to 6 days. They are benign. Aetiology is unknown. |
|

|
Seborrhoeic dermatitis primarily affects the scalp and intertriginous areas. It is most common in the first 6 weeks of life, but can occur in children up to 12 months of age. Involvement of the scalp is frequently termed "cradle cap", and manifests as greasy, yellow plaques on the scalp. Other commonly affected areas include the forehead and eyebrows (as in the photo to the left), nasolabial folds, and external ears. Involvement of skin creases, such as the nappy area, can lead to secondary Candidal infection and maceration.
The aetiology is unknown. Treatment includes the use of a mild tar shampoo, oatmeal baths, and avoidance of soaps. Occasionally, a mild topical steroid may be indicated. |
|

|
The photos show a typical Mongolian spot with bluish discoloration.
This is a very common benign skin pigmentation occurring frequently in Polynesian, Asian and Mediterranean babies but also, though to a much lesser extent, in Europeans. Although the intergluteal area is the most common site, similar lesions may occur over the trunk or extremeties and at times multiple lesions may be noted. Such lesions have been confused for bruises of child abuse. They gradually fade during the first few years of life. |
|

name newborn rash ?
|
Pustular melanosis
Lesions are present at birth and are characterised by superficial pustules which rupture easily without any actual pus content, leaving a spot of hyperpigmentation. Some hyperpigmented lesions may be present at birth. Any area of the body may be involved. The pustules last for a day or two but the pigmented spots may persist for a long time. Aetiology is unknown. Smears from the pustules reveal polymorphonuclear leukocytes with absence of organisms. |
|

|
lice
|
|
|
trichotillimania vs alopecia areata
|
trichotillomania:
hair shafts broken at diff lengths patchy hair loss, worst at dom hand side and eyebrows/lashes ALOPECIA AREATA autoimm total loss in sharply defined areas short broken off hair ends "excla point hairs" in bald area, High rate regrowth in a year can use steroids topically |
|
|
Rectal prolapse
#1 cause |
chronic constipation
|
|
|
Hirshsprung
vs functional constipation |
Hirshsprung :
no urge to defecate or straining Rarely soiling small ribbon like stools rectum tight narrow and has no stool Functional constipation Large stools in rectal vault rectum big and full of big stool poor sph tone |
|
|
encopresis
|
leak of stool matter
only dx if kid over 4 Usually voluntary with holding (fear defecation) - inc fiber, check fissures can be functional dysmotility -NMus myotonia can be Hirsh rarely, intest pseudoobst anal stenosis metabolic hypothy, low Potassium low Ca |
|
|
Constipation
Rule of 3s |
3 enemas
3 days |
|
|
How does kid with intestinal atresia present ?
|
Born distended abdomen
vomiting bile May/may not pass mec or perf Dx: contrast enema Rx sx anast Unlike esoph atresia where no distension in abd |
|
|
TPN
#1 comp |
* #1 sepsis in 1-5%
* plus clots central vein * placement issues : brachial plexus, perf veins, PTX * the mucosal atrphy can be reversed with oral feeds In clinic PUlm concerns LT with liver abn and high LFTs |
|
|
3 year old
abd pain pica guiac + stools weak and dizzy eosinophilia |
hookworms
Necator Ancylostoma anemia guiac + but rarely h.chemia/melena Rx mebendazole |
|

In Mono Zy
One chorion/placenta - fused or shared But 2 amnionic sacs (one amnion is "siamese"/conjoined twins) |

Twin Twin Transfusion
** Twin on Left: DONOR : Smaller twin ... Oligohydram ..less fluid ....anemia , hypovolemia ** Twin o right RECIP : bigger twin ...more fluid POLYhydram ...plethora AFTER birth : If crit diff over 15 or if bigger twin Hct > 65% = polycythemia and can have hyperviscosity symtoms: resp distress. Smaller twin can have hypovolemia |
|
|
CSF values for neonate ?
|
CSF neonate 0-4 weeks
WBC 0-20 (premie wbc 0-10) ptn under 100 glu over 60% serum Infant over 4 weeks wbc 0-5 ptn under 45 glu over 50% serum |
|
|
CSF for 2 Month old
|
Infant over 4 weeks
wbc 0-5 ptn under 45 glu over 50% serum CSF neonate 0-4 weeks WBC 0-20 (premie wbc 0-10) ptn under 100 glu over 60% serum |
|
|
When Hib vax
|
2M
4M 6M 12M |
|
|
When IPV vax
|
2M
4M 6-18M 4 Yr |
|
|
When MMR
|
12M
4 YR |
|
|
when varicella vax?
|
12M
booster at 4yr |
|
|
What vax's together at 2,4, 6 month visit ?
|
DtaP
Hib PCV7 Polio |
|
|
Dx and Treatment of toddler
barking cough "steeple sign" on radio |
Dx croup w/ upper airway edema
parainfluenza Rx cool mist, fluids Then racemic epi if no resp can use corticosteroids * albuterol no good Blueprints cases. |
|
|
LOWER Airway obst with foreign body:
How to eval ? partial vs total ? which is ball valve and what does that mean ? |
Kid to little : lat decub
Kid co-op : insp and forced expir films. TOTAL OBST: atel and volume loss on bad lung side. On expiration, as good lung empites, heart shifts toward bad empty collapsed side. PARTIAL OBST causes BALL-VALVE w/ local air trapping So, initial INSP view local air trap amidst atel. so HYPER inflated. Then with expir, still air trapping so shift of heart AWAY from bad lung. |
|
|
kid 1 year old
running with unshelled peanuts choking then drool stridor can't really talk |
UPPER airway TOTAL OBST
Under one year flip over arm 5x, then press belly 5x. OVER 1 yr, Heimlich. If partial, can still talk some, let them try to cough it out. |
|
|
infant over 2 months
what % SBI |
2-3% occult bactremia
often S PNA UTI: fussy, no app, non focal exam PNA tachypnea, abd tender, may not cough |
|
|
DIff Dx
infant big head irritable poor feeding hyper reflexia hypertonicity muscle |
hydrocephalus
T2 chiari aqueduct stenosis, tonsils are down w/meninogomyelocele Toxoplasmosis epeneymomas 0-15 yrs, NF2, 4th vent medullloblastomas in cerubellum |
|

kid has port wine nevus
seizures What disorder ? What else worried about ? |
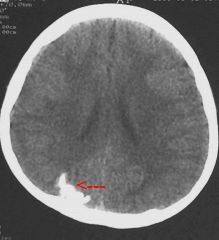
Sturge-Weber (encephalotrigeminal angiomatosis)
port wine nevus on face and ipsilateral cortical atrophy MR seizures hemiparesis hemiatrophy : one leg longer cortical calcification: on CT see gyri calcification in parietal area, and in cisterns, a "tram track" following cortex. |
|
|
congestive heart failure in 2 weeks old
Most common form ? Other forms ? |
#1 myocarditis
dilated vents and LA poor systolic function DIff Dx: glycogen: pompe thick muscle pericarditis w/ eff abberent origen L Cor A (ECG like MI) endocardial firvroelastosis with high voltages in LV |
|
|
Ebsteins abnormality
|
Quadruple heart sound S1 S2 S3 S4
Large RA heart block on R chest leads murmur : systolic (pulmonary area) murmur diastolic LLSB |
|
|
cyanotic diseases
One is exception to R to left shunt rule |
tricispid atresia
which has lg LV and L axis devation as RV hypoplastic Gets picked up in nursery as early cyanosis |
|
|
early cyanosis
nml sized heart CXR: heart like an egg on a string" |
trans great arteries with intact septum
bonus : ECG r axis dev; RVH |
|
|
When do Tof F kids get cyanotic
|
After a few days,
ductal dependent |
|
|
cyanotic kid
CXR "snowman" fluffy venous congestion |
Total anom venous return
below diaph venous congestion as cant get back |
|
|
renal
Ageneis has oligo or poly amnios ? |
renal agensis
HAS oligohydraminos NO fluid pulm hypoplasia death if bilat agenesis |
|
|
accessory renal arteries ?
potential problem ? |
If cut in OR, ischemia.
|
|
|
congen polycystic renal dx
|
Die as child.
|
|
|
Diff billiary emesis
|
REcall
Hirshsprung mec ileus mec plug anorectal malform malrot bowel small left colon syndrome in infant of DM mom maternal med, esp Mag atresia duod, jej, il, colon int duplication |
|
|
horseshoe kidney
|
Ok if fused at top
can halt at IMA inc chance of Wilms See more with Turners |
|

Holt Oram syndrome
|
ADom
ASD (rarely VSD) and carpal bone abn hand bones abn like non-opposable thumb or 3 fingers |
|
this kiddo has a low nasal bridge
is real friendly heart murmur |

Williams syndrome (WS; also Williams-Beuren syndrome or WBS) is a rare neurodevelopmental disorder caused by a deletion of about 26 genes from the long arm of chromosome 7.[1] It is characterized by a distinctive, "elfin" facial appearance, along with a low nasal bridge; an unusually cheerful demeanor and ease with strangers, coupled with unpredictably occurring negative outbursts; a predisposition to violent outbursts; mental retardation coupled with unusual (for persons who are diagnosed as mentally retarded) language skills; a love for music; and cardiovascular problems, such as supravalvular aortic stenosis and transient hypercalcaemia, hyperacousis, elasti gene in some,
|
|
|
8 month old Billy is here for WCC.
Born 26wk gestation. Plot is height, weight, head circum. clipp |
* even tho he's 8 months old CHRONO
Plot at 5 month marker, as 12 weeks early so really 5 months. Usually do this up to 2 yrs when premies catch-up. Can do x----* with X at gest age and line to where chrono age is. |
|
|
Kids language
When say mama when babble when 2 words together ? clipp |
At 6-8 months, the infant has added a few consonant sounds to the vowel sounds, and may say "mama" or "dada" but does not attach them to individuals.
At a year, the infant will attach "mama" or "dada" to the right person. The infant can respond to one-step commands such as "Give it to me." At 15 months, the toddler continues to string vowel and consonant sounds together (gibberish), but may imbed real words. The infant may say as many as 10 different words. At 18 months, a toddler can say nouns (ball, cup), names of special people, and a few action words or phrases. The toddler adds gestures to her speech, and may be able to follow a two-step command. At 2 years, the toddler can combine words, forming simple sentences like "Daddy go." |
|
|
What about milestones in a toddler that is having psychosocial stress ?
clipp |
Most often, a regression in previously achieved behaviors is seen in response to stress. For toddlers, temper tantrums, sleep disturbances and refusal to eat are common adaptations. Language acquisition may be slowed during periods of stress. During hospitalization (an extreme form of stress) children may develop increased dependency, enuresis or encopresis. If a child has recently gained motor milestones and is ill, the achievements may be temporarily lost.
|
|
|
Periventricular leukomalacia (PVL)
what is it ? clipp |
Periventricular leukomalacia (PVL): PVL is the result of damage to the white matter surrounding the ventricles in the brain as a result of hypoxia, ischemia and inflammation. It is correlated with intraventricular hemorrhage (IVH). IVH is bleeding from the delicate vessels of the neuronal and glial proliferation zone (the germinal matrix) that surrounds the lateral ventricles in preterm infants and fetuses. It is likely that damage to the white matter is actually more widespread, but not easily visualized using current clinical imaging techniques. PVL with cysts (cystic PVL) is highly correlated with CP.
|
|
|
Cerebral palsy causes ?
clipp |
MOST idiopathic !!
Premature -> spastic diplegia (periventric white matter abn like PLeukmalacia) ...One subtype of CP, spastic diplegia, is greatly increased in premature infants. A broad range of severity is seen in individuals with spastic diplegia. Lower-extremity involvement causes difficulty with walking and increases the risk for hip dysplasia, scoliosis and calf-muscle shortening. Upper-extremity involvement can cause difficulty in fine-motor tasks such as writing. Some children with spastic diplegia also have cognitive impairments. ~ 10% due to birth asphxia Birth asphix and kernicteris -> dyskinetic CP (athetosis, dystonic) Bganglia, thalamus, abn spastic hemiplegia: unilat UMN stroke so do coag studies Ataxic CP : whole body cerebellar abn spastic quadriplegia : global brain abn |
|
|
Males with small testes and gynecomastia
|
kleinfelter
XXY |
|
|
When might do testing for inborn errors metab ?
What tests ? Clipp |
Infants with some of these disorders may present with lethargy and hypothermia (you must also consider sepsis). Older children may present with lethargy, vomiting and coma, developmental regression or chronic vomiting. Other disorders, such as phenylketonuria, are not usually associated with metabolic exacerbations and can remain clinically undetected until some degree of CNS damage has occurred. This is the reason that newborn screening for PKU was first developed. A careful family history may uncover children with similar presentations or early unexplained infant deaths. Some experts recommend quantitative amino-acid testing on urine and plasma in children with mental retardation and no specific physical findings.
|
|
|
Tests to diag CP ?
clipp |
Diagnosing CP:
- MRI is critical 89% of children with CP have an abnormal MRI - Genetic and metabolic testing should be performed in patients with dysmorphic features, growth failure or developmental regression - Hearing and vision in all - In-depth assessment by a developmental specialist: For an infant, this is often done with a Bayley Scales of Infant Development - Coagulation studies: if hemiplegia, - EEGs: only if there is a history suggestive of seizures. |
|
|
REceptive vs expressive lang better for assesing LT lang outcome ?
clipp |
Assessment: Receptive language (what the child understands) is a better indicator of long-term outcome than expressive language (speech). Ask questions about the child's ability to follow directions, with or without gestures; does the child seem to pay attention; does he hear well? Then ask about words he says and if he uses the words correctly.
|
|
|
define MR
clipp |
Mental retardation/Cognitive disability: Definition of mental retardation has 3 components:
1. Onset before 18 years of age 2. Some degree of cognitive impairment 3. Some degree of impaired adaptive behavior. The most common definition of cognitive impairment is an IQ more than 2 standard deviations below the population mean. Visual deficits or chronic illness can affect IQ measurement. Assessment of adaptive behavior should guide therapy. |
|
|
hyperactivity,
gaze avoidance or autistic behavior young male with suspected MR |
think fragile X
don't have macro-orchidism until after puberty |
|
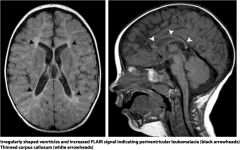
kid can't walk yet and a premie
|
periventricular leukomalacia
extra white FLAIR and T2 by ventricles From ICH as premie Can see cysts too - cystic PVL See small c callosum also common with CP |
|

Where is kiddo delayed ?
|
language
gross motor note white part of line is what most kids can do blue is % kids that cant do it. C is caution |
|
|
downs diag
[clipp) |
karyo type lymphs
Results tr 21 Then know not mosaic (not 100% but unless see mosaicism or phenotype signs of it, say NOT mosaic) |
|
|
Downs well child care
[clipp] |
vision
hearing yearly thyroid All refer cardio : 40% structural heart abn (echo as infant but not used to diagnose) Before sports neck xray CBC neonatal NO MRI needed No need refer hemonc unless have cancer |
|
|
Prenatal testing for Downs ?
samples from where ? [clipp] |
1. maternal serum levels [indirect]
- AFP, hcg, PAPP-A, inhibin 2. Chorionic fluid or amnionic fluid /amniocentesis [direct chromo] : 3. Chorionic villis sample [direct chromo] 4. U/S: nuchal fold, nasal bone, |
|
|
Fragile X syndrome is caused by the expansion of a trinucleotide repeat segment (involving CGG repeats) that is just outside the coding region of the FMR1 gene on the X chromosome. Affected males usually have more than 200 repeats, while normal individuals usually have fewer than 50. Individuals with 52-200 repeats have a premutation that has the potential of expanding to a larger size, perhaps to a full mutation. This expansion is more likely to occur when the gene with the premutation is inherited from the mother, and the larger the size of the premutation, the greater the chance of expansion to a full mutation. There is some correlation between the severity of the mental retardation and the size of the expansion in the full mutation.
Fragile X syndrome is an X-linked trait, and most affected individuals are male. Females with a full mutation range from being asymptomatic to having mental retardation and/or psychiatric problems. Findings in males may include large testes (after puberty), large ears and evidence of a mild connective tissue abnormality (joint laxity, pectus excavatum, flat feet) |
|

|
campomelic dysplasia
|
|

|
ellis von crevald
nail hypoplasia polydactyly asoc heart abn also |
|
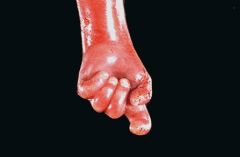
|
tri 18
OVERLAPPING fingers clenched fist MR, prom OCCIPUT, micrognathia, low earsm polydactyly, heart defects, renal malforms, limited hip abduction, rocker bottem feet |
|

tri 13
name and features ? |
A newborn male with full trisomy 13 (Patau syndrome). See cleft palate, inguinal hernia, and postaxial polydactyly of the left hand.
TRI13 TEEN micro ophthal, micro-ceph, MR, heart and renal defect, umbil hernia, cutis aplasia |
|
|
|
thanatophoric dysplasia
peri220.jpg (16446 bytes) Ultrasound may reveal long bones that are shortened. There are several possibilities, including short-limbed dwarfism. Seen here is a radiograph demonstrating short, curved femora and humeri, along with prominent platyspondyly of the vertebrae. This is thanatophoric dysplasia. As the name implies, this is a lethal condition, but it occurs sporadically. |
|

|
thanatophoric dysplasia
Ultrasound may reveal long bones that are shortened. There are several possibilities, including short-limbed dwarfism. Seen here is a radiograph demonstrating short, curved femora and humeri, along with prominent platyspondyly of the vertebrae. This is thanatophoric dysplasia. As the name implies, this is a lethal condition, but it occurs sporadically. |
|
|
what happens to most Turners babies ?
|

|
|
|
47 XXX
|
47, XXX
female 1:1000 Developmental delay and decreased IQ vs sibs abd behav probs taller |
|
|
very high cholesterol
MR toe syndactyly |
Smith Lemli Opitz
AR noo 7 dehydrocholesterol .... |
|
|
47 XXY
|
male
Kleinfelter 1:1000 1% MR and 3% infertility clinics adv mat age |
|
|
47 XYY
|
male
normal newborns normal fertility occ low IQ |
|
|
Kid looks like Roman warrier helmit
|
delt 4p
wolf-hirchorn small head cleft lip and palate common seiz disorders most severe MR |
|
|
Teratogens
tobacco coke fetal hydrantoin |
Tobacco: increases risk low birth wt
Fetal Hydantoin Syndrome: cardiac defects, dysmorphic craniofacial features, hypoplastic nails, & distal phalanges, IUGR, & microcephaly. Mental retardation may be seen. Rare neonatal side effect: methemoglobinuria. - Up to 30% of exposed fetuses may have anomalies; full syndrome occurs in 10% of exposed fetuses. - appears to be compatible with breastfeeding |
|
|
|
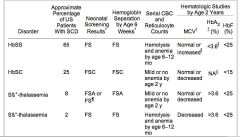
|
|
|
sx common in sickle kids
[clipp] |
tonsillectomies (snoring, OSA)
GB removal as adolescent |
|
|
Why and when penny prophy sickle ?
|
penn to prevent pnemumococal sepsis
Start ages 2 months, STOP age 5. No benefit unless have had sepsis already or had spleen removed. |
|
|
Kid with sickle has a fever.
What do you do ? [clipp] |
Fever may be the only sign of sepsis in children with sickle cell disease and must be dealt with as a medical emergency, with rapid evaluation, blood cultures and institution of broad-spectrum parenteral antibiotics.
The lack of normal splenic function as well as several other more subtle immunologic deficiencies call for this rapid and aggressive approach. |
|
|
vax in kids in sickle
|
23 PNA at 2 yrs
|
|
|
Child with sickle cell starts to have slurred speech and act funny ?
Whats wrong ? How can you screen for this event ahead of time ? |
Evaluation of cerebral blood-vessel flow by Trans Cranial Doppler (TCD) study has been shown to be a useful screening tool for those children with sickle cell disease who are at increased risk of stroke. Chronic transfusion therapy in children with elevated TCD blood flow has been shown to significantly decrease the risk of stroke
|
|
|
acute chest
[ clipp ] |
cute chest syndrome: A recent prospective study of acute chest syndrome (ACS) in patients with sickle cell disease reported 80% presented with fever, 62% had cough, and 44% had chest pain. 48% were admitted for other reasons and developed ACS while hospitalized. Mean O2 sats were 92%. A specific cause was found in 38% (infection or pulmonary fat embolism). Average hospitalization was 10 days. Of these patients, 3% died of ACS or other complications. NEJM 342; 1855, 2000. ACS can develop in children admitted for a painful vaso-occlusive crisis. In this situation, the chest findings may be a result of fat embolism. It is also possible that the findings in the chest result from vaso-occlusion of pulmonary vasculature. It is always difficult to distinguish whether an infiltrate in the lung of a child with sickle cell disease represents an infectious process, pneumonia or atelectasis (pain in the chest or abdomen can lead to difficulty with expansion of the lower lung).
|
|
|
chronic effects sickle cell dz
[ clipp ] |
Chronic: anemia; jaundice; splenomegaly; cholelithiasis; delayed growth and sexual maturation; lymphoidal-tissue hypertrophy involving Waldeyer's ring can cause snoring, obstructive sleep apnea; functional asplenia; cardiomegaly and functional murmurs; hyposthenuria and enuresis; proteinuria; restrictive lung dz; pulmonary HTN; avascular necrosis; proliferative retinopathy; leg ulcers.
|
|
|
crit in sickle cell dz
[ clipp ] |
Baseline Hcts ~18-28%.
|
|
|
kids
normal bp vs hypertension |
up to 90th percentile is nml
Over 95 th percentile is HTN clipp |
|
|
How to quantify proteinuria in children
|
The degree of proteinuria can be better quantified by 24-hour collection or by spot measurements of both urine protein and creatinine. In children it is difficult to obtain accurate 24-hour collections, so a urine protein:creatinine ratio is very useful.
Urine protein (mg/dL) / Urine creatinine = protein:creatinine ratio: <0.2 is normal in children older than 2 years (<0.5 is normal in 6- to 24-month-olds) >1.0 is in a suspicious range for nephrotic syndrome >2.5 is diagnostic for nephrotic syndrome 24-hour collection: - Normal amount of protein excreted is less than or equal to 4 mg/m2/hr - Abnormal: 4-40 mg/m2/hour - Nephrotic range: Greater than or equal to 40 mg/m2/hour clipp |
|
|
in child,
benign causes of proteinuria |
Children may excrete 1+ to 2+ (30-100 mg/dL) of protein during a fever or after significant exertion, which clears after resolution of the fever or exertion. Orthostatic proteinuria is a frequent finding in adolescents and does not signify renal disease. There may be as much as 1500 mg/1.73 m2/24 hours, but protein excretion occurs when the patient is standing, not while recumbent. When the first morning urine is checked it should be negative for protein.
clipp |
|
|
Interstitial nephritis
does it cause ptn uria ? or hematuria ? |
Interstitial nephritis can be associated with red and white blood cells in the urine, but not with this massive degree of proteinuria. In children, interstitial nephritis is rare and usually caused by a medication such as Methicillin (no longer available in the United States), NSAIDs, penicillins, cephalosporins, rifampin, sulfonamides, or infection.
clipp |
|
|
Diff Dx kid with nephrotic syndrome
low comp vs normal w/ hematuria vs not |
nephrotic
LOW comp: lupus, post strep Hematuria too :HSP, IgA nephropathy With HIV, Hep B would see other lab abn (blood or liver) |
|
|
which kids to do renal biopsy
clipp |
Patients who do not respond to steroids with elimination of proteinuria after 8 weeks of therapy are designated "steroid resistant" and need a renal biopsy when medically stable to determine if they have Mesangial Proliferative Disease. Other indications for renal biopsy in patients with NS include:
1) All patients younger than 1 year of age (increased chance of congenital NS); 2) Infants >3 months and <18 months of age with hematuria; 3) Children >10 years of age if the diagnosis is not a drug reaction or postinfectious glomerulonephritis; 4) Children with type I diabetes <10 years' duration; 5) Children of all ages who have hematuria and proteinuria if the mother has hematuria (Alport syndrome); 6) Children with Henoch-Schoenlein purpura; 7) Children with non-postinfectious glomerulonephritis with progressive decline in renal function and urine output; 8) Patients with suspected lupus nephritis with a positive ANA, elevated anti-DS DNA titer, and a decrease in C3 that persists more than 3 months; 9) Patients with steroid-responsive NS who have more than two relapses in a 6-month period (“frequent relapsers"); 10) Patients with a low serum complement at the time of initial presentation not related to acute postinfectious glomerulonephritis; 11) Hypertension at the time of presentation with NS (increased risk for focal segmental glomerulonephropathy); 12) Patients with systemic lupus erythematosus with proteinuria or NS; 13) Evidence of chronic renal insufficiency with persistent elevation of serum urea nitrogen and creatinine. The prognosis is less favorable for mesangial proliferative disease, which causes about 5% of idiopathic nephrotic syndrome. The histology is characterized by a diffuse increase in mesangial cells and matrix. Only about half of these patients will respond to corticosteroid therapy. The worst prognosis is for the roughly 10% of patients with idiopathic nephrotic syndrome who have focal sclerosis. |
|
|
treatment nephrotic syndrome
clipp |
Treatment
- IV furosemide, preceded by albumin infusion. Never treat with diuretic alone! Can lower intravascular volume to dangerously low levels. - Corticosteroids - No-added-salt diet. - When in remission, give polyvalent pneumococcal vaccine. For children who relapse frequently, treat with cyclophosphamide, chlorambucil, and/or cyclosporine for 8-12 wks, or longer. Most outgrow this disease by their late teens without permanent renal damage. |
|
|
Newborns with Jaundice
Danger signs |
Family history of significant hemolytic disease
Vomiting Lethargy Poor feeding Fever Onset of jaundice after the third day High-pitched cry Predischarge TSB or TcB level in the high-risk zone Jaundice observed in the first 24 h Blood group incompatibility with positive direct antiglobulin test Gestational age 35-36 wk Previous sibling received phototherapy Cephalohematoma or significant bruising Exclusive breastfeeding, particularly if nursing is not going well and weight loss is excessive East Asian race |
|
|
Kernicteris
early and late signs ? clipp |
Kernicterus
- basal ganglia and hippocampus - earliest signs lethargy, poor feeding, vomiting, and hypotonia - Late signs irritability, hypertonia, opisthotonus, seizures, extrapyramidal disturbances and deafness. |
|
|
How should poo's look in a newborn in first few days ?
How often should they pee ? clipp |
By the 3rd day of life, bowel movements should begin to appear yellow (no longer meconium) and by the 6th-7th day there are usually 3-4 stools per day (some have stools with every feeding). The baby should void 3 to 4 times a day by the third day, and by the 6th day of life the baby should urinate pale yellow urine at least 6 times a day.
Biliary atresia may appear in a healthy-appearing infant at 3 to 6 weeks with jaundice and gradually acholic (pale) stools. |
|
|
When use alt formula ?
clipp |
LActose in tol rare in year 1 : occ post gastroen, or hered galactosemia.
Human milk is high in palmitic and oleic acids. It contains the essential fatty acids, linoleic acid and alpha-linolenic acid, and their long-chain derivatives arachidonic acid and decosahexaenoic acid (these derivatives are not found in bovine milk). Infant formulas remove the fat of cow milk and add oils (the exact composition varies between formulas). Oils like palm olein, soy, coconut, sunflower, safflower are added. Linoleic and alpha-linolenic acids are added. |
|
|
newborn with
jaundice AND hepatospenomeg ? clipp |
* galactosemia may have hepatomegaly, ascites and edema. *
* sig hemolytic disease may have hepatosplenomegaly and pallor, with jaundice presents in the first 24 hours. * congenital infections (e.g., cytomegalovirus, toxoplasmosis, syphilis, rubella, herpes) may have elevated direct and indirect bilirubin, and may have hepatosplenomegaly. |
|
|
Physiologic Janudice
|
Unconjugated/Indirect Hyperbilirubinemia
* normally, in term newborn peaks at 3-4 days of life, * BY DEF bili 15 mg/dL or less in term, breastfed infants who are healthy. SO IF HIGHER, "BREAST FEEDING J or other ! * usually no rx, observe or photo, maybe. |
|
|
2 kinds breast-type jaundice
|
Unconjugated/Indirect Hyperbilirubinemia
Breastfeeding-associated Jaundice - breast-milk jaundice - may be caused by inhibitory substance in the milk that increases enterohepatic circulation. - breastfeeding jaundice / really lack of breast feeding ! - decreased milk supply leads to decreased enteral intake and increased enterohepatic circulation. |
|
|
PAthologic Jaundice
type diff dx |
Unconjugated/Indirect Hyperbilirubinemia
- antibody POSITIVE - direct Coombs or direct antibody test (DAT) positive. E.g. Rh/ABO incompatibilities, incompatibilities of minor blood group antigens. - antibody NEGATIVE - infants with red-cell membrane defects (e.g., spherocytosis) or red-cell enzyme defects (glucose-6-phosphate dehydrogenase or pyruvate kinase deficiency). - Increased bili production - bruising (birth trauma), cephalohematoma or other hemorrhages (intracranial), polycythemia or swallowed blood. - Decreased bili clearance - Crigler-Najjar syndrome, galactosemia or hypothyroidism. |
|
|
Unconjugated/Indirect Hyperbilirubinemia
Type - causes ? |
Unconjugated/Indirect Hyperbilirubinemia
1) Physiologic Jaundice - bili 15 mg/dL or less in term, breastfed infants who are healthy. Physiologic jaundice, which does not require treatment, usually peaks at 3-4 days of life. 2) Breastfeeding-associated Jaundice - breast-milk jaundice - may be caused by inhibitory substance in the milk that increases enterohepatic circulation. - breastfeeding jaundice - decreased milk supply leads to decreased enteral intake and increased enterohepatic circulation. 3) Pathologic Jaundice - antibody POSITIVE - direct Coombs or direct antibody test (DAT) positive. E.g. Rh/ABO incompatibilities, incompatibilities of minor blood group antigens. - antibody NEGATIVE - infants with red-cell membrane defects (e.g., spherocytosis) or red-cell enzyme defects (glucose-6-phosphate dehydrogenase or pyruvate kinase deficiency). - Increased bili production - bruising (birth trauma), cephalohematoma or other hemorrhages (intracranial), polycythemia or swallowed blood. - Decreased bili clearance - Crigler-Najjar syndrome, galactosemia or hypothyroidism. |
|
|
Conjugated/Direct Hyperbilirubinemia Causes -
|
Conjugated/Direct Hyperbilirubinemia Causes - Ischemic injury due to neonatal asphyxia, sepsis, congenital metabolic toxins or biliary obstruction such as biliary atresia.
|
|
|
biliary atresia
s/s? assoc with ? clipp |
Biliary atresia - intrahepatic or extrahepatic bile ducts abnormally small or absent. Associated with congenital heart dz, intestinal malrotation and other defects. If not corrected, can lead to progressive cirrhosis, portal HTN, hepatomegaly, jaundice and eventual death by age 2.
Signs and Sxs: jaundice, hepatomegaly, acholic stools, dark urine, elevated Direct Bili, elevated alk phos. |
|
|
Indications for Further Eval in Jaundiced Infants:
clipp |
Indications for Further Eval in Jaundiced Infants: Family h/o significant hemolytic dz; vomiting; lethargy; poor feeding; fever; onset of jaundice after 3rd day; high-pitched cry; dark urine; light stools.
|
|
|
when and why CBC in jaundice ?
clipp |
Eval of CBC in Jaundice - suspicion of hemolytic disease or anemia (e.g., jaundice in the first day of life or TSB >14 in the first 48 hours). If anemia found, an elevated reticulocyte count would be further evidence of hemolysis. These tests would be more essential if jaundice had presented in 1st 24 hours.
|
|
|
colostrum vs milk
ptn, and other stuff content ? how long doe sit come ? clipp |
Colostrum is yellowish fluid produced in 1st 5 days postpartum, and which is slowly replaced by milk. Contains more minerals and protein but less fat and carbs than milk, IgA.
|
|
|
benefits breastfeeding ?
clipp |
Benefits of Breastfeeding
1) Infants - maternal-child bonding, protection against some infections (e.g. otitis media, respiratory infections), SIDS and allergic reactions. 2) Maternal - decreased postpartum bleeding and more rapid uterine involution, lactational amenorrhea, earlier return to prepregnant weight, delayed resumption of ovulation with increased child spacing, improved bone remineralization postpartum, reduction in hip fractures in the postmenopausal period. Other benefits: decreased cost, readily available. |
|
|
newborn vit suppls
clipp |
Nutritional Supplementation
- During first 6 mos, infants should not be given extra water, juice, or vitamin/mineral supplements. All vitamins except Vitamin K are in human milk. - Fluoride - Breast- and bottle-fed infants both should receive fluoride supplements after 6 mos old if the water supply lacks fluoride (< 0.3 ppm). - Vitamin D - Breastfed infants may need Vitamin D before 6 mos if the baby not exposed to adequate sunlight (at least 15 minutes per week). -iron |
|
|
caput vs cephalohematoma ?
clipp |
Caput succedaneum: edematous swelling over the presenting portion of the scalp of an infant. It overlies the periosteum and therefore crosses suture lines, consists of serum, and would not cause hyperbilirubinemia.
Cephalohematoma: subperiosteal hemorrhage and thus will not extend across a suture line, and may contribute to hyperbilirubinemia. |
|
|
barlow and ortolani
clipp |
1) Barlow test - Examiner places thumb on the lesser trochanter and middle finger over greater trochanter. With the hips flexed to 90 degrees, the hip is brought into slight adduction and gentle downward pressure with the hand is applied to the hip. A normal hip will not dislocate, while a dislocatable hip will subtly move out of socket.
2) Ortolani Maneuver - Abduct the hip and push the femoral head anteriorly with your fingers over the greater trochanter. If dislocated, this maneuver will cause the femoral head to relocate with a "clunk." (With this maneuver, the baby makes an "O" -- Ortolani -- with its legs as its feet come together.) |
|
|
Bright futures
Prenatal AG |
fam resources
hiv breastfeeding SAFETY: car safety, pets (toxo), HOME - lead, mold, GUN, WATER under 120, smoke and CO detector, SLEEP safety, hand wash, limit baby exsposure to others. |
|
|
10 month old
bouts irritable draws up legs acts like in pain bloody stools and lethargic Diff Dx and eval ? peds curric |
Intussecption :
peak 5-12 mnths. inter bouts abd pain, bloody stool, +/- bil vomiting, and neuro shock like state. SIGNS : "Dances" no bowel in RLQ, xray Donot. U/S: "pseudokidney sign" edema walls compress dark mucosa A ABD xray reading that rules out intuss is "ileocolic area and RUQ" well visualized" RX: hydrate, NG decompress, hydrostatis reduction (air enema) then to OR. DIff Appy, Gastroenteritis, Meckels |
|
|
14 yr old
6 hrs abd pain right sided no diarr |
Appendicitis
- no diar usually - rectal pain/tender |
|
|
No poo for few days
"current yellow stools" guiac postive |
Juv polyposis coli
Peutz Jeugers |
|
|
Fever adn rash :
what labs to run |
CBC to check plts
UA consider strep swab or complment levels r/o tick bites |
|
|
14 months old baby with abd mass
how eval ? |
U/S
CT if not renal DIff: neuroblastoma #1 Renal: Wilms, ectopic kidney, |
|
|
incarcerated hernia
vs strangulated |
incarc : non reducible
stang : non-reduc AND blood supply arrested |
|
|
14 yr female
acute abd pain diff that is different from male 14 yr old |
PID
* Ovarian torsion |
|
|
Abd pain :
blood test results (CBC) |
Abd pain AND
----------------------- anemia = esp schisto HUS high plts = HSP |
|
|
Abd pain
UA results |
sterile pyuria = appendicitis
HUS = ptn uria and microhematuria |
|
|
Signs that abd pain DOES and DOES NOT need to go to OR
|
GO TO OR:
progression of pain, pinpoint tenderness, muscle ridgidity NO OR: resolution of pain, tolerate PO under observation |
|
|
What other then DM causes polyuria ?
|
DM
DI hyperthyroid intersititial nephritis high Ca renal failure and ptnuria CHECK: blood glu, urine |
|
|
13 year old and no periods.
When do you do a workup ? |
avg age 11.9 AA; 12 Cauc
Do PE for 2nd sex char, by 13 should have some. Generally have menses 2 years post breast buds. If no, consider Turners, check FSH. R/O imperg hyman but then you'd have pain. |
|
|
Key points to sports physical
|
special senses (eyes, hearing)
cardiac and pulm (PE fine) Neurologic Musculoskelel Tanner staging |
|
|
Kid with lots of bruusing - w/u
|
Check medical causes: CBC and plts
Note: patterned bruieses (loops) not c/w bleeding disorder. Skeletal survey in kids under 2 (non-verbal) "Silverman" 17 films CT head , abd, optho Note all sibs need eval. |
|
|
7 year old with vaginal discharge ?
Diff Dx |
* foreign body
* yeast infection abx * irritants like bubble bath * abuse |
|
|
accidental burn from intentional
|
splashes
donot mark immersion line |
|
|
Signs of skeletel injury that suggest abuse ?
|
Some parents should Manage Anger .
Spiral fx extremity Posterior rib fx S Metaphysiseal chip fracture (wrechning) esp if non-amb Ages - fx of diff ages |
|
|
Def of Failure to Thrive
|
FTT is physical neglect
under 2 SD below mean cross 2 percentiles |
|
|
What are these signs of ?
child under 6 vomit ipecac diarr laxatives recurent abscess polymicrobial apnea (choking) fever blood in urine/stool |
Munch by proxy
Trial separation Hidden camera Must be reported. |
|
|
16 mnth old
mad over no cookie cries, turns blue and pasess out |
Apnea spells
not volitional occur in expiation and reflexive paroxysmal 6 m - 6 yrs If freq investi possible Rett, seiz, sleep d/o, ortho hypo, fam dysauto also link pica. Behav Rx: put child on side. NO CPR but if brady can use atropine. |
|
|
bed wetting and day wetting ?
When clinical ? |
Bedwetting after age 6
day wetting after 4 For 2x week For 3 consec months Enuresis: Primary vs sec (new baby, acute stress) Enurseis occurs in 10-15% boys at 7 years old. RX: behav mod for 6 months Then DVAAP or TCA |
|
|
7 years old
loses temper argues with adults refuese to comply with adults req of rules delib annoy no resp mistakes angry resentful spiteful or vindictive impairs socially academic fx |
ODD
defiant, negativistic, disob, hostile behavior 4or more for 6 months RX: beh prob solve skills parent skills set limits constancy |
|
|
Dx ?
* soon after birth life threat bact infections * no grans |
Kostmann syndrome
As adol inc change leuk and myelodysplasia |
|
|
Dx ?
short steattorhea neutropenia |
Scwachman-Diamond syndrome
25% aplastic anemia 1% leuk |
|
|
eye partly white
photophobia rotary nystagmus |
chediak-higashi
AR abn neut granules |
|
|
megakarycyte hypoplasia
low plts no radii aplatic anemia ezcema |
Wiskott-ALdrich
|
|
|
- 4 yr old child previously well
-Presents with presistant nosebleeds 2 days -petechiae on arms and legs -plts under 10,000 |
** ITP low plts vs HUS nml plt count
** Ask about circum as ITP nml circ vs fx def bleed after circ. ** ITP often a couple days after viral URI ** can give pred in ITP but never without Bmarrow exam first ! ** acute ITP remission in 6 mnths vs chronic if last over that ITP RX #1 IvIg and #2 RhoGam |
|
|
2 days after diarrhea
2 year old pale, eyes yellow schistocytes on smear |
HUS
high BUN high retic indirect hyperbibli NORMAL PLT COUNT vs ITP low plts count (under 10k) |
|
|
Dx:
infant is floppy and weak but bright and alert (nml cognition) 4 months old absent deep tendon reflexes / areflexia tongue fasiculations nml pain sensation |
Infantile Spinal M Atrophy type I
aka Werdnig-Hoffman disease AR : Do blood genetic testing Loss of anterior horn cells Cognition remains normal ! T2 infants can sit but not walk T3 weakness starts later, post walking |
|
|
infant severe flooy at birth
obtundation difficulty suckling nad breating areflexia clubfeet weal facial muscles |
Myotonic dystrophy - neonatal
confirm with DNA analysis |
|
|
FEbrile seizures ?
Def and rules ? |
Under 15 minutes.
If it lasts over 30 mimutes = febrile status epllepticus LT f/u: no risks neuro deficits unless already have them. Does increase risk epilepsy later in kids with fam hx epi, complex febrile seizures, neurodev problems NO inc risk of more febrile seizures so no godo to prophy febrile seizures. |
|
|
For just one seizure, in a kid, do an EEG ?
|
No.
One seizure isn't treated with meds. EEG can't dz or r/o epilepsy. Can have one seiz (no fam hx) w/o meds. With 2nd seiz see neurologist, EEG. When MRI? focalality hints. Seiz and neurocutaneus disorder |
|
|
what kind of seix is tonic clonic ?
gen vs focal onset ? etc ? |
2nd generalized
focal onset |
|
|
seizure of 15 year old male in the morning.
What question do you ask in the history ? Etiology of d/o? |
Hand jerking ?
Juv myoclonus genetic starts around puberty photosensitivity common EEG: iireg genearlized poly spike and waf ve RX: AED resp good, no spont resolution. |
|
|
EEG pattern in infantile spasms
|
diffuse dysrhythmia
high voltage spike, slow waves, mult spike waves HYPSARRHYMMIA |
|
|
seizure with lip smacking but person is still alert
|
Rolandic
simple partial chldhoood often 2nd genearlized aura , tongue cheek, then genealoze to face as goes down gyri |
|
|
6 week old
staccato cough conjunctivitis |
chlamydia trach
gradual onset wbc normal Rx erythromycin |
|

|
bullous pemphigoid
|
|

|
current jelly stool
|
|

|
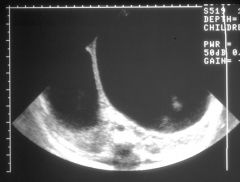
double bubble
|
|

kid has this rash
Also small size for age |
dermatitis herpetiformis
|
|

|
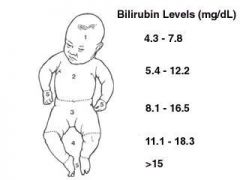
|
|
|
Anterior fontanelle'
Post -when close - what sutures What does AFOF mean ? |
- Ant font closes 18 months
nml 4-6 cm diamond at sagittal and coronal suture meeting nml AFOF = ant font open and flat - sagital and lambdoid suture meet closes at 2 months |
|

- midline capillary hemangiomas
- lumbosacral hypertrichosis - the lumbosacral dermal sinus - the midline lumbosacral subcutaneous lipoma - midline lumbosacral appendage (tail) |

cutaneous stigmata of occult spinal dysgraphism are present in 50-70% of patients w/ tethered cord.
* If your child was born with spina bifida (open spine) then the cord could become tethered because of the scar tissue that resulted from surgically closing the spine at birth. This scar tissue causes the cord to attach abnormally. * The spinal cord can also become tethered with spina bifida occulta. when your child bends or stretches but when it is tethered, it is stretched, especially with those movements. This abnormal stretching puts tension on the cord that can cause permanent damage to the muscles and nerves that control the legs, feet, bowel and bladder. Signs and symptoms Bowel or bladder problems: Orthopedic problems: Persistent back pain, (scoliosis), Loss of sensation in the legs or feet, Unequal growth legs or feet, gait probs, |
|
|
Teen
- you are doing HandP in ED after he is hit by car skateboarding - Past Hx : 3 months ago admitted and stomach pumped after intoxicated and OD extasy and prescription pills at a party - has "friends" doesn't say names - mostly hangs out - "bored" most of the time |
depressed ?
- sleep induction probs - change eating - "feeling boredom" - fam hx - SI or plan -social w/d isolation - feel hopeless - hx past depr, counseling, SA -recent inc EtOH, drugs, acting out, change school perf - recurrent 'accidents' - inc somatic symptoms-diminshed affect in interview -preocc with death HEADDS update article |
|
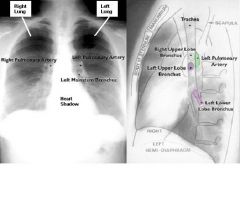
Which lobe if _______ obscured ?
R costophrenic angle ? Left ? R heart border ? Left ? |
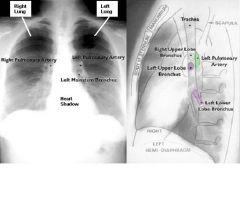
R costophrenic angle = R lower lobe
Left costophrenic angle = left lower lobe R heart border = right MIDDLE lobe L heart border = LEFT UPPER LOBE |
|
|
CXR tubes and lines
NGT ET tube chest tube central line Swan trans venous pacer |
* NG = should be in stomach and uncoiled, IF above diaph think hernia
* ET = 2 cm ABOVE carina * chest tube = in pleural space not in lung * Central venous catheter = in SVC not in RA (systemic pressures) * swan Ganz = Pulm Art (R heart pressures) * trans venous pacer = RA |
|
|
ECG rate mnenmonic
|
300
150 100 75 60 50 Irregular rates : count whole complexes in 30 lg boxes (6 seconds) and multiply by 10. |
|
|
ECG
sinus rhythm if : |
P waves in all leds
P wave upright in I and AVF No P usually means atrial rhy |
|
|
ECG
axis |
nml I + II+
LAD I + AVF neg RAD I neg, AVF + extreme RAD I and AVF neg |
|
|
ECG
intervals nml PR QT interval ? prolonged ? QRS interval ? prolonged when ? |
ECG intervals
* nml PR 120-200 msec short PR WPW Long PR heart block * QT interval : prolonged if over 440 msec * QRS interval nml under 120 msec prolonged QRS if beat ventricular, BBB, artificial pacing, TCA O/D, WPW |
|
|
ECG hypertrophy
|
NORMAL kids can have "abm" ECG
Has high sens low specific * RAE = P wave > 2.5 mm lead I,II, V1, V2 * LAE = broad (over 120ms) notched P I and II or biphasic in V1 * RVH = DOL 5 to 10 years upright T in V1 (T's flip from V3 to V1 as age); tall R in V1 or S in v6 * LVH = tall S V1 or R in V6; broad Q (over 40) in V5 V6; after 24hrsold inverted T's in V5 V6 never nml BVH = soft sign Katz-Wachtel criteria amplitude R+S one lead over 65mm OR R+S 2 leads over 45mm |
|
|
LP procedure
* Local ? * site ? * needle ? Tests: ? |
LP procedure
* Local anesth to skin subQ 1% lido * site L4-L5 OR L3-L4 * spinal needle 22ga 1 1/2 inch deep Tests: cell count, cx ans sens, glu, ptn conc Can do opening pressure |
|
|
Nml cells in Lumbar puncture
Nml protein ? |
WBC nml 0-5 but as high as 15 in neonate.
PMNs in this count abnormal but in neonate 1-2 PMNS can be normal. Protein = Up to 150 neonate, falls to nml 10-25 mg/dl by 6-12 weeks. Rises to adult range of 20-45 in puberty. In bloddy specimen CSF ptn rises 1 mg/dL per 1000 RBC/ml |
|
|
arterial puncture sites peds ?
|
radial
dorsalis pedia not axill, fem, brachial (throm or insif flimb) |
|
|
DX?
RX? kid high spiking fever spot rash abd, chest, extensor splenomegaly constipation hepatitis |
Typhoid fever
Salm typhi 1-3% intest perf and hemmorage !! other comps: myocard, PNA, hepatitis, menigoenceph RX: chloramphenicol PMS |
|
|
DX ?
WHAT COMP IS FEARED ? abdominal cramps, fever, vomit THEN diarr tenesmus and mucus BANDEMIA |
Shigellosis - bact dysentary
Shigella sonnei and flexneri Meningismus and seizures due to neuroTOXIN Treat by most amp pr TMP-SMZ concern of worse HUS PMS |
|
|
Who to treat Salmonella ?
|
Treat if :
under 6 months bactermia chronic illness or Icomp PMS |
|
|
3 month old infant
diarrhea for 3 weeks showing signs malnutr and slow growth |
Dx: intractible diarr of infancy
- infant under 6 mnths - D over 2 weeks w/ malnutr or malabs Etiol diverse: milk soy allergy : bloody diarrhea, vomit, poor feeding. RX: casein hydrolysate formula as soy ptn cross reacts with milk ptn , Hirsh, AI, transport defects, PMS |
|
|
chr diarr
Toddlers |
- Giardia Tx: stool Ag, duod biopsy/aspiration Rx: metro or quiniacrine
- inflam bowel d/o - primary malab d/o ...... CF .......celiac dz : PMS |
|
|
Kids falls and hits head.
When to do CT ? COMSEP |
You cre doing CT to look for brain bleed
Criteria : Fall 4-6 feet and onto what surface If no worsening in 4-6 hours, majority have no bleed and can go home. |
|
|
4 month old in Ed
fever 104 C petechiae Diff ? Tx? Manage ? |
SBI : sepsis and DIC
Blood cx Urine cx lumbar puncture : crypto, Gram CBC PT,PTT : if high consider DIC Admit and Tx : Vanc and ceftriaxone BUT overall #1 cause fever and petichaie VIRAL. |
|
|
Listeriosis
early onset vs late onset presentation |
* early onset neonatal
sepsis a fe whr after birth : resp distress, fever, diarrhrea, rash, hepato spleno megaly, (often mom had fever), miliary granulomatous dz * late onset, up to 5 weeks ( 9-30 days) meningitis = signs irritable, poor feeding, fever. MONOCYTOSIS 10-20% in CSF and peripheral blood Rx : amp and add gent if severe as synergistic |
|
|
early onset neonatal
sepsis a fe whr after birth : resp distress, fever, diarrhrea, rash, hepato spleno megaly, (often mom had fever), miliary granulomatous dz MONOCYTOSIS 10-20% in CSF and peripheral blood |
Listeriosis
early onset Rx amp and add gent for synergy |
|
|
Burns
When IV hydration ? |
* IV hydrate over 10% BSA ( child head 18% vs adult 9% as space came from legs); lg burns can add bicarb, don't add K at first as tissues release it.
*elec burns: myoglobinuria *bacitracin dressing now ok on face. Never sulf on face but now don't use silver sulfa. * intubate : inhalation injury by PF or other not just burnt nose hair OR over 25% burn BSA * * kids: higher risk infectin, worse fluid loss |
|
|
Kids CHF
dilated hypertrophic COMSEP |
* Dilated: infection, muscular dystrophy
*Hypertrophic : LVH, HOCM murmur CXR globular heart, * myocarditits incl Kawasakis : CHF, pulm edema, low QRS voltage, ST and T changes |
|
|
2 week old
fever 101F non focal exam LAbs? CXR? lumbar ? Empiric treatment ? COMSEP |
YES CBC and UA
Yes blood and urine cx Yes lumbar : ! can have meningitis without meningeal sepsis ! No CXR unless has cough. RX: HOSPITAL, AMP and GENT !! Use gent as bilirubin and Vanc. |
|
|
7 month old
fever 103 mild irritable poor feeding COMSEP |
R/O sepsis :
CBC, blood Cx, urine cx. No CXR unless has cough. Unlike a 2 week old, NO LUMBAR puncture. Empiric RX: no amp as not concerned about Listeria. |
|
|
Dx
6 month old high fever 3 days then pale pink maculopapular rash and fever gone Rx? |
Roseola infantum = 6th dz
pale pink rash on neck and trunk Rx supportive, Common cause of febrile seizures HHV 6 (occ sub occip LN or swollen eyelids) |
|
|
5th dz
vs 6th dz |
5th dz = slapped cheek parvo, erythema infectiousum
6th = roseola infantum , HHV6 |
|
|
7 year old
CCC macular rash face and neck goes down trunk DX? 2 names COMSEP |
Measles = rubeola
Rx: supportive AND IGG COmps: PNA, OM, enceph, SCPE, croup, hepatitis |
|
|
Dx :
4 yr old 5 days fever and rash not helped by tylenol and amoxi cranky and fever 103.6 bilat conjunct but non purulent puffy hands macularpapular rash COMSEP |
KAWASAKI
- Req 5 days fever (tylenol no good) - HIGH WBC (over 15K) , CRP high, ESR high - extremely puffy - red MM , red tongue, red conjunctiva, red pharynx RX: Now IVIG Later echo or cor A angio |
|
|
infant 20 days old, premie
lesions on scalp fever remains after 48 hrs on abx CNS signs mom fever at delivery CSP pleo cells, negative gram stain |
herpes
CCHMC |
|
|
fever
cchmc |
rectal 38C = 100.4F
|
|
|
FUS vs FUO
cchmc |
FUS fever source not apparent after HandP
|
|
|
SBI
cchmc |
meningitis
bone and joint inf soft tissue inf (cell) PNA UTI sepsis/bactremia enteritis |
|
|
Toxic appearence
= Yale Observ Scale |
lethargy
poor or no eye contact failure to ercogparents or interact with obejects and presons in room poor extremity perf acrocyanosis mottling slow cap refill < 2 secs in warm environ hypovent or hypervent or cyanosis |
|
|
Low risk of SBI = Rochester crit
|
prior h/o being healthy
-born term -no prior hx - no chr underly illness - not hx longer than mother - not tx for unexpl high bili - not recvd antimicrobial agents -no intrapartum materal fever, GBS nor abx treatment No focal bact inf on exam No evid purlent OM, skin , soft tissue, bone, joint. Neg lab screen. |
|
|
DX?
Lab tests ? 5 yr boy freq urination Na serum 150 likes to drink water over juice or milk slowing down in growth curve bit irritable/cranky, some muscle weakness playing soccar |
Diabetes Insipudus
can't conc urine PU, nml to high Serum Na (can get hyperNatr dehydration and show these symp late as intra cell dehydration. Irritable and muscle weak). Cause: tumor, trauma, histiocytosis LAB: morning urine SPGRAV < 1,010 Water deprive test: load first, deprive, sample plasma and urine. + test is wt loss 3-5%, dilute urine (osm under plasma), serum Na rises over 145 (nml body keeps Na WNL over water req), serum osmol over 290. Then test ddavp and if fail : central DI Workup Central DI: Skull radio, MRI Peds Recall |
|
|
Why can't you give
juice, soda, to dehydrated kid ? |
HYPO tonic !
serum 285 mOs Pedialyte 250 Infalyte 200 rehydralyte 310 |
|
|
floride suppl ?
mom is veggie, what suppls ? |
- FL only give after 6 Months
risk florinosis - mom veggie: thaimine, B12 |
|
|
14 month old
anorexia, itchy, failure to grow bulging anterior fontanelle tender swelling over tibias (both) Mom health food nuts |
Hyper vitaminosis A
Congen lack enz Pseudotumor : N, V chronic: slow wt gain, irritable, TENDER SWELLING OF BONES, hyperosteosis long bones, craniotabes, itching, skin fissures, desquam |
|
|
15 month old can't say recognizable words.
Normal ? COMSEP |
Speech:
* 6 months babble 9M mama/dada byebye * 12M 1-3 words, 1 step commends * 2 years 2-3 word phrases * 3 years 3/4 of speech understandable to strangers, 3 colors 4 years tells a story FA |
|
|
babble VS understand 3/4's of speech
|
* 6 months babble and at 3 strangers understand 3/4 of speech
FA |
|
|
Age kids have 2-3 word phrase ?
|
* 2 years 2-3 word phrases
FA |
|
|
social smile
|
2 months
|
|
|
head up prone
|
2 Months
head up prone eyes follow object to midline, eye contact recognize parent |
|
|
Rolls over ?
|
4 months
rolls over laughs regards hand |
|
|
regards hand ?
|
4 months regards hand
6 months transfers objects hand to hand 9 -10 M pincer grasp |
|
|
transfers objects hand to hand
|
6 months transfers objects hand to hand
4 months regards hand 9 -10 M pincer grasp |
|
|
crawls
|
9M crawl, cruises
12M walks 2 Y stairs, kicks 3 tricycle 4 yr hop on one foot ------------ 4 M roll over 6 M sit well unsupported , roll prone to supine |
|
|
cruises
|
4 M roll over
6 M sit well unsupported , roll prone to supine 9M crawl, cruises 12M walks 2 Y stairs, kicks 3 tricycle 4 yr hop on one foot |
|
|
walks
|
12M walks
2 Y stairs, kicks 3 tricycle 4 yr hop on one foot ------------ 4 M roll over 6 M sit well unsupported , roll prone to supine 9M crawl, cruises |
|
|
kicks ball
|
2 Y stairs, kicks
3 tricycle 4 yr hop on one foot ------------ 4 M roll over 6 M sit well unsupported , roll prone to supine 9M crawl, cruises 12M walks |
|
|
hop on one foot
|
4 yr hop on one foot
------------ 4 M roll over 6 M sit well unsupported , roll prone to supine 9M crawl, cruises 12M walks 2 Y stairs, kicks 3 tricycle |
|
|
Ages ?
paralell play group play |
2 years parallel play
3 yrs group play, simple games 4 yrs plays with kids, simple interaction |
|
|
Mnemonic for behaviors at 6 months
|
6abbles = 6 months babbles
Six strangers switch sitting at six months - sit well -recog strangers - switch obj hand to hand babble, rolls prone to supine |
|
|
Words mneumonic
|
- know 1 word at 1 year
- Puts 2 words together at 2 years And half of speech understandable by strangers |
|
|
Mneumonic 3 years
|
TRIcycle
stacks 3 cubes, 3 numbers, 3 colors, 3 kids in a group (plays in group), 3/4 speech understandable |
|
|
shape drawing
|
A 2 year old can copy a line,
So a 4 year old can copy 2 lines to make a cross and a square ( 4 sides) |
|
|
dyslexia
|
written lang
kids have excellent verbal lang |
|
|
4 year mneumonic
|
4 year old
40 lbs 40 inches tall draw 4 sides figure (copy square) |
|
|
Sleep
-infants |
- infant half time is REM
- parasomnias peak age 3 -nightmare in REM - night terror non-REM, amnesic -sleep walking ages 4-8, nonREM |
|
|
Short stature
|
- short stature = height < 5th percentile (or 2nd)
Causes: - #1 : familial /normal varient : nml growth rate, nml bone age, puberty at nml age - constitutional delay : "late bloomers", will have growth spurt later, also nml varient, decel growth 6M to 1 yr and resume 2-3yrs, delay puberty and delayed bone age -> Bone age = height Age NML : Chrono age = Bone age / height age Other causes delayed bone age: GH def, hypothyroid, pit hypo, ALso cz short : nutri, Cushing, Silver Russel |
|
|
Tall
|
- #1 familial
- Hormonal : adrogens / CAH, sex steroids, GH - syndromes : Marfan Kleinfelter SOTOS syndrome: assoc MR and cerebral gigantism |
|
|
Amt of steroids that means no live vax
|
high dose steroids
2 mg/kg/day OR 20 mg day oral for 14 days or more Can still vax if EOD, inhaled, physiologic dosing. |
|
|
Characteristics of innocent heart murmur
|
nml S1 and S2
periph pulses nml no structal heart defects nml CXR, ECG asymptomatic Grade III or less usually systolic or flow Usually LUSB BAD: clicks, snaps, extra sounds, heaves, thrills, low femoral pulses OR no change with body position (venous gone gone if supine and Still gone if Valsalva) Do not count murmurs with fevers. |
|
|
What is schedule for WCC newborn ?
|
1 week
2 week 1 month 2 month 4 month |
|
|
MAIN DX IDEA ?
10 yr old boy dark urine headache COMSEP |
glomerulonephritis
Main cause in kids post-strep Confirm glomneph looking for cell in urine (the h/a is HTN) |
|
|
2 year old
fever urine 1+ ketone, 1+ protein murmur |
kids w/ fever
can have ptnuria and with tachy can have murmur re-eval once afebrile |
|
|
Hematuria in kids Mneumonic
AND workup |
TICS
TRAUMA tumor Infection #1 UTI, POST STREP, inflamm (GOMERULOnephritis) S stones (calciuria) , sickle hgb get hemturia with infarcts and damage ALSO: conge anomoly (ruptured cyst), and healthy kid exercising microhematuria, HUS W/U: CBC for HUS, renal and UA |
|
|
Proteinuria causes
COMSEP |
nephrotic
orthostatic transient glomerneph |
|
|
Labs to do if hematuria and ptnuria
|
creat, C3, ASO, maybe ANA titer
LOW C3: post strep, SLE, chr infection |
|
|
Hearing testing
|
- Birth ABER
- Age 4 tones with hand raising COnductive loss causing hearing delay an ind for PE tubes RF hearing loss: Under 35 weeks getation, in NICU, hyperbili needing exch tx, ototoxic abx, TORCH, pulm HTN, neuro inj, Small birthwt under 1000 g has 10% hearing impairment |
|
|
Strabismus
amblyopia |
esotropia : rolling in
exotrpia : rolling out Correct early or develop AMBLYOPIA = poor vision in one eye when a deviated eye. |
|
|
Hearing testing
|
- Birth ABER
- Age 4 tones with hand raising COnductive loss causing hearing delay an ind for PE tubes RF hearing loss: Under 35 weeks getation, in NICU, hyperbili needing exch tx, ototoxic abx, TORCH, pulm HTN, neuro inj, Small birthwt under 1000 g has 10% hearing impairment |
|
|
Strabismus
amblyopia |
esotropia : rolling in
exotrpia : rolling out Correct early or develop AMBLYOPIA = poor vision in one eye when a deviated eye. |
|
|
Sports physical
- when need to do ECG ? - when complaint of LH, do you need to do ECG ? |
ECG for longQT, WPW, hypertrophic cardiomyopathy.
NO need for it if LH due to pre-syncope 2/2 hypotension. |
|
|
Sports physical
nutritional suppl What is SE creatine ? |
Creatine
SE weight gain from edema cramps, heat intolerance sprains High BUN, creatinine, CPK NOt endoresed for use in Peds Not recc anyone with renal dz |
|
|
Sports physical
contraindications for contact sports |
one kidney
Downs: do c spine xray first |
|
|
13 year old
Chest pain sudden sporadic pain, L sternal border well localized worse inspiraton NOT related to exercise #1 cause |
- precordial catch syndrome
etiol unk. #1 cause chest pain in adol not reltd to exercise |
|
|
VAx for adol
|
11-12 MCV4
Tdap Hep B 2nd dose varicella if not already |
|

limp w/ insidious onset after mild bump on coffee table
Boy 7 cana move hip/leg without pain but knee hurts can't bring leg out or rotate in |

Legg perthes
aseptic necrosis femoral head limited abduction and int rotation Diag: MRI can show avas necrosis before xray can Rx: observe and brace ig dec ROM |
|

Male 12
overweight pain in leg and knee won't put weight on leg leg tends to roll into ext rotation |
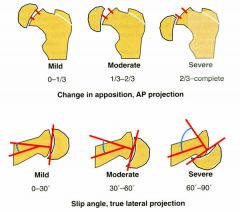
SCFE : males 11-13
SCFE RF: adol, obese, endo (Cushing, DM) HYPOTHYROID W/U : xray both hips, AP and frog leg view. kidney failure, or growth hormon Rx: ortho consult, iny fix with percut pin |
|

|
cavus
high arch neuromus dz |
|

|
club foot = talipes equinovarus
* 4 Features : Has hindfoot also varus equinus heel metatarsus adductus talonavicular subluxation * Unlike positional clubfoot form being in uterus which you can unfold in exam. * Common 1/1000 * Do radio and prepare sx |
|

treats what ?
|
DDH
|
|
|
Knee cap PE
What part of knee hurts in MCL injury ? Osgood schlater ? |

|
|
|
Dx and test
18 month old afebrile won't put weight on right hip swollen warm R knee 3 weeks ago kid had viral URI |
Transient synovitis
* Like septic joint, need to tap joint to tell apart. * usually afebrile ( but can have septic joint w/o fever ) * often preceded by URI Rx: tap joint to r/o septic joint, supportive , NSAIDs. |
|
|
ankle sprain
Most common : inversion injures ? eversion injures / |
Inversion is 85%
- lat ligament 1st ant talofibular, then if severe pain its also post talofibular Eversion 15% medial lig most common deltoid lig More severe vs inversion injr=ury Grade 2 is brusing, some loss of ROM Grade III: joint unstable, total loss of ROM |
|
|
osteosarcoma
ages ? all need what test for mets ? Rx ? |
10-20, 'sunburst pattern"
all need CT for mets in lungs Rx rad and chemo |
|
|
Ewing sarcoma
|
ages 1-10
'onion skin " on xray, radiolucent w. calcified periosteal elevation rare CAuc and hereditary Need CT for mets Rx: rad, chemo, sx, some BMT auto |
|
|
* Baby 4 months old
when flex hips left knee lower * 12 months old painless limp and lurch to left |
Left develop dysplais hip
- 3 to 6M that side knee lower Then muscle contractures and nml Ortolani and Barlow BUT - 12 months trendel to that side IF bilateral dislocation waddle gait and lordosis as both displaced hips. Newborn w/DDH have nml xray untl 6-8 weeks. |
|
|
OI types
|
mild OI : type I and IV
lethal in newborn type II III severe OI bone deform and lots of fx |
|
|
torticollis
low hairline deaf |
Klippel Feil syndrome
Con gen fusion of sevearl cervical vertbra - short neck -low hairline - limited neck motion ALso renal anb, scoloios, s bifida, deafness TESTS: renal u/s, hearing, c spine flex ext films. |
|
|
child under 11
vague knee pain feel loose body in knee |

osteochritis dissecans
avas necrosis of bone next to artic cartilege kids: observe adol: can remove bit |
|

neonate
bloated abd shock |
NEC
gas in bowel wall giving lining, double wall like railroad track without ties |
|

|
thrush
|
|
|
10 month old
oral thrush many axillary and inguinal LN recurrent PNA FTT |
Immunodef suspect in oral thrush at 10 months
Not SCID which has absent thymus and hypoplastic LN Not Brutons as that has no peripheral LN |
|
|
Letterer Siwe dz
|
langerhans histiocytosis form
Immunodef skeleton involved seborrea derm LNadenopathy hepatosplenomag bluging eyes pit dysfx systemic : fever, FTT, growth retardation |
|
|
red vascular birthmark on nose
wobbly gait develops chronic sinus infections and PNA What is risk ? |
ataxia telangiestasia
AR nad repair Presents years 1-6 Risk leuk/lymphomas LAb: high AFP and CEA |
|
|
Brutons agamma
VS Common variable immunodef |
Brutons : younger , no B cells, gene Xq22 Ty kinase. No tonsils adenoids and peripheral LN !
CVID: older, less severe infections, makes autoab, celiac dz like symptoms, bald, thymoma, perm anemia |
|
|
staph PNA
mild bleeding issues eye has white patch pancytopenia |
Chediak higashi
progerssive peripheral neuropathy RX : high dose ascorbic ACID ABX, BMT |
|
|
Lots of skin infections
pneumonitis osteo big liver and spleen |
CGD
do NZT test Will have high ESR, high gama globulinemia Abn CXR |
|
|
Effects of no spleen
|
Low IgM, alt complement
Need opsonic ab See howell jowell bodies |
|
|
staph infections recur
eczema like rash, itches |
Jobs
also "course" facial features IgE over 10,000 IU/ml eosinophilia Rx antistaph pen, IVIG ! |
|
|
6 yr old
prev healthy girl LN anterior cervical 3 x 5 cm tender |
anything under 2 cm normal
SO this is BIG unilateral NOT after a DX SO biopsy as might be CANCER. |
|
|
growth
What is stunting ? |
flattening of growth curve
|
|
|
"At risk for overweight" means what ?
|
BMI > 85 th percentile
or under 95th |
|
|
Kid eats pre natel vits ?
Signs toxicity ? At what levels ? Treatment ? |
N/V/D
blue lips, nails, hypotension Over 60 mg/kg toxic/death RX: defuroxime |
|
|
6 yr old
fever h/a , sore throat rash mac-pap worst axilla and groin |
Strep pyogenes
sandpaper rash scarlet fever Rx penicillin |
|
|
cord falls off when ?
|
10-14 days
|
|
|
EM of kidney
"spike and dome" |
Spike and dome in EM
Membranous glomerulunephritis #1 cause nephrotic in adults but rare in children Kids ususaly resolve form it on own. |
|
|
Postural proteinuria
Worse when laying or sitting ? |
more ptnuria when laying supine.
|
|
|
Child with :
- acute renal failure and recently on sulfa abx - chronic renail failure : N, V, headache, fatigue, HTN, growth failure. H/o reflux and infections |
Intersitital nephritis
acute neph ARF : drugs NSAIDS, sulfa, penny, ampho chronic: anesgel, lithium, infection, vesiorefluz ACute biopsy: lymohs, eos, neuts and edema in kidney but glom nml chronic: lymphs and plasma cells. fibrosis nad sclerosed glomeruli due to ischemia. These kids usually progress to ESRD. |
|
|
Cystineuria
Stones RAdio ? Treatment ? How treat uric acid stones ? Struvite ? Ca ? |
Cystinuria
Stones : radioopaque. Rx with D-penicillamine to chelate cystine. D/D : AR, low reabsorb di-basic aa (cyst, lysine, arg, orn) Uric Acid - allopurinol and alkalinaize urine. STruvite - abx Ca thiazide diuretics to reduce ca excretion or pot citrate to inhibit ca stones. Stones over 5-6 mm need to use stent or lithotripsy to remove. |
|
|
Pyelo vs cystitis
|
Cystitis : usually no fever
Pyelo :fever, abd flank pain, N/V/D UA abn of over 5 WBCs Over 100,000 colonies one bact or 10,000 in symptomatic child or any growth in cath sample. |
|
|
Treatment of peds UTIs
|
Treat those 2 months to 2 years LONGER : more likley bactremia so : 10-14 days
Kids over 2 : 5-7 days All under 5 yrs and all males : renal U/S. |
|
|
to de-torse testicle
|
open book.
Most torse medial so rotate testicle out like opening a book. |
|
|
How do you tell RTA apart !
In kid how might it present ? Which has renal stones? Which has rickets ? Which is Fanconi anemia ? |
Type 1 : DISTAL : can be for life. Has acidosis as defect in secreting Hyd ions. Has renal stones (hyperCaUria).
Type 2 : Proximal : Low resorb of BiCarb. Usually resolves. Part of other things: Fanconi. Can have rickets due to phosphate wasting. Type 3: combo of 1 and 2. Type 4: Mineralocorticoid def like low aldosterone (Addisons, CAH) or low renin (renal interstitial dz). |
|
|
2 year old boy
left flank mass incidnetly found by mom BP 110/70 UA 5-10 RBCs 2-3 leuko |
Wilms
mut p53 Do U/S abd and urinary tract Then CT |
|
|
8 year old girl
easily palpable kidneys U/S shows cysts in kidneys hepatic fibrosis portal HTN |
Auto RECESSIVE
polycystic kidney Dz - renal cysts are dilations of colleting ducts - as fetus oligohydram and Potter -results in ESRD |
|
|
1 week old
wrinkled belly which lacks abd muscle High BUN distended bladder |
Prune belly syndrome
- wrinkled belly as underdev ant m wall - can see club feet - urinary tract abn - GU abn (undesc testes lots pyelo and renal abn |
|
|
Dx:
18 year old develops anorexia, polyuria and polydipsia and unexplained fevers Lab shows glucosuria but nml blood glucose. Abnormallyhigh urine PH in presence of hyperchloremic metabolic acidosis and mild hypoalbuminemia. |
Fanconi syndrome
proximal RTA : loss phos and rickets younger kids : growth retardation, rickets RX: phosphate, bicarb therapy CAuses: - cystinosis -galactosemia, tyrosinemia, wilsons chemo drugs, metals, gentamycin, old tetracycline |
|

7 month old with this mouth ?
Why ? |
baby bottle decay aka early childhood caries
- use cup at one - no juice from bottle, use cup - no nightime bottle / breast - no flouride toothpaste until 2 or 3 unless dentist says so |
|
|
When kid get upper GI endoscope ?
|
S/S GI ulcer : night pain better with food, dark stool, did vomit frank blood once.
Maybe not if vomiting 2 days due to hamburger and "streaks" of blood in emesis. SMALL Malory-Weiss tears from emesis are common and rarely lead to bad life threat bleeds. SO, if person stable and not bleeding, don't need to do a scope NOW in the ED. Watch and observe. |
|
|
17 month old
- cranky for 1 month - won't walk -seems tender over both her legs -low grade fever -petichae over skin and small not well healed cut XRAY of legs : "genearlized bony atrophy with epiphyeal separation" |
SCURVY
- kids get diffuse tenderness over bones worst on legs - poor wound healing / collagen formation -hemmorage signs - low grade fever swelling, tachypnea, poor appetite DX: clin picture, hx. No lab test. PreTest Peds |
|
|
Wrong choice on FIRST AID:
Behcet |
Behcet :
vascultis sm and med arteries -non-destructive artritis, esp lg joints like knees - Systemic symptoms : fever, erythema nodosum, apthus stomatitis, uvetitis, CNS thigns |
|
|
Wrong choice on FIRST AID:
- infant hepatosplenomegaly D, V FTT icterus, malabrob CALCIFIED ADRENAL GLAND on KUB No treatment |
Wolman syndrome
lysosomal acid lipase disorder - infant hepatosplenomegaly D, V FTT icterus, malabrob CALCIFIED ADRENAL GLAND on KUB No treatment |
|
|
HYdronephrosis
causes ? |
PURE P
Posterior urethral valve Uretopelvic obst reflux Ectopic ureterocele Prune bely syndrome - cause unilateral hydronephrosis : #1 UPJ obst - to show kidney fx in obst kidney do furosemide renogram - congenital UPJ obst : only hydroNEPh not in ureter - #1 cause uretal tract obst in boys: post uretal valve s: ureatra and ureters and kidneys all big (Rx by sx obliterate the valves) |
|
|
VesiculoUretel reflux
|
Grade 1 and 2 = lower ureter and renal pelvis
RX: watch, prophy low dose abx, UA cx every 3-4 months Grades 4-5 : see hydronephrosi Do Sx. |
|
|
3 features of prune belly syndrome
|
abs muscle under developed
undesc both testes (in abdomen) urine tract abn |
|
|
Wilm vs neuroblastoma
|
........Wilms / Neuroblastoma
AB..bulging flank // calcified CXR lung mets // paravertebral mass Bone rad ..none // bony mets CT....renal // supra renal calcified Nuc bone scan x // tumor uptake U/S solid or cystic // solid, calci suprarenal poss invade renal vein // encasement of vessels |
|
|
torus fx aka buckle fx =
greenstick fx = breaks Salter Harris breaks = Bowing : elastic deformaton = |
torus fx aka buckle fx = bucklig of one side of bone's cortex
greenstick fx = incomplete fx (transverse), on one side cortex breaks and on other side periosteum breaks Salter Harris breaks = to epiphseal plate Bowing : bone deforms and may not remodel back to right place elastic deformaton = bone goes back to originol position |
|
|
Of finger abn -
fused extra one big etc Which is worst ? |
macrodactyl , one big finger, retd AVMs, NF, lymphangiomatosis.
Also extra finger common in AA but in Cauc can be sign of other congen abn |
|
|
How can you use imaging and such for DDH
|
- radiographs not good as infants not ossifed younger then 6-12 months.
But best film AP NOT frog-leg. - ultrasound up to 5 months before fem head ossifies - clin exam (frog leg is for SCFE) |
|
|
adol chronic foot pain
on radio has "calcaneonavicular bridge" where 2 bones fused OR talocalcaneal joint obliteration. |
Tarsal coalition
cause of chrinic foot pain A congenital fusion of tarsal bones. Best eval is with CT. |
|
|
scolisos eval
signs not idio ? |
Idio : s curve convex to right thoracic area
NOt idio sign: upper thoracic location focal cuvrve and no reverse curve sharp angulation Other causes: neuromuscular, neurofibram, syrinx |
|
|
3 langeehana histiocytoses dza
|
* eos granuloma : spine w. collapse of vertrabra, lytic skull lesion
* Letterer-Siwe acute diffuse fatal, rash hepatospelenomag lung * Hand schuller Christian chronic diffuse skull defect DI bulging eye |
|
|
Newborn with chylothorax
Epi ? Rx? |
Nml FT infants, nml delivery
- presents at end of week one, only milky fluid after eat milk - CXR massive pleural effusion #1 cause chylothorax - Rx : feed with MCT and thoracocentesis Rad recall |
|
|
Newborn with pulm edema on CXR
and normal heart size - don't recover in 24-72 hrs - recover in 24-72 hrs |

don't recover 24-72 hrs
hypoplastic left heart IMAGE (heart can also be big) TAPVR with obst pulm lymphangiectasia DO recover in 24-72 hrs TTN Aspiration of amn fluid intra cranial hemm hyperviscosity hypervolemia |
|
|
Newborn with pulm edema on CXR
and BIG heart size - don't recover in 24-72 hrs |
Do not recover in 24-72 hrs
hypoplastic left heart severe co-arc myocardiopathy |
|
|
newborn
patcy lung infiltrates -small lung vol -lg lung vol |
small lung vol
RDS pulm hypoplasia hypoventilation Lg lung vol I HEAR Infection (PNA) Hemmor EDema incl TTN and rarely neprotic Aspiration esp of mec RDS of on vent |
|
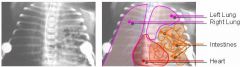
Name 2 kinds of diaph hernias ?
Which is common one ? |

Pic before is of Bochdalek herina, Most congen Diaoh hernia.
The Bochdalek foramen/hernia's most LEFT, posterior and have upper pole of kidney, retroper fat, and some bowel. More rare Morgagni hernia out Morgani foramen which is right behind stermnum. Often have bowel or fat. |
|
|
steeple sign
vs thumg sign |
steeple :
narrow trachea looks pointed in sub-glottic airway on FRONTAL film in CROUP Thumb print sign lg epiglottis looks like thumb on LATERAL film in epiglittis |
|
|
steeple sign
|
steeple :
narrow trachea looks pointed in sub-glottic airway on FRONTAL film in CROUP Thumb print sign lg epiglottis looks like thumb on LATERAL film in epiglittis |
|
|
thumb sign
|
Thumb print sign
lg epiglottis looks like thumb on LATERAL film in epiglittis [steeple : narrow trachea looks pointed in sub-glottic airway on FRONTAL film in CROUP] |
|
|
situs types
s. ....(nml) s. inv s ambig |
s solitus = nml
s inversus = mirrow image aortic arch, heart, liver on right side s ambig = bilat right sidedness, epartial brinchi, trilobar lungs, asplenia, horixontal liver, midine stomach |
|
|
ASD
o primum o secundm |
ASD
most common o secudum which iss high up w. o primum which is lower in atriam : can see endo card cusion defect, cleft mitral valve, ant mitral valve in septum. |
|
|
two most common causes cyanotic heart dz infants
|
TOF: decreased flow thru pulm vessels, boot heart, often right sided aortic arch
transposition great arteies : varible flow thru pulm vessels, lg heart and narrow mediastinum, egg-on-a-side pattern. |
|
|
why do you bring down an undesc teste ?
|
- easier to examine for cancer, but risk same
- DOES DECREASED risk of torsion - doesn't help sperm count |
|

|
NEPHROTIC SYNDROME MIXED
CAST Oval fat bodies(3), Red blood cells casts(5), Waxy casts(1), Cellular casts(1), Renal tubular cells(1), Hematuria with dysmorphocytosis |
|

|
RBC casts
glomerulunephritis nephritis syndrome in lkids , post strep esp if HTN. (IgA has no HTN usually) |
|

|
Renal tubule epithelial cell casts
as ischemia, infarction, or nephrotoxicity cause degeneration and necrosis of tubular epithelial cells. The presence of these casts indicates acute tubular injury |
|

|
WBc cast
|
|
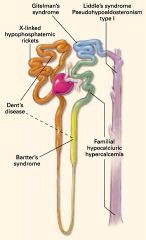
CASE:
4 year old girl , ht and wt 5th percentile serum K 2.7 meq/l normal BP DX ? Hint : polyuria, polydipsia, and a tendency to dehydration, can vomiting |
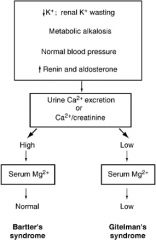
- inherited hypokalaemic alkaloses often also hypomagnesaemia,
chloride wasting and hyper-/hypocalciuria - HIGH aldo but unlike pri hyperaldo as renin high not supressed and have nml BP, not HTN. - Barttner, Liddle, Gitelman, apparent mineralocorticoid excess, glucocorticoid suppressible hyperaldosteronism. - Bartner's : Like people on furosemide, pee alot, loss of Na and Cl, dehyd, can lose Ca - neonatal BArtnerr : presents prem birth as polyhyd, have severe dz w. ca stones renal failure. - Classic Barter presents in school age. Normal or slight urinary ca excr no kidney stones. Bartnerr VS Gitelman Both abn NaCl absorbtion. Gitelman: distal tubule VS Bartner : thick asc limb * Gitelman has LOW SERUM MG and not Ca in urine * Bartnerr : nml serum Mg , more Ca in urine |
|
|
benadryl OD
|
lethargy
tachycrdia excitation |
|
|
What age range drowns and gets burns ?
|
Kids under 4 drown
Kids under 4 : scald, elec burn, contact burns. |
|
|
Burn classification
4 critieria and only one is depth |
Depth : super (1), partial thick, full thick
PErcent BSA Location - disability, worse if face, etc Assoc with other injuries |
|
|
Infant compressions
PALS |
under 1 year old
- one hand on head - 2 middle fingers sternum one finger bredth below nipple line - press down 0.5 - 1 inch - 100 per minute - ratio 30:3 Two rescuers Hands circle chest thumbs on sternum 15:2 ratio |
|
|
child compressions
- age - how PALS |
Age 1 to puberty
child compressions One resucer - one hand on head - heel of hand lower half of sterum - press 1 - 1 1/2 inches down, 100/min - ratio 30:2 if one rescuer If 2 recuers ratio 15: 2 |
|
|
PALS
rescue breaths what ages mouth and nose ? vs mouth ? |
infants under 1 year : cover mouth and nose
infants obligate nose breathers ! Remember when suctioning to suction their nose. child over 1 year : cover mouth and pinch nose |
|
|
PALS
How is start diff from adults ? |
Arrive
- check for responsivness - shout for help, - give 1 minute BLS ----if pulse give one cycle of 20 breaths before calling 911 ---- if no pulse or HR under 60, chest compressions and do cycle for one minute, then call 911. - Then call for help by phone |
|
|
IV sites
PALS |
Arm
med cubital cephalic vein and trib in hand basilic Lower leg saphenuous esp gr saph ankle veins dorsal arch med marginal |
|
|
pinpoint pupils
|
coma
narcs pilocarpine pesticides and nerve gas (organophosphates ) Horner pontine hemmorage posterior synechia ? 3 sphilis ( maybe 3rd N paraysis or closed angle glaucoma) (atropine gives fat pupils) |
|
|
fat pupils
|
epi
phenylepi atropine-like drugs |
|
|
atropine
pilocarpine pupils |
BLock Mus-Ach R
--------- Atropine is from belladona nightshade Atropine is antagonist of musc - Ach R Mus Agonist ------------------- physostigmine or pilocarpine. |
|
|
4 year old in garage
drooling teary wet his pants and vomited sweated |
Atropine is given as an antidote to SLUDGE (Salivation, Lacrimation, Urination, Diaphoresis, Gastrointestinal motility, Emesis) symptoms caused by organophosphate poisoning.
|
|
|
Types of hemiparalysis
|
* Todds (post-ictal ) paralysis = contralateral
|
|
|
herniations that preesnt with
* CN III dysfx * cheyne stokes |
* uncal hernia Ipsi lat oculomotor probs
* transtentorial hern cheyne stokes |
|
|
How treat tetanus ?
|
human tet Ig
IV pen or metro sx debridge wound dark room, intub, sedate, diazepam of severe |
|
|
MELAS
MERRF |
Both mitoch encephalopathy and mutant tRNAs
MELAS: mito enceph, Lactic acidosis, strokelike episodes, hemianopsia and cortical blindness , Dx m bops MERFF myocloin epi raggd red fibers get epilepsy , cerbellar ataxia , dysarthria NOT SAME as freidrich's ataxia : onset before age 10 , ataxia worse in legs than arms, profound hypotonia , postive Romburg , low to no DTRs , skel abn , cardiomyopathy , optic atrophy , HIGH AFP , peripheral nerve deficits , only boys AR for mitoch ptn frataxin |
|
|
freidrichs ataxia
|
MERFF myocloin epi raggd red fibers get epilepsy , cerbellar ataxia , dysarthria
NOT SAME as freidrich's ataxia : onset before age 10 , ataxia worse in legs than arms, profound hypotonia , postive Romburg , low to no DTRs , skel abn , cardiomyopathy , optic atrophy , HIGH AFP , peripheral nerve deficits , only boys AR for mitoch ptn frataxin |
|
|
age 2 oculomotor ataxia
about age 4 worse and losing ability to walk as teen get red marks of capilay on nose , eyes, limbs |
ataxia teleangiectasia
risk brain tumor and lympoid tumors |
|
|
2 year old
Viral illness 2 weeks later sudden onset truncal ataxia and kid can't sit or stand anymore horizontal nystagmus |
ACUTE CEREBELLAR ATAXIA
Dx of exclusion r/o freidrichs compelte recovery in 2 mnths |
|
|
infant botulism
|
1 sign is abscence defecation
to have botulism must have CN palsies and typically bilateral symmetric palsies No good to use abx or blocking antibodies. Can use EMG with high freq reverses pre-syn blockade and incremental response. |
|
|
5 month old
- doesn't seem to look at parents any more - "startles" more - WBCs have no hexosaminase A |
tay sachs
|
|
|
hartnups
|
hartnups : urine pro OH-pro and arg normal
Plasma levels nml. Rx NAD/NADH and high ptn diet. this has rashses psych changes |
|
|
neonatal jaundice
hepatosplenomegaly Neuro degen signs |
Nieman pick
has hepspel meg unlike Tay Sachs No sphingomyelinase |
|
|
4 year old
fractures his femur pancytopenia splenomegaly |
GAuchers
AR Rx with enz replacement : Beata glucosidase In dz glucocerebroside accumlates in retic endo system : bone, spleen, liver. |
|
|
red macules that don't blanch
severe limb pain renal failure and bx shows lipid |
FAbry
XL |
|

scimatar
|

TAPVR with return below ? diaph
so wierd artery loops down across chest presents with child older, even a teen |
|
|
kid tet spells CXR
|

TOF boot cxr
|
|

ASD CXR
|
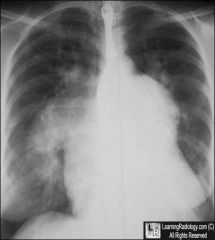
above worse ASD with PAHTN
|
|
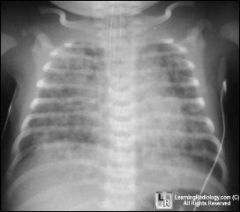
birth trouble
mec stained fluid |
mec aspiration
|
|

|
double aortic arch esophagus
|

