![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
18 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Increase pulmonary blood flow (Acynotic) Because blood is oxygenated it's usually asymptomatic unless severe. |
Atrial septal defect (ASD)
Ventrial septal defect (VSD)
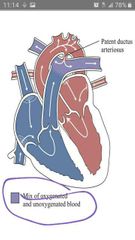
Patent ductus arteriosus (PDA)
|
|
|
|
Obstructive heart- ventricles can't pump blood due to resistance. It's also ACYNOTIC |
Aortic stenosis
Coarctation of the aorta |
|
|
|
Decrease pulmonary blood flow (cynotic)
The classic sign is Cynotic that doesn't respond with O2.
Polycythemia will occur and increase risk for embolism in cerebral or lungs. |
Tetralogy of fallot (TOF)
Pulmonic stenosis (also a heart obstruction)
Tricuspid Atrasia (TA)
Transposition of the Great arteries is MIX of both because the left ventricle aggressively pumping blood in the lungs. Loud murmurs
Those usually symptomatic unlike ⬆️ pulmonary blood heart condition. |
|
|
|
Patent ductus arteriosus (PDA) ⬆️ pulmonary flow Acynotic |
S/S: dyspnea, retraction, tachypnea, bounding pulse. HEART SOUND: machine-like murmur in both systole and dystole. COMPLICATION: CHF, hepatomegaly. Dx: echo & XR of large left ventricle and PDA.
|
|
|
|
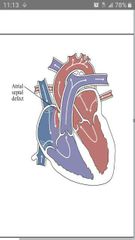
Atrial septal defect (ASD) ⬆️ Pulmonary flow
Acynotic
Usually asymptomatic and kids may grow out of it within 4 years. |
S/S for large defect: 1. easy tiring because most of the blood escape from the left atrim to right atrium and barely any blood reach the left ventricle. 2. Poor growth because low circulatory blood flow but it's highly oxygenated. 3. CHF s/s
Heart sound: soft systolic murmur in pulmonic area which is the blood flow escaping the left atrium.
Dx echo of dialate R ventricle |
|
|
|
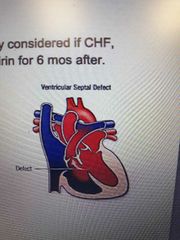
Ventricle septal defect (VSD) ⬆️ PULMONARY FLOW
Acynotic
Usually Asymptomatic
Usually will close alone |
S/S from large defect: CHF and at risk for pulmonary infections.
Heart sound: systolic hollow murmur at 3/4th intercostal at the defect as blood escaping.
Dx: CXR shows large heart and increase pulmonary vascular marking due to over stretch from too much blood. |
|
|
|
The traditional cardiac s/s in children.
1. CXR allow to see size & pulmonary blood flow patterns, lungs infection. 2. Echo to see enlargement of chambers and valve. 3. MRI show vascular on the heart. |
Poor feeding specially infant
Tachypnea and dyspnea
Failure to thrive/poor growth
Tachycardia
Activity intolerance
Sleep more or frequent rest
Swelling of the eyes and feet.
|
|
|
|
Tet spells
Happen in Tetralogy of fallot and cause pt to be severely cyanotic |
It occur after crying, exercise, or when agitated. It is due to decrease systemic resistance and pulmonary blood flow. So toddler squat to increase peripheral vascular in order to shunt the blood from right to left.
S/S: severe cyanosis, tachypnea, SOB, LOC/faint. |
|
|
|
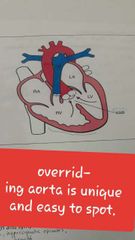
Tetralogy of fallot 1. Ventricle Septal defect 2. Pulmonary stenosis 3. R ventricle enlargement 4. Overriding aorta between both ventricles and receive little deoxygenated blood from right ventricle. |
Pulmonic stenosis increase pressure in the right ventricle causing a RIGHT TO LEFT shunting.
Deoxygenated blood mix go to systemic due to overriding aorta and VSD. Unlike PDA, VSD, and ASD that have only oxygenated blood and not mix. PDA, VSD, and ASD only have oxygenated blood.
S/S: poor growth, clubbing, activity intolerance (tet spell), SOB in tet spell. Toddlers squat to increase vascular resistance and thus decreasing right - left shunt. polycythemia, tet spells, metabolic acidosis.
Heart sound: systolic murmur in the pulmonic area like ASD but not soft.
Dx: CXR shows boot shaped heart. Decrease pulmonary marking unlike VSD. EKG shows right ventricle hypertrophy. Echo shows obstructed pulmonary artery.
Paliative surgery with shunt untill they old enough or stronger. Endocarditis prophylaxis. |
|
|
|
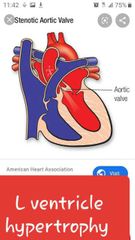
Aortic stenosis
Usually Asymptomatic |
L ventricle hypertrophy to force blood out to systemic.
S/S: weak peripheral pulse (like coarctation in LE), CP unlike coarctation obstruction that after the coronary arteries. dyspnea after excercise, fainting in severe case.
Heart sound: systolic murmur in aortic area.
Dx: CXR shows prominence of L ventricle and EKG show hypertrophy.
Prostaglanding to maintain PDA in newborn until it fix. |
|
|
|
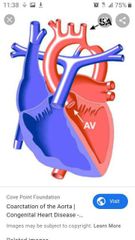
Coarctation of the aorta
Similar to aortic stenosis and also ASYMPTOMATIC.
It grow by itself
|
Stenosis near the ductus arteriosus or peft subclavian.
S/S: lower BP and weaker pulse in LE. Weakness & pain in the legs after run or walk. Cynotic in LE in severe case. Traditional: poor feeding, failure to thrive.
Heart sound: lound S2 and sytolic murmur.
Dx: CXR shows cardiomegaly and pulmonary venous congestion from back up blood. Indentation is shown in CXR. |
|
|
|
CHF SNS cause tachycardia. Reeuce blood flow to kidney. Myocardium stretch to help. Still can't maintain cardiac output. After all that, edema or pulmonary congestion occur. |
Frequent resp. infection common in infant while dyspnea more common in older children.
NI: check digoxin level 6h after administration. 0.8-2 is normal range. 25-30mcg/kg. Don't ever redose if child spit or try to cath up miss dose.
Suspect CHF if infant feed for longer than 30 min. Digoxin need 90 pulse in infant and 70 pulse in younger children.
Maintain oxygenation and myocardial function with digoxin. prevent tet spells. Adequate nutrition. Calories count, more calories, and I/O. Promote rest and don't feed for more than 35 min. Use NG if necessary. Worsen in feeding habbit indicate worsen heart. Teach parent on toxic effect on digoxin and how to take pilse before. Watch for feeding habbit, lethargy, dyspnea, swelling eyes and extremities.
S/S: dyspnea, tachycardia, pallor, nasal flaring, cyanosis, cough, crackle, S3 gallop. CO drop in heart failure so BP go down. CO go up in sepsis to compensate for vasodilation. Despite increase in CO, bp still drop. |
|
|

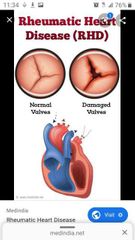
Rheumatic Heart Defect Damege of the heart valve from autoimmune response. |
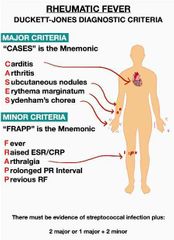
1-3 weeks of an untreated strep throat. That's the hallmark sign to suspected RHD.
New murmur with chest pain (carditis) and strep last week. Joint inflammation HEAT. Erythema marginatum- rash with pink macules and blanching in the middle. SOB. syndenham- aimless movement of extremities.
ASA give to kids in this case. Antibiotics and prophylaxis for 10 years or untill 21. Throat culture. Bed rest. Limited walk at home only. Temp Q4h. Family throat culture.
|
|
|

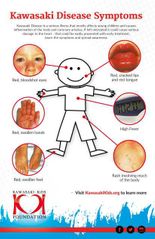
Kawasaki disease Systemic vascular inflammation of small and medium arteries specially coronary arteries.
Leading cause of heart disease in children, specially 5 years old. |
Phase 1. 1-2 weeks. Acute high fever, IRRITABILITY, red throat, swellen hands & feet, lymphadenopathy, rash on trunk and perineum, red eyes, diarrhea, hepatic dysfunction.
Phase 2. 2-4 weeks. End of fever. Skin problem start with fissures & cracked lips and peeling (desquamation) of fingers and toes. JOINT PAIN.
phase 3. 4-8 week. All s/s is almost disappears with grooves nail. ABD pain, diarrhea, vomit. Similar to strep and measles.
Dx: high spike fever for >5 days. Echo of coronary abnormalities. High WBC. Treatment: IV immune Globulin but postpone LIVE vaccine for 11 months. High dose ASA for the anti inflammation effect.
|
|
|
|
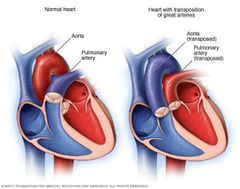
Transposition of the great arteries. |
Switching the aorta and pulmonary artery.
S/S: Tachycardia, feeding intolerance, failure to thrive, fatigue, and CYNOSIS. will lead to CHF.
CXR: egg-shaped heart with enlarged L ventricle and increase pulmonary vasculature as a result the L ventricle forcing blood in it. ECHO shows abnormal position of the arteries. CBC shows polycythemia. Prostaglandin E1 to get PDA.
|
|
|

Infective Endocarditis Injury in the endocardium cause cloting in the affected area. Bacteria in the blood adhere to it. |
As the bacteria multiplies in the endocardium, it attracts platelets causing a VEGETATION. It can break off causing as an embolus. as an embolus.
Maybe associated with a defect, rheumatic disease, CVC line, heart surgery, or IV drug use. Most at risk are bicuspid surgery and cardia surgery.
S/S: low fever, fatigue, weakness, weight loss, JOINT/MUSCLE PAIN, new murmur, splenomegaly, petechiae, OSLER NODE, JANEWAY LESIONS.
Blood culture & ECHO shows infection and damage.
|

|
|
|
Tricuspid atresia Tricuspid valve absent and undeveloped (hypoplastic) right ventricle. |
S/S: tachypnea, cyanosis, palor, trachycardia, diaphoresis, seuzure, LOC.
prostaglandin E1 reopen the ductus arteriosus.
|

|
|
|
TOF and ASD heart sound |
TOF lound murmur over pulmonic area
ASD soft murmur over pulmonic area
Arotic stenosis is murmur over aortic area. Coarctation is lound S2 & murmur.
|
|

